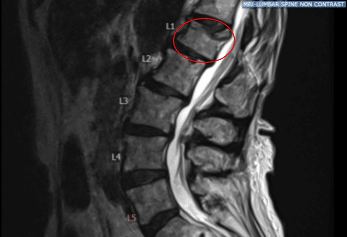
Case Study: L1 kyphoplasty with bipedicular access
An extremely pleasant patient with a past medical history of osteoporosis presenting with intractable back pain and a wedge compression deformity of the first lumbar vertebra. The physical exam showed tenderness of the right paraspinal region at L 5 and tenderness of the left paraspinal region at L 5.
Pre-Operative X-ray
Preoperative MRI showed hyperintense STIR signal change in L1 vertebra. After extensive discussion and the failure of nonoperative management, they were taken to the operating room for a L1 kyphoplasty procedure for pain control.
The risks, benefits, alternatives were extensively explained to the patient. Risks included failure of pain to improve with a technically successful and complication-free surgery, bleeding, infection, methyl methacrylate extravasation causing a neural element compression and new onset neurological deficits as well as pulmonary embolism. The rare potential risks for conus medullaris injury was also explained to the patient.
The operational procedures performed on the patient were L1 kyphoplasty with balloon tamps and bipedicular access, injection with methyl methacrylate, Intraoperative fluoroscopy with immediate neurosurgical interpretation and L1 vertebral body bone biopsy.
The patient was identified by two separate name markers and brought into the operating room. General endotracheal anesthesia was induced. All appropriate lines were placed by the department of anesthesiology. The patient was then positioned prone on an open Jackson table with chest and hip bolsters. Care was taken that the eye sockets, ulnar and peroneal prominences were carefully padded.
At that point, fluoroscopy was assembled and a starting incision was marked up 4 cm off of midline in line with L1 pedicles. The starting stab incisions were kept less than 1 cm in overall length. The area was sterilely prepped and draped in the standard neurosurgical sterile fashion. Members of the operating team went to wash their hands.
Following draping, a final time-out was carried out identifying the patient and the nature of surgery to be performed, the level of the spine to be operated on, respective roles and responsibilities of all associated team members following completion of successful time-out, the stab incisions were infiltrated with 1% lidocaine with epinephrine as well as 0.25% Marcaine with epinephrine and opened with a #15 blade to commence the case.
Dissection was carried down to the level of the dorsal lumbosacral fascia using monopolar electrocautery. The Kyphon one-touch introducer needles were then used to cannulate the bilateral pedicles at L1 under biplane fluoroscopy with care being taken to not breach the medial border of the L1 pedicle until the vertebral body of L1 had been confirmed entered on lateral fluoroscopy.
Once both Kyphon one-touch introducer needles were completely placed, the inner stylets were withdrawn through the cannula. An L1 vertebral body biopsy was obtained using the biopsy aspiration trocar with a 3 cc syringe attached. This was sent off to pathology for permanent specimens.
A hand drill was then used through both cannulae in order to create tracts for the Kyphon balloon tamps. The hand drill was withdrawn. The balloon tamps were inserted and inflated to 200 PSI bilaterally with care being taken to restore the end plate. A defect was noted in the superior L1 endplate corresponding to preoperative MRI imaging with balloon inflation.
The balloons were taken down. Methyl methacrylate was mixed and allowed to harden to exact viscous consistency and the methyl methacrylate was injected bilaterally through the pedicular access with care being taken to fill the screw defect at L1 with slight extension upwards into the T12-L1 disk space but no extravasation either anteriorly into the venous plexus or posteriorly into the canal.
Approximately 5 cc of methyl methacrylate were injected overall with good height restoration and excellent placement across midline and creation of bony support with an L1 vertebral body proper. Once the methyl methacrylate had been injected and allowed to hardened to the desired consistency, the inner stylets of the Kyphon introducer nails were withdrawn and maintained in place for two minutes.
Final AP and lateral radiographs indicated excellent methyl methacrylate position with minimal to superior extravasation of the T12-L1 disk space. Accordingly the Kyphon one-touch introducer needles were withdrawn.
The stab incisions were copiously irrigated with antibiotic impregnated saline and final hemostasis was achieved with Monopolar cautery. Closure was then carried out with bilateral #3-0 Nylon sutures and vertical mattress session which were secured in place to reapproximate the epidermis.
Dermabond was applied to the skin edges and the nylon sutures were then withdrawn following incision with a #11 blade after the Dermabond had been allowed to harden.

Fluoroscopic Imaging
The patient was then reversed back into a supine position and general endotracheal anesthesia was reversed, endotracheal tube was removed. The patient was found to be in the same condition in which they entered the operating room, which is to say awake, alert, following commands briskly with full motor power in her lower extremities.
I attest that I was attending neurosurgeon of record and performed the entirety of this case myself with the aid of my co-surgeon throughout. We performed both aspects of this case equally operating in a bipedicular fashion and we directly supervised and interpreted all fluoroscopic imaging together.
The patient initially followed up in one week after the surgery and then continued following up in our office 4, 6, and 8 weeks. In their last office visit they stated they were able to continue daily activities with little to no back pain. They also agreed to continue physical therapy.
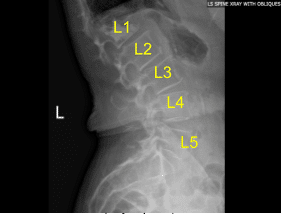
Postoperative Lumbar Spine X-ray Status Post Vertebroplasty of L1 Sagittal View

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
