Case Study: Revision L4-S1
Transforaminal Interbody Fusion (TLIF)
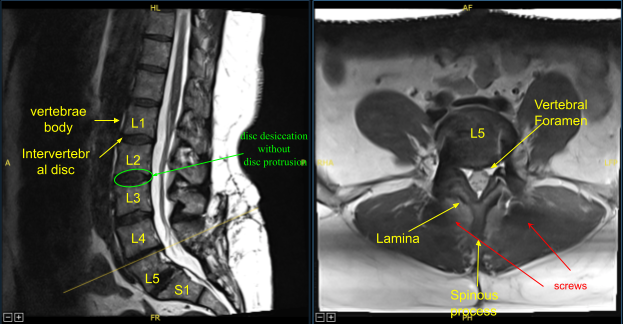
The patient presented to the office status post two previous lumbar surgeries performed by another provider including L5-S1 discectomy and L5-S1 TLIF. They developed recurrent back and lower extremity pain and symptoms and imaging showed adjacent segment disease with L4-L5 disc herniation, stenosis, as well as pseudarthrosis at L5-S1.
Surgery was recommended to decompress and stabilize their lumbar spine after she had failed conservative treatment measures. Risks, benefits, alternatives, and potential complications were explained to them. All their questions were answered until no further issues were raised and she provided written informed consent which was placed in the chart.
The patient was brought to the operating room. Their identity was verified. General anesthesia was induced. They were intubated by the anesthesia service. Respiratory and cardiac monitoring leads were placed. Neuromonitoring leads for somatosensory evoked potential and EMG were placed. She received preoperative prophylactic IV antibiotics.
They were positioned prone on the Jackson Relton-Hall frame. All pressure points were carefully padded. Lumbar area was cleaned with chlorhexidine and a previously made incision was demarcated. Skin was sterilized with a DuraPrep solution. Sterile drapes were placed in the usual manner. 1% lidocaine with epinephrine was infused along the incision line.
The skin was opened with a 10-blade scalpel. Hemostasis was obtained using bipolar electrocautery and Bovie monopolar; and Cobb elevators were used to carry the incision down sharply to divide the fascia and expose previous spinal instrumentation at L5-S1 as well as the L4 lamina and bilateral L4 transverse processes. Self-retaining retractors were placed. Fusion was explored and was found to be inadequate and confirmed pseudoarthrosis.
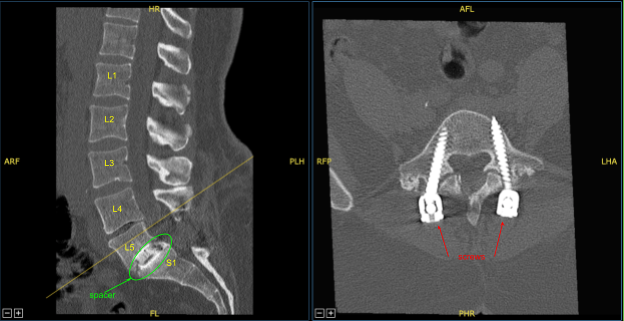
Locking caps at L5 and S1 were removed. The rods were removed. The screws were checked and were found to be tight and therefore were left in place. Next, the fixed neuronavigation arrays for the right posterior-superior iliac crest with two Schanz pins. Sterilely draped the patient to obtain the CT scan.
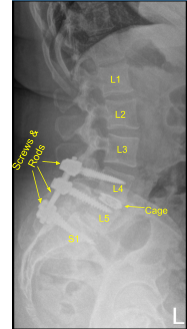
Transferred the data to the neuronavigation computer and image guided neuronavigation techniques were utilized for placement of the bilateral L4 pedicle screws which was accomplished by decorticating electric high-speed drill, cannulating the pedicles with the navigated pedicle finder, sounding for breaches, and measuring the depth using 5.5-mm tap and placing 6.5×45 mm titanium pedicle screws under neuronavigation guidance without difficulty. Neuromonitoring signals were table throughout.
Next, we performed L4 laminectomy, bilateral facetectomy with Leksell rongeur, electric high-speed drill under continuous irrigation and Kerrison rongeurs resecting ligamentum flavum in piecemeal fashion and exposed thecal sac, decompressed it circumferentially and neurolyzed bilateral L4 nerve roots with Metzenbaum Penfield technique and confirmed with nerve hooks. Epidural bleeding was controlled with bipolar electrocautery and Surgiflo hemostatic matrix.
The thecal sac was retracted medially towards the right side with nerve root retractor. Annulotomy was performed with a 15-blade scalpel. Discectomy was performed with sequential pedal shavers and pituitary rongeurs. Endplates were prepped for arthrodesis with scrapers. We collected morselized autograft, bone shavings, and morselized resected spinous process and lamina.
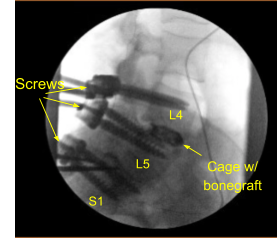
Demineralized bone matrix allograft was placed into the interspace and then titanium expandable interbody device was placed under fluoroscopic guidance after sterilely draping the C-arm unit. AP and lateral imaging showed correct positioning and then the cage was expanded to the proper fit and the subsequent x-ray showed good positioning both in the midline and anteroposterior.
Next, a new CT scan was obtained, which showed correct positioning of the new pedicle screws and interbody spacer. Bilateral transverse processes of L4, L5, and lateral ala were decorticated for arthrodesis. Pre-cut, pre-contoured rods reflected and placed across the tulips from L4 to S1 and secured with locking caps and finally tightened with the torque and anti-torque device.
Morselized autograft and allograft were placed into lateral gutters from L4 to S1 for the arthrodesis. Wound was irrigated copiously throughout the procedure. Vancomycin powder was applied. Closure was performed by a plastic surgeon.
Following that, the patient was then turned supine on the cart, extubated uneventfully, and transported to the recovery room in stable condition. At the end of the case, all sponge counts, needle counts, and instrument counts were correct, and the patient tolerated the procedure well with 200 cc estimated blood loss and no complications.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
