Interspinous Process Spacer
Interspinous process spacer decompression surgery is a minimally invasive spine surgery used to treat conditions such as spinal canal stenosis. The surgery involves placing a metallic/plastic spacer in between the spinous process of the adjacent vertebrae. The surgery benefits the patients via decompressing the spinal nerve roots and the thecal sac.
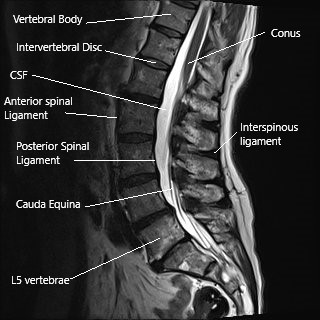
Anatomy of Spine
The spinal cord runs in the vertebral canal and gives numerous branches (spinal nerves) as it travels down the canal. The vertebral canal is formed by the vertebrae stacked upon each other. The lamina creates the vertebral canal’s roof, and the vertebral body forms the floor.
The spinous process is a bony projection at the back of the vertebrae. The projections may be felt under the skin as you run your hand in the lower back’s midline. The spinous processes provide stability and help in the backward movement of the spine.
Spinal Stenosis
In spinal canal stenosis, the space available for the neural tissues in the vertebral column decreases. Usually, an age-related degenerative process triggers the changes leading to stenosis. The intervertebral disks lose their fluidity with age causing decreased disk height which may result in degeneration of the facet joints that support the adjacent vertebrae.
The facet joint and disk degeneration may cause the formation of bone spurs and thickening of the ligamentum flavum as the body tries to re-align the vertebrae. The bone spurs and thickening of ligaments may narrow the vertebral canal and the neural foramen leading to compression.
The compression of the spinal nerve roots and the dural sac may cause symptoms of radiculopathy and neurogenic claudication. The patients may experience shooting pain down the buttocks, thighs, leg, or feet depending upon the nerve compressed. The pain may accompany numbness and tingling sensation along the region of the involved nerve. In severe cases, there may be a weakness of the muscles of the lower extremities or loss of bowel and bladder control.
Neurogenic Claudication
Symptoms of neurogenic claudication include pain in the buttocks, thighs, groin, or legs on walking. The symptoms get worse on walking downhill and relieved by bending forward. The symptoms occur due to the narrowing of the vertebral canal and the neural foramen on the backward movement of the spine.
As the spine bends backward, the ligamentum flavum buckles to compress the dural sac, and the capsule of the facet joints press on the neural foramen. The resulting compression of the dural sac and spinal nerves may cause symptoms due to decreased blood supply to the involved nerves.
Management
The initial treatment of spinal stenosis is conservative that may involve the use of physical therapy, pain medications, alternative medicine, and epidural/nerve block injections in the spine. The patients who have not benefited from conservative treatments for six months may be candidates for decompression surgery.
Laminectomy
Lumbar decompression surgeries usually involve removing bony or soft tissue structures to widen the vertebral or the neural foramen. Laminectomy, laminotomy, or laminoplasty are the surgeries usually performed to decompress the involved segment. The surgery may be accompanied by lumbar fusion surgery to provide rigid stabilization to the spine.
Interspinous Process Spacer
Interspinous process spacer surgery decompresses the involved segment with dynamic stabilization. The surgery is usually performed with a minimally invasive technique that involves tiny incisions at the back.
A local or general anesthesia may be given to the patient to numb the involved area. Under fluoroscopic guidance, the surgeon introduces small tubes to reach the interspinous area and gradually introduces increasing diameters of tubes to separate the tissues. The spacer is then introduced through the tubes and turned to its proper position. The incision is then closed in layers, and the skin incision is closed with one or two sutures.
Benefits of Interspinous Process Spacer
Interspinous process spacer limits the backward bending of the spine. The symptoms of canal stenosis and neurogenic claudication are position-dependent. The backward motion of the spine exacerbated the symptoms. The spacers prevent the backward movement and thus result in relief of symptoms.
The rigid fixation offered by fusion surgeries often results in limitation of motion of the spine. The interspinous process spacers do dynamic stabilization by allowing limited forward bending, side bending, and twisting movement.
The surgery also allows the patients to go home the same day of the surgery. The majority of the interspinous process spacers may be inserted in an outpatient setting. There is little postoperative pain as the incisions used are very small. The back muscles are also separated and not cut as compared to the traditional fusion surgeries.
The distraction of the spinous processes leads to the opening of the neural foramen, thus alleviating canal stenosis symptoms. The decompression achieved is dynamic as opposed to lumbar fusion surgery.
Potential complications
Being a minimally invasive surgery, the risks of complications is minimal, but there may be potential complications associated with interspinous process spacers. The spacer may dislodge and move out of its place. The interspinous process spacer may break or fracture the spinous process. There may be inadequate relief of symptoms, or additional surgery may be needed.
Contraindications
The interspinous process spacers are not indicated in patients with motor and sensory weakness associated with nerve compression. The patients with bowel and bladder incontinence who may have cauda equina syndrome are not candidates for spacers as they may require immediate open decompression. Also, patients with spine infection and osteoporosis are not candidates for interspinous process spacer.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.