Case Study: Revision Lumbar Spine Surgery In A Patient
With Adjacent Segment Degeneration And Radiculopathy
The 66-year-old male patient was in our office referred by her PCP, with complaints of lower back pain for many years. The pain was improved with back surgery (L3-5 PSF) two years ago with the use of BMP but the pain has come back.
The pain was moderate to severe in intensity. The patient described the pain as sharp and burning located in the lower back. The pain was intermittent and did not disturb sleep. The pain was associated with numbness, radiating pain, and limping. The radiation and numbness are more on the right side, back of boththighs, buttocks, knee, and leg. His leg pain was more than the back pain.
Walking made the symptoms worse. The grocery cart sign was positive. Lumbar canal stenosis (LCS) symptoms were present. The distance was 100 yards. Rest, heat, ice, lying down, bending forwards made the symptoms better.
He was a former smoker having quit 12 years ago and a social drinker. Her current medications included metformin, lisinopril, metoprolol, and atorvastatin. He had a posterior spinal fusion surgery 2 years ago.
The patient was calm, conscious, cooperative, and well oriented to time, place and person. Upon examination of the lumbar spine, the patient was tender to palpation over the paraspinal musculature as well as over the spinous processes in the L5-S1 region and had no crepitus with range of motion.
The old surgical incision was healed well without induration, erythema, or discharge. The patient had a limited range of motion of the spine due to discomfort. He had a positive straight leg raise test on the right side.
There was no tenderness to palpation over the trochanteric bursa and hip. There was no soft tissue swelling and ecchymosis. The patient had a full range of motion of the hips. The hips were stable on the examination. They are neurovascularly intact distally. There are no erythema, warmth, or skin lesions present.
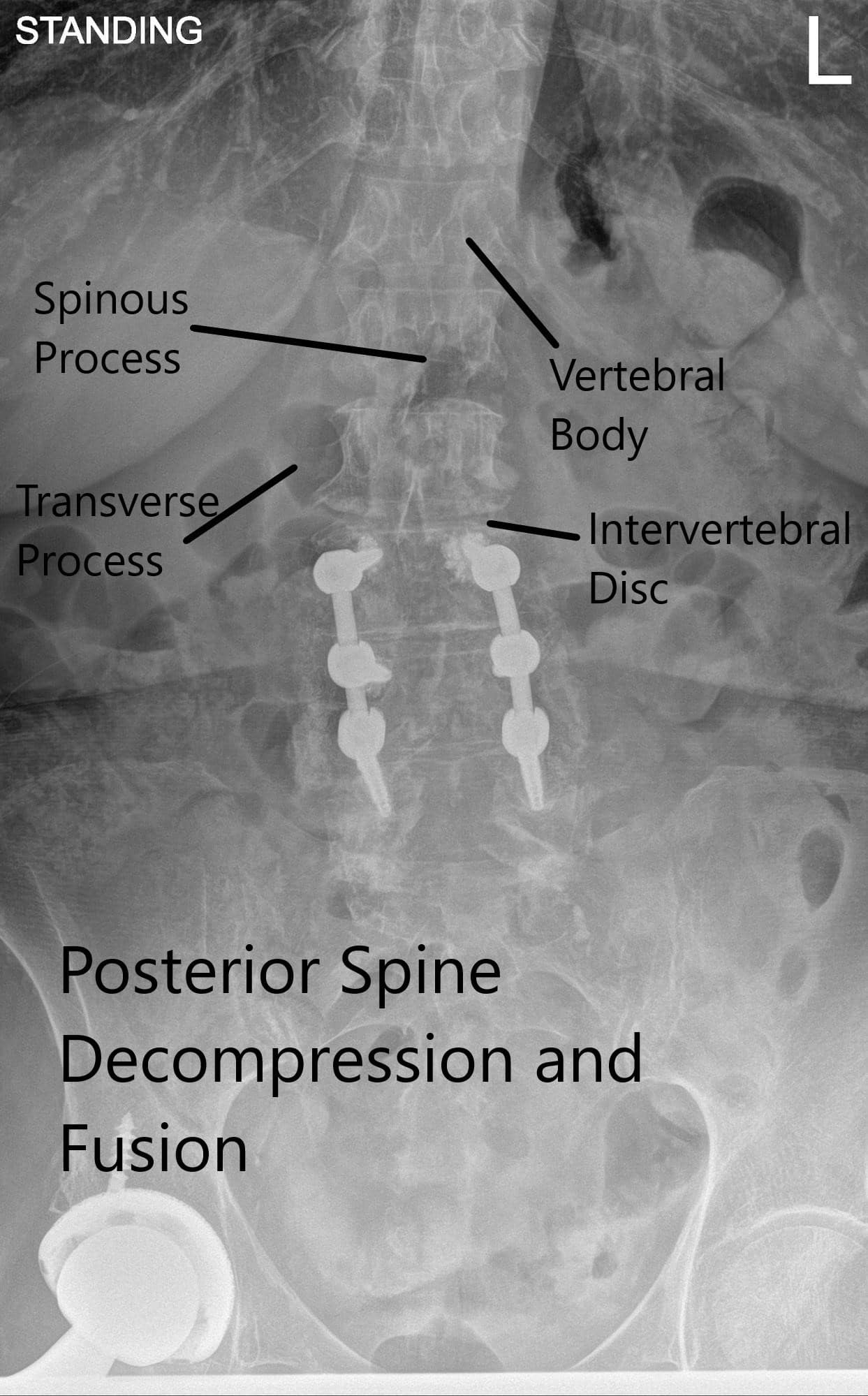
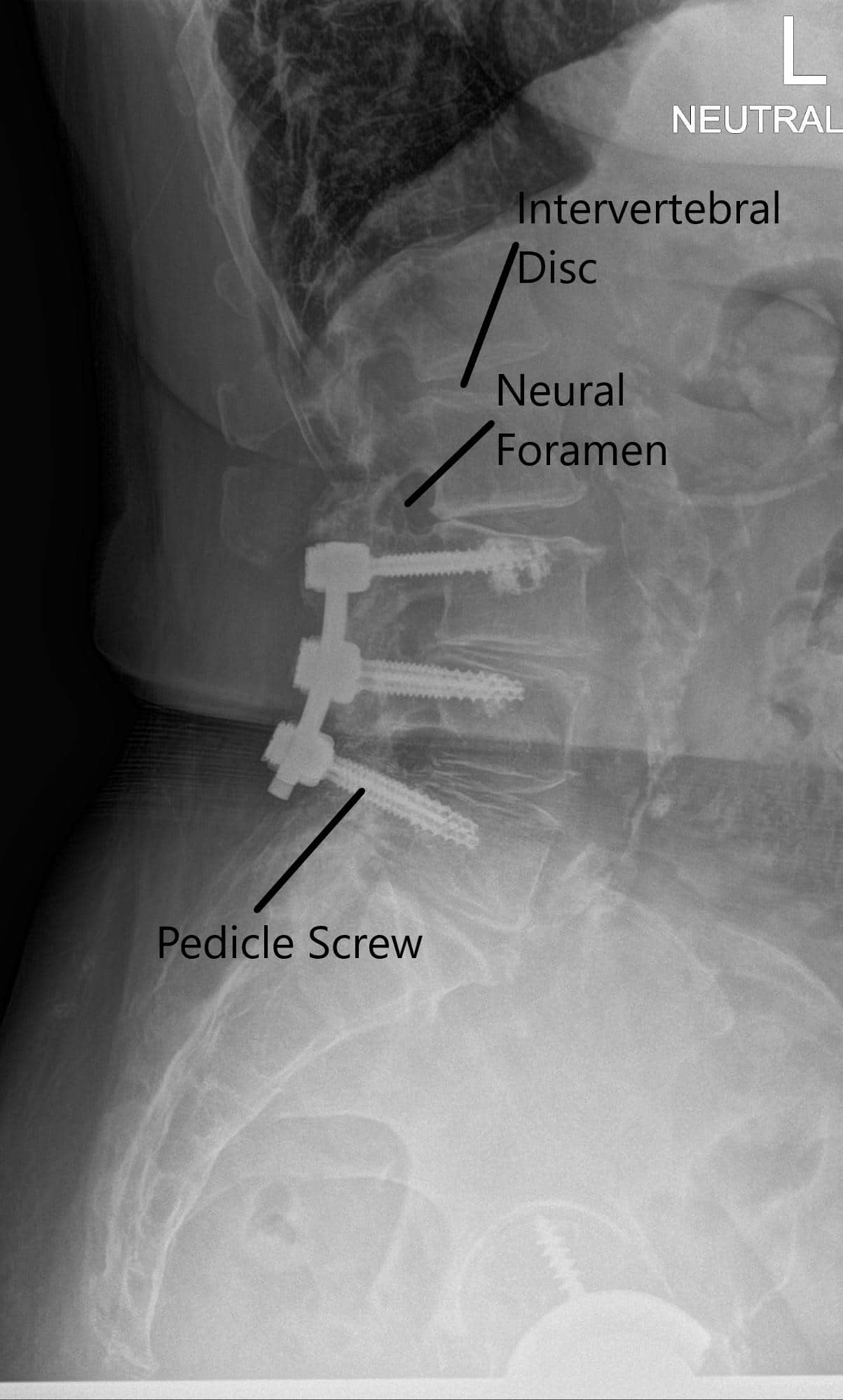
X-ray of the LS spine in AP and Lateral views.
