Case Study: L4-5 Laminectomy and Discectomy
The patient presented with severe radicular pain on the left lower extremity, which was not relieved with conservative treatment and the patient was admitted to the hospital where magnetic resonance imaging (MRI) was done, which showed an extruded and herniated disc of left L4-5. The patient was also having weakness in the L5 myotome on the left.
Physical examinations revealed tenderness of the paraspinal region of L5 on both left and right sides. Patients active range of motion was lateral flexion to the left (20 deg.) and the right (20 deg.); rotation to the left (20 deg.) and the right (20 deg.); and flexion (40 deg.), extension (10 deg.), and pain with motion.
Their passive range of motion was lateral flexion to the left (20 deg.) and the right (20 deg.); rotation to the left (20 deg.) and the right (20 deg.); and flexion (40 deg.), extension (10 deg.), and pain with motion.
Straight leg raising test was positive on left side along with weakness of left extensor hallucis longus tendon. We discussed treatment options and the patient opted for surgical management.
We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, dural tear, aggravation of the pain, deterioration of neurological status, non-recovery of the pain, repeat surgery, repeat disc herniation and possible need for fusion in the future among others.
We discussed systemic complications including blood clot, cardiac, pulmonary, and neurological complications including blindness and death. The patient understood and signed an informed consent. MRI findings supported the diagnosis of spinal canal stenosis and neural foraminal narrowing.
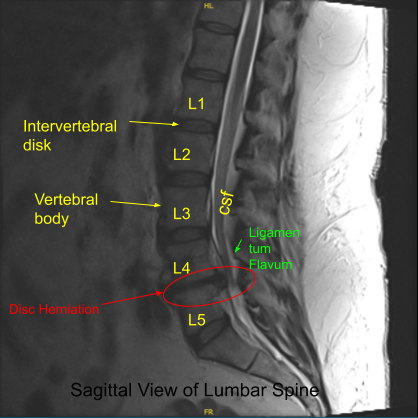
Sagittal View of Lumbar Spine
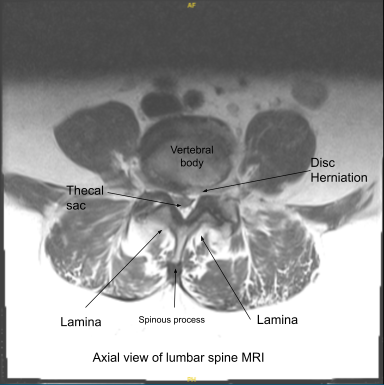
Axial view of Lumbar Spine MRI
The patient was taken to the operating room where general anesthesia was induced. Neuromonitoring was established. The patient was flipped prone on a Wilson frame on a four-post Jackson table.
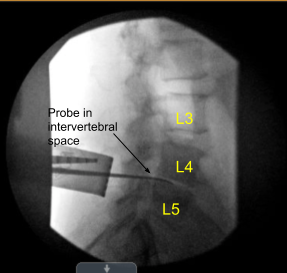
All the bony prominences were well padded. Spinal needle was used to mark the L4-5 intervertebral disc space. The lower back was prepped and draped aseptically in the usual fashion. Preop antibiotic in the form of 900mg of clindamycin was given. Time-out was called.
With sharp and blunt dissection, the skin, fascia and posterior interspinous ligament was cut in the line of incision. Paravertebral muscles were dissected and retracted laterally with the use of Bovie on the left side of the spinous process. The lamina of L4 was reached.
A fluoro was brought in and Woodson was put under the lamina of L4 and x-ray was taken to confirm our level. Once the level was confirmed, laminotomy of the left inferior L4 and superior laminotomy of left L5 was performed with the use of high-speed drill.
Once the laminotomy was performed, ligamentum flavum was seen. The ligamentum flavum on the left side of L4-L5 was removed to expose the nerve root. The nerve root was retracted medially with the use of Love nerve root retractor. The herniated disc could be seen.
Further annulus was cut with the use of a sharp blade and partial discectomy was performed with the use of pituitary with the help of ball tip probe. The specimen was saved for histopathology. Further examination with the nerve hook and Penfield showed good decompression of the nerve root with no residual fragments. Foraminotomy of left L5 and left L4 was done with kerrison 3 & 4 mm.
The Left L4 and L5 nerve root was released from nearby adhesions with the use of nerve hook and Penfield 4. Good decompression of the nerve roots was achieved. The wound was thoroughly irrigated. Hemostasis was achieved.
40 mg of Depo-Medrol was instilled in the area. Neuromonitoring was stable during the surgery. Closure of the fascia was done with the use of 0-Vicryl. 0.25% marciane was used to achieve local anesthesia.
Closure of the wound was done with the use of 2-0 Vicryl and 4-0 Monocryl. Dressing was done with the use of dermabond and telfa and tegaderm The patient was flipped supine, extubated and moved to recovery in a stable condition.
The patient initially followed up in two weeks after the surgery and then followed up in our office after 6 weeks. In their last office visit the patient stated their leg pain was relieved, she was able to move around and started to work.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
