Case Study: Transforaminal Lumbar Interbody Fusion L4-S1
The patient reported sharp and tingling pain radiating to the legs from the lower back. Patient reported pain levels to be 4/10 with weak limbs, numbness of the legs/feet with tingling. The patient had an operation for right leg radiculopathy and a microdiscectomy of right L4-L5 and L5-S1 was done prior.
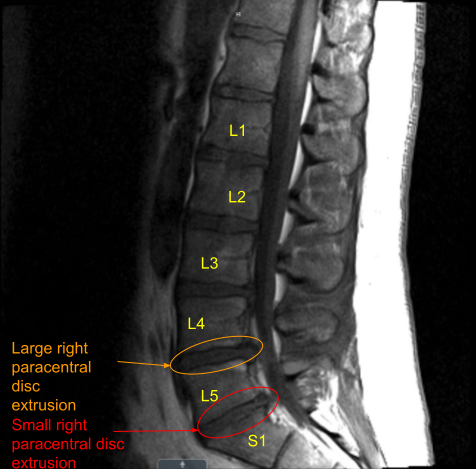
The patient had good relief after the surgery which was followed by recurrence of the pain in two weeks. This was associated with tingling and numbness along with foot drop on the right side. A repeat MRI was done which showed a re-herniation of disc on the right L4-L5.
MRI and CT of Lumbar spine were done which showed degenerative disc disease L4-5 and L5-S1 with re-herniation at L4-5.
We discussed treatment options including surgical and non surgical, their risks, complications and recovery. We discussed use of implants in the form of screws, rods and cage as well as use of biologics as bone grafts and substitutes from his own bone, cadaveric bone as well as non-human derivatives.
We discussed regarding the procedure and its risk of bleeding, infection, reherniation, restenosis, failure to fuse, implant failure, dural tear, worsening of symptoms, short or long term tingling, numbness, weakness, need for repeat surgery, chances of temporary or permanent nerve or vessel injury, risk of blindness, cardiac event, stroke, paralysis and death.
We discussed the need for extensive rehab, inability to return to presurgical level among others. Patient agreed with the for a transforaminal lumbar interbody fusion (TILF) L4-S1, understood and signed an informed consent.
The patient was taken to the operating room where IV lines were put in place. Patient was anesthetized and intubation was done. Neuromonitoring was put in place. Foley catheter was passed. 3 g of Ancef along with 1 g of TXA and dexamethasone before the surgery.
Patient was flipped prone onto the Jackson table associated with Aero. All the bony prominences were padded. A safety test was done and found to be adequate. Draped aseptically in usual fashion after monitoring that area. A time-out was called.
The scar of the previous surgery was marked and incision was given extending the scar proximally and distally. An incision was developed deeper direct to the subcutaneous tissue. Hemostasis was achieved and reflectors were placed in place. Bovie was used along with Aquamantys to achieve hemostasis and further dissection. Fascia was cut in line of incision.
Dissection was done on either side of the spinous processes. Laminotomy sites were reached and the tissue was preserved along the laminotomy sites. The dissection was carried laterally on either side of the spinal column. Dissection was carried along the facet joint onto the TP and the TPs of presumably L4, L5 and ala of S1 were dissected on either side.
Allis clamp was put on the right-sided L4 transverse process and imaging with fluoroscopy was done to confirm the level which was confirmed. Further preparation was done by exposing the lamina as well as the TP on both sides of L4 and L5 and bilateral S1. The navigation reference frame was put in phase by putting two Schanz pins into the right ilium through separate stab incisions.
Aero was brought in and a spin was done to obtain CT scan images. The navigation reference was verified. Having navigation ready, pedicle screws were planned to be inserted first on the left L4 followed by right L4, left L5, right L5, left S1, and right S1 sequentially.
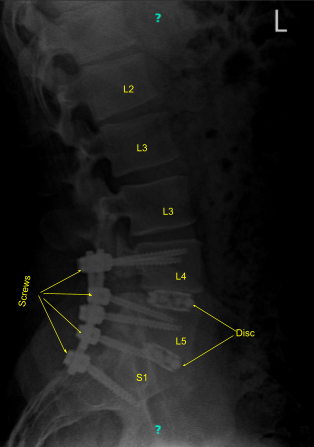
All the entry points were marked with the reference probe followed by drill, followed by navigator gear shift, navigator tip and insertion of pedicle screws on bilateral L4, bilateral L5, and bilateral S1.
Now the laminectomy of L4 and L5 was done with the use of rongeur, burr, and Kerrison. The parts on the right side were cut with the use of drill and the anterior facets of L4 and L5 were removed followed by partial removal of the superior facet of L5 and S1 with the use of Kerrison.
The disc space on L4-L5 and L5-S1 on the right side was reached. There was an extruded disc at L4-L5 on the right which was removed and put in a specimen container. Discectomy of L4-L5 was planned after retracting the dura to the left. Annulotomy was done with a knife up to 13 mm. Curette was also used sequentially to clean the disc space and pituitary was used to remove the disc fragments. Thorough discectomy was performed.
A 30 mm x 10 degree Globus expandable cage was opened and packed with bone. Bone graft was inserted into disc space followed by a cage which was expanded after checking under fluoroscopy.
Following that, the discectomy of L5-S1 was done in the similar fashion with annulotomy with a blade followed by discectomy with the use of paddle shavers sequentially up to 12 mm followed by curettes and pituitary forceps to remove the disc space material.
The end space was prepared again and a 36 mm x 10 degree expandable Globus cage was inserted. It was medialized. Pictures on fluoroscopy were taken and found to be acceptable but it felt that the cage on the L4-L5 was a little lateral, so it was removed and reinserted more medially and found to be in satisfactory position this time.
After that, a low dose CT scan with Aero was again done to confirm the placement of the screws and the cage. The newly taken pictures showed satisfactory positions of all the six pedicle screws and the cages x 2. Further adhesions of both bilateral L4,bilateral L5, and bilateral S1 nerve roots were released with the use of Penfield and Woodson tool.
The wound was thoroughly irrigated and drained. Decortication of bilateral TPs of L4 and L5 and ala of S1 was performed in preparation for fusion. Rod was inserted on both sides and fixed with set screws on L4, L5, and S1 screws bilaterally.
The set screws were torqued in all six locations. This was followed by insertion of bone graft which was locally harvested mixed with DBM into the gutters between L4 and S1 on both sides. Hemostasis was thoroughly achieved.
Final pictures were taken and saved. The neuromonitoring was stable during the time. Closure was done with insertion of drains. Patient was flipped supine and moved to recovery in a stable condition.
Patient followed up for 3, 6 weeks and then 3 and 6 months after the surgery. They reported being able to sit and walk while carrying out usual activities of daily living. They also reported that the pain had improved and they were back to work in 3 months.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