CT scan signs of early screw loosening are seen. However, signs of bony ankylosis from L3-5 are also present. Degenerative spinal stenosis at L2-3 was present and was relatively unchanged since the most recent prior exam in 2018 but demonstrates progressive stenosis over the sequence of scans. MRI showed adjacent segment disease at L2-3 and L5-S1 with nerve root compressions.
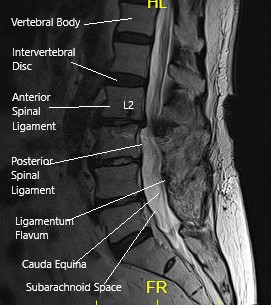
MRI of the LS spine in sagittal section.
We discussed risks and benefits of surgical treatment including infection, bleeding, injury to adjacent nerves and vessels, worsening of pain, injury to the dura and CSF leak, need for repeat surgery, need for the possibility of further degeneration needing fusion in the future, systemic problems like cardiac, neurological, pulmonary events, blood clots among others. The patient understood and signed the informed consent for lumbar spine surgery.
The patient was taken to the operating room where general anesthesia was induced and the patient was intubated. SSEPs and EMGs were set up by the neuromonitoring team. A Foley was passed preoperatively.
Preoperative antibiotics in the form of 2 g of Ancef was given before the surgery. The patient was flipped prone onto its four-post Jackson table and well padded on bony prominences. The lower back was prepped and draped aseptically in the usual fashion.
A timeout was called before the surgery was started. The prior incision was marked and the area instilled with Local anesthetic. The incision was given along the upper 3 cm of the previous incision, extended proximally by two more centimeters. With sharp and blunt dissection the fascia was reached.
The fascia was cut along the line of incisions and the spinous process of L2 was reached. With the use of monopolar cautery, bilateral dissection on either side of the spinous process was done to expose until the facet joints. The inferior part of the lamina was exposed. C-arm was brought in to confirm the level. The inferior spinous process was removed using the Horsley bone cutter.
The inferior lamina was removed using a combination of the electric drill with matchstick burr and Kerrisons up to the level of the insertion of the ligamentum flavum. All the thickened ligamentum flavum was excised. Foramen of L2 nerve root was reached above the pedicle of L2.
The foraminotomy of L3 was done bilaterally between the pedicles of L2 and L3 using Kerrison punches. The satisfactory decompression was achieved. Following that the scar of previous surgery was encountered and removed with the use of a combination of curettes and Kerrison punches. Bilateral foraminotomies of L3-4 were performed subsequently.
Hemostasis was achieved and the wound was irrigated and packed. Now, an incision was given on the inferior part of the previous incision and extended 2 cm distally. With sharp and blunt dissection and use of hemostasis, the bone was reached.
An x-ray was done and we were found to be on the right facet joint. It seemed that the patient’s scoliosis as well as the previous scar was more on the right side. We developed the plane between the facet and spinous process and cleaned up the soft tissues. Right laminotomy of L5 was performed using an electric drill and Kerrison punches.
The nerve root of Right L5 and S1 were followed into the foramen. Foraminotomy of L5 was performed using Kerrison punches. A thorough decompression of L5 and S1 nerve roots was performed. Finding it all satisfactory. Final pictures were taken and saved.
Hemostasis was achieved. Wounds were thoroughly irrigated. The nerve roots epidural space was instilled with 5 mg of Duramorph mixed with 80 mg of Depo-Medrol. One gram of vancomycin was put after thorough irrigation.
The closure was done by the plastic surgeon. The patient was turned supine on the operating bed and extubated. Post Op examination showed intact neurovascular status. The patient was moved to the postoperative care unit in a stable condition.
Patient did well after the surgery. Her leg pains were resolved. He did have residual back pain which was being treated conservatively with Physical Therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
