Case Study: Cervical disc replacement C5-C6 and C6-C7
Patient is a 40 yr old female who was seen in the office with complaints of pain radiating to both upper extremities with weakness, tingling and numbness. His physical examination and imaging findings were consistent with cervical canal stenosis. He had tried non operative treatment which has failed. We discussed treatment options and agreed for surgical management. Informed consent was taken.
The patient was brought to the operating room where general anesthesia was induced. The patient was put on the Jackson table. The neck was put in extension with the use of upper back rolls. Their shoulders were taped to the table to allow fluoroscopy of the lower cervical spine. Neuromonitoring was established. The area was cordoned and prepped and draped aseptically in the usual fashion. Preoperative antibiotic was given. A time-out was called.
Right transverse approach was planned. The level was checked under lateral fluoroscopy. A transverse incision was given along the neck crease on the right side. Hemostasis was achieved and platysma was reached. Supraplatysmal dissection was performed. The platysma was cut in the line of the incision.
Supraplatysmal dissection was performed to allow mobility of the incision. Deep dissection was performed between the strap muscles and sternocleidomastoid. The anterior spine was reached. Hemostat was used to check the level and found to be at C5-C6.
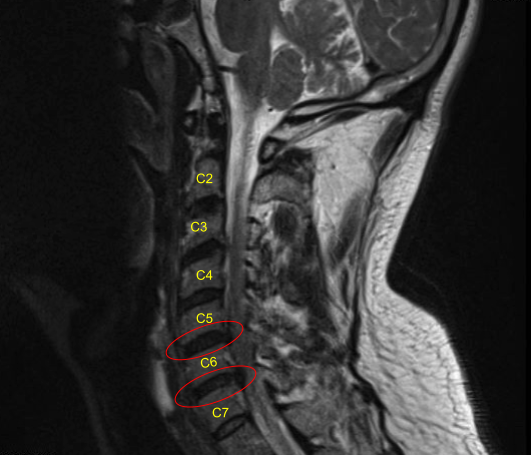
Further dissection was performed distally as well as proximally to open the area. A needle was used in the disc space to confirm the level and found to be C5-C6 and saved. The disc was marked and the distal disc was also marked at C6-C7. The longus colli was raised on either side of C5, C6, and C7 to expose the body as well as the disc.
Skyline retractors were used. Caspar pin were passed into C7 and C6 to allow distraction of C6-C7. Discectomy of C6-C7 was performed using curette and Kerrison. Thorough foraminotomy of bilateral C7 was performed with the use of Kerrison punches Number 1 and 2.
PLL was also excised and posterior osteophytes were removed using #1 and #2 Kerrison. Once the discectomy was performed, the endplates were leveled. Vertebral spreader was used to check the flattening of the surface. Template was used for the disc replacement and a 19 mm x 15 mm x 6 mm disc was planned. The disc was inserted into the disc space and checked with the C-arm and found to be satisfactory.
The disc holder was removed. Now, the C7 Caspar pin was removed and inserted into C5. Distraction of C5-C6 was performed using the Caspar distractor. Discectomy was performed using curette and Kerrison #1 mm and 2 mm. PLL was excised and osteophytes were removed. Thorough foraminotomy of bilateral C6 was performed with the use of Kerrison punches number 1 and 2.
The disc space was sized and 6 mm x 17 mm x 15 mm disc was planned. The disc was opened, inserted into the disc space, and found to be satisfactory in the AP and lateral view of the C-arm by fluoroscopy. Finding it in a satisfactory position, the Caspar pins were removed.
The wound was thoroughly washed. Surgifoam mixed with 40 mg of Depo-Medrol was instilled into the wound to allow hemostasis. Closure was done in layers using 2-0 Vicryl for platysma, subcuticular stitch, and 5-0 Monocryl. Steri-Strip was applied over the wound. The patient was extubated and moved to recovery in stable condition.
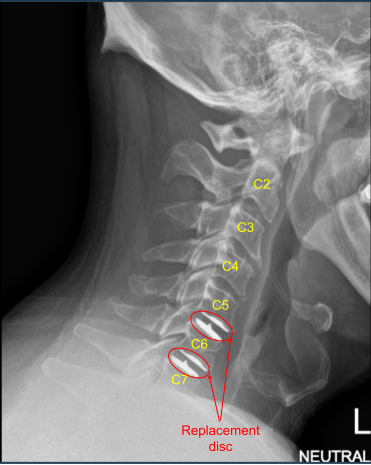
The patient was followed up regularly at 2, 6 12 weeks and then at 6 and 12 months. She made complete recovery and had full relief of symptoms.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
