Case Study: L3-S1 Laminectomy and Fusion
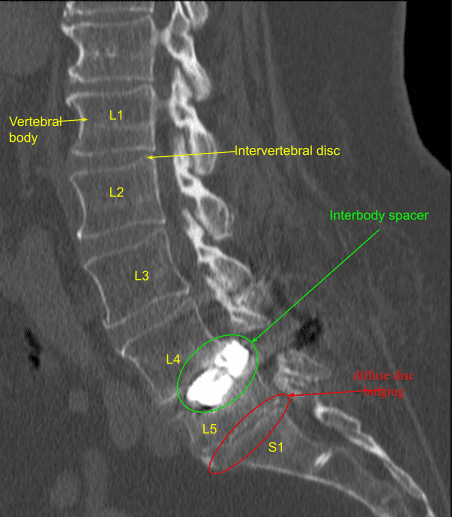
A patient presented to our clinic with a history of at least two other lumbar spine surgeries with recurrence of severe low back pain, inability to ambulate and imaging showing severe adjacent segment stenosis as well as hardware malfunction, mispositioning and pseudarthrosis.
Surgery was recommended to decompress and stabilize the lumbar spine. The risks, benefits, alternatives and potential complications of the surgery were explained to them. All of their questions were answered until no further issues were raised and they provided written informed consent which was placed in the chart.
The patient was brought to the operating room. Their identity was verified. Surgical timeout was performed. General anesthesia was induced. They were intubated by the Anesthesia Service. Respiratory and cardiac monitoring leads were placed. Neuromonitoring leads for somatosensory evoked potentials and EMG were placed.
They received preoperative prophylactic IV antibiotics as well as IV tranexamic acid. They were positioned prone on a Jackson Relton-Hall frame with all pressure points carefully padded. Lumbar area was cleaned with chlorhexidine.
A midline incision was demarcated as per their previous scar with an extension rostrally. Skin was sterilized with DuraPrep solution. Sterile drapes were placed in the usual manner. 1% lidocaine with epinephrine was infused along the skin line.
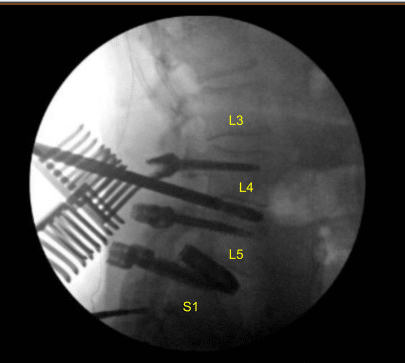
The skin was opened with a #10 blade scalpel. Hemostasis was obtained with bipolar electrocautery. Bovie monopolar and Cobb elevators were used to carry the incision down through the subcutaneous tissue and scar tissue and exposed posterolateral spine from L3 to L5 exposing the previous indwelling hardware at L4-5. Self-retaining retractor was placed. Previous locking caps, rods and pedicle screws were removed.
The L4 pedicle screws were loose. We then placed the neuronavigation array to the right superior iliac crest via two stab incisions and Schanz pins were placed. Neuronavigation array was fixed rigidly.
Intraoperative CT scan was obtained. Data was transferred to the neuronavigation computer. Accuracy was verified. Stereotactic image-guided neuronavigation techniques were used to reposition and replace the new pedicle screw at L4 on the right side in a proper position.
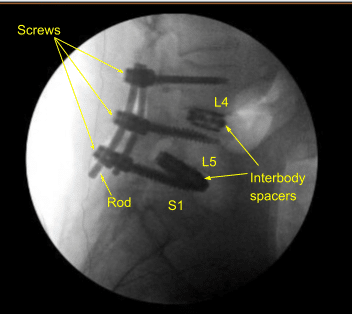
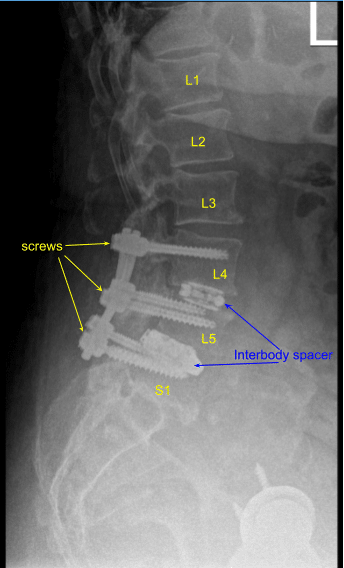
The remaining pedicle screws on the left at L4 and bilateral L5 were replaced with new pedicle screws slightly upsized. A tighter fix was achieved. Next, we placed the new pedicle screws at L3 bilaterally decorticating with electric high-speed drill, cannulating with navigated pedicle finder, palpating for breaches, measuring the depth, under tapping by 1 mm and placing the pedicle screws in a usual manner without difficulty. Neuromonitoring signals were stable.
Next, an intraoperative CT scan was obtained showing the correct position of all the screws. Next, we performed L3-4 laminectomy using Leksell rongeurs collecting autograft for morselization for arthrodesis, exposing hypertrophic ligamentum flavum which was retracted in a piecemeal fashion with Kerrison rongeurs.
Bilateral facetectomies were performed. TLIF was performed retracting the thecal sac and nerve root medially with the nerve root retractor. TLIF was performed from the patient’s right side. Annulotomy was performed with a #15 blade scalpel after coagulating the epidural veins with bipolar electrocautery. Discectomy was performed with sequential paddle shavers and pituitary rongeurs. Endplates were prepped for arthrodesis with curettes and rasps.
Interbody spaces were irrigated clear, packed with morselized autograft from the decompression as well as demineralized bone matrix allograft, and then an expandable titanium interbody spacer was placed under sterilely draped fluoroscopic guidance in AP and lateral views into proper position. Neuromonitoring signals were stable. Bilateral L3-4 neurolysis was performed with Metzenbaum-Penfield technique and confirmed with nerve hook circumferentially.
The wounds were irrigated clear. Precut-precontoured titanium rods were selected and placed across the tulips from L3 to L5 bilaterally and secured with locking caps which were all final tightened with a torque and anti torque device.
Bilateral transverse processes were decorticated with electric high-speed drill from L3 to L5 and morselized autograft and allograft mixed with bone marrow aspirate from a separate incision at the superior iliac crest was all combined for the posterolateral arthrodesis graft as well as bone morphogenic protein. No CSF leak or durotomy was appreciated after inspecting the thecal sac.
Vancomycin powder was applied liberally. A medium size Hemovac drain was tunneled in a subfascial manner and secured to the skin with a 3-0 nylon suture. Interrupted 0 Vicryl sutures were placed in a watertight fashion to reapproximate the fascia and 2-0 Vicryl sutures for the subdermal layer.
Exparel long-acting local anesthetic was infused into soft tissues for postoperative analgesia.
More vancomycin powder was applied in the subdermis. Skin was reapproximated with surgical staples, cleaned and dried sterilely, and dressed with Mepilex bacteriostatic dressing. Hemovac canister was applied to suction.
The patient was then turned supine on the cart, extubated uneventfully and transported to the recovery room in stable condition. At the end of the case, all sponge counts, needle counts and instrument counts were correct. The patient tolerated the procedure well.
The patient initially followed up in two weeks after the surgery and then continued following up every 4 weeks. In their last office visit the patient was able to ambulate and showed signs of improvements with back pain.
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.

