Case Study: Management Of Cauda Equina Syndrome (CES) in a 60-Year-Old Female With L2-L4 Critical Lumbar Stenosis And Acute Leg Weakness
A 60-year-old female was admitted to the hospital for intense back pain and leg pain with associated right leg weakness. She had a recent history of her legs giving out suddenly. The workup in the ER included an MRI which suggested critical stenosis from L2 – L4. The patient was having urinary symptoms, acute leg weakness as well as numbness in the groin area and in the lateral parts of his legs bilaterally.
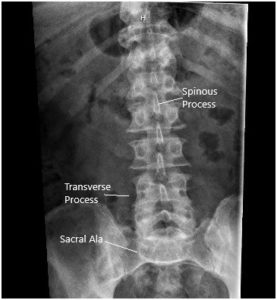
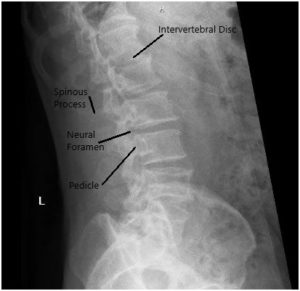
X-ray in AP and Lateral views demonstrated narrowing of the L5-S1 Disc
MRI suggested Ligamentum flavum hypertrophy contributing to severe central spinal stenosis at L2-L3. There was mild to moderate narrowing of the left neural foramen. There was a severe narrowing of the right neural foramen with effacement of the exiting right L2 nerve root due to a far lateral disc herniation.
At L3/4 there was a disc bulge and a facet and ligamentum flavum hypertrophy contributing to severe central spinal stenosis. There is mild to moderate narrowing of the bilateral neural foramina.
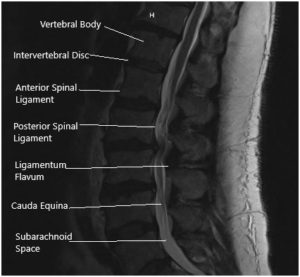
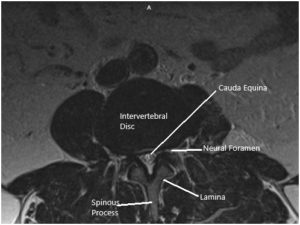
MRI of the Lumbosacral spine in sagittal and axial sections.
Her past medical history was significant for hypertension, thyroid disease, and diabetes mellitus. She had previously undergone anterior cervical decompression and fusion 7 years ago. She was currently on Lipitor, Folic acid, Levothyroxin, and Metoprolol.
These clinical findings correlated with his imaging findings and given the severe neurological compromise and cauda equina syndrome, we offered emergent surgery for the patient. The patient had a significant medical history and immediate stabilization was initiated. The patient understood all of the risks, benefits of the lumbar spine surgery, and gave informed consent.
- Bilateral laminotomies, foraminotomies, and medial facetectomies from L2 to L4.
- L2/3 far lateral discectomy through a posterior lateral approach.
- Neurolysis of right L2 nerve root bilateral L4 nerve roots, bilateral L3 and bilateral L4 nerve roots
- Un-instrumented posterolateral fusion with arthrodesis from L2 to L3.
- Use of local morselized autograft and morselized allograft.
- Use of physician-directed fluoroscopy.
- Complex wound closure with assistance from plastic surgery.
Patient was taken to the operating room where general anaesthesia was induced. She was positioned for surgery on her belly. Preoperative antibiotic was given. The incision was made after localization with fluoroscopy over the L2 to L4 levels. We made a midline incision over the spinous processes and continued our dissection using Bovie cautery in the avascular plane. We applied our self-retaining retractors to hold the muscle and skin edges apart and achieved hemostasis with bipolar cautery.
We continued our exposure from the inferior lamina of L1 to the bottom of L4 up to the facet joints. We exposed the pars interarticularis at each level and at L2-3, we tested the instability using Kocher camps and there was quite a bit of movement at this level.
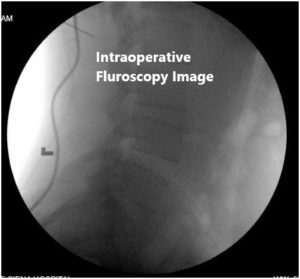
Intraoperative fluoroscopic images
We were concerned about this preoperatively given the patient’s level of back pain and anterolisthesis at this level, so we made an incision at this point to do a non-instrumented fusion from L2 to L3 as was discussed with the patient. We then exposed the transverse processes of L2 and L3 and we entered Kambin’s triangle at the far lateral side of the L2-3 level to enter the disc space and do discectomy.
We were very careful with dissection instruments to identify the nerve roots and keep them safe. We used a pituitary rongeur to remove the herniated disk and to free up the nerve root adequately. At this point, we then performed our laminotomies from L2 to L4 using the 3-mm matchstick drill.
We were able to decompress centrally as well as laterally at these levels using Kerrison punches and protecting the dura at all times using the Woodson dental instrument. We followed the nerve roots out from their exits from the thecal sac to the neural foramen freeing them circumferentially from all compressive elements.
We achieved both central and lateral recess and foraminal decompression. We at this point then decorticated the transverse processes of L2 and L3 on both sides and placed our fusion mass posterolaterally using a mixture of morselized autograft and allograft. The wound was washed out copiously with bacitracin irrigation and hemostasis achieved with cautery. The wound was closed in layers after instillation of vancomycin powder. The patient remained stable post-op. She was transferred to rehab center and had a good relief of pain and gradual recovery of her weakness.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
