Case Study: Transforaminal Interbody fusion
with Pedicle screw fixation of L5-S1
The patient who was seen in our office with complaints of left-sided radicular pain along with tingling and numbness. Aggravated by standing and walking. The patient was not able to perform usual activities of daily living let alone play sports.
The patient had a history of left-sided radiculopathy, which was treated with microdiscectomy in the past. The patient had tried conservative management in the form of NSAID’s, physical therapy, rest, but it did not help the patient.
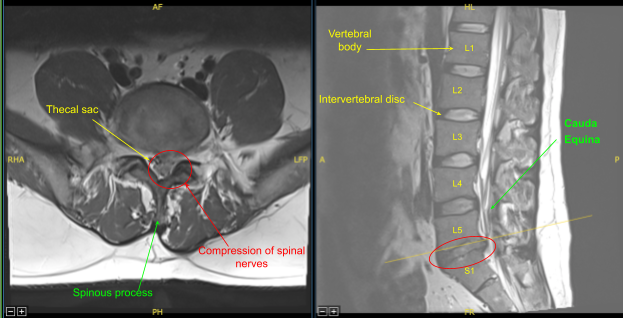
Magnetic resonance imaging (MRI) was done, which showed previous left hemilaminectomy at L5-S1, Left central disc herniation/extrusion at L5-S1 contributes to effacement of the thecal sac and left lateral recess with severe spinal canal stenosis and mass effect upon the descending left S1 and at least S2 nerve roots.
We had discussed treatment options including; surgical and non surgical, both their risks, complications and recoveries. We discussed the use of implants in the form of screws, rods and cage as well as use of biologics such as bone grafts and substitutes from his own bone, cadaveric bone as well as non-human derivatives. We discussed the need for extensive rehab, inability to return to presurgical level among others. Patient agreed with the plan which was a Transforaminal Interbody Fusion (TLIF) L5-S1 electively.
The patient was taken to the operating room where general anesthesia was induced and a Foley catheter was passed. Preoperative antibiotics in the form of 2g of Ancef was done, which was repeated after 4 hours of surgery. The patient was flipped prone on a four-post Jackson table.
All the bony prominences were well padded. The lower back was prepped and draped aseptically in the usual fashion. Time-out was called. He had a scar, which was on the left side of the midline.
Incision was given along the right margin of the scar towards the midline. The incision was extended deep through the subcutaneous tissue and the fascia. The spinous process was reached and dissection was done on either side of the spinous process of presumed L4, L5, and S1.
Dissection was taken down to the lamina on the right side of L4 and L5 and a Woodson was inserted underneath the lamina of presumed L5. X-ray was taken in lateral view and found that the Woodson was under the L5 lamina.
The level was marked and further dissection was performed on either side of L5, inferior L4 and the superior part of the S1 to the facet joint of L4-5 and L5-S1 on either side. Further dissection was done along the transverse process of L5 and sacral ala on either side.
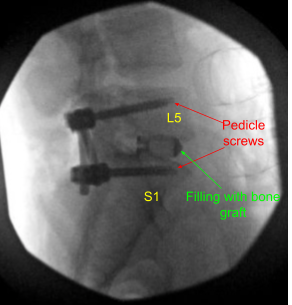
Once the dissection was done, the decision was made to put pedicle screws in both pedicles of S1 and L5. Drill was used to mark a pilot hole and a gearshift was used to guide the hole through the pedicle of S1 on either side under fluoroscopic guidance. Ball-tip sound was used to check the integrity of the canal.
Then 40 mm x 6 mm of pedicle screws (Depuy Synthes) were inserted on either pedicle of S1 and checked under fluoroscopy and found to be in satisfactory position. Similarly, a pilot hole was made with the use of drill on either side of the pedicle of L5 followed by a gearshift to find the path under fluoroscopy. A ball-tipped probe was again used and all the walls were found to be intact. Again, tapping was done and 6 mm x 45 mm pedicle screws were inserted in either pedicle.
Now the laminectomy of L5 was performed on either side with the use of kerrison punches and match stick burr. Pars was left intact on the right side, but the pars was excised on the left side with the use of burr and an osteotome. The superior facet of the S1 was also removed with the use of Kerrisons. Multiple large disc fragments were removed from the left S1 foramen to decompress the nerve.
A laminectomy and decompression of bilateral L5 and S1 was performed with kerrison punches and checked with a woodson probe. Discectomy of the L5-S1 was done on the left side with the use of curettes, shaver, and pituitary.
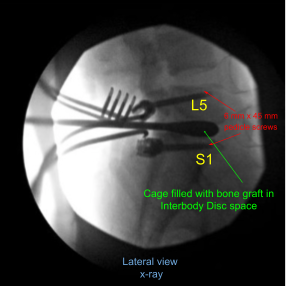
A trial cage was inserted and checked under fluoroscopy and it was decided to put a 9 mm x 36 mm titanium cage. Allograft was used and mixed with morselized auto bone graft of the lamina and spinous process. The cage and disc interspace was filled with bone graft and the cage was inserted and checked under fluoroscopy, found to be in satisfactory position.
A thorough irrigation of the wound was done and decortication of the transverse process of both L5, sacral ala as well as parts on the right side was performed and bone graft was inserted over the Fibergraft. The 45-mm rods were used to connect the both pedicle screws on either side and the set screws were inserted and tightened and torqued.
Final pictures were taken and saved. Surgiflo mixed with 40 mg Solu-Medrol was put over the exposed dura. In the process of decompression, there was patch of ligamentum flavum, which was stuck to the dura or left as an island as it was very risky to remove it. The nerve roots were thoroughly decompressed. Hemostasis was achieved.
The wound closure was performed in the layers by the plastic surgeon and was dictated separately. Two grams of Ancef was repeated after 4 hours of surgery. The patient was extubated and moved to the postoperative recovery unit in a stable condition.
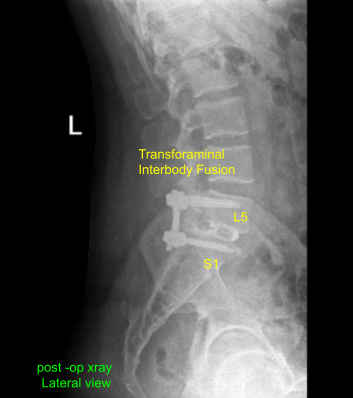
Postoperative X Ray showed there is a normal lumbar lordosis. There were no destructive abnormalities or fractures. The intervertebral disc spaces appear preserved. There was no spondylolisthesis. The facet joints appear unremarkable.
The patient followed up in our office two weeks after the surgery, with their post operative images. During this visit we discussed home exercise programs for rehabilitation of the back. We went over the X Rays and the surgical procedure. They agreed to continue icing to keep the swelling to a minimum and to continue to utilizing early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
They will lean themselves off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications. In their last office visit the patient stated their radiculopathy had been resolved.
They were able to perform all usual and recreational activities and were also able to exercise. They were able to do 40 pushups, run 1.5 miles in 15 min and plank for 1.5 minutes.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
