Lumbar Laminectomy Surgery
If lumbar spine pain becomes so severe that it disrupts daily life or is accompanied by swelling, tenderness, or redness, it’s important to seek medical attention.
At Complete Orthopedics, our expert spine specialists are adept at treating lumbar spine pain through both surgical and non-surgical means. We examine symptoms, diagnose the condition, and recommend suitable treatments, including surgery if necessary.
Serving New York City and Long Island, we partner with six hospitals to offer cutting-edge lumbar spine surgery and comprehensive orthopedic care. You can schedule a consultation with our orthopedic surgeons online or by phone.
Learn about the common causes of lumbar spine pain and the treatment options available, including when surgery might be the best choice.
Overview
Lumbar laminectomy is a surgical procedure performed on the lower spine to relieve pressure on the neural structures, such as the spinal cord and nerves. This surgery is often necessary for individuals suffering from spinal canal stenosis, a condition where the spinal canal narrows and compresses the spinal cord or nerves. Typically, lumbar laminectomy is considered after all other conservative treatments have been exhausted. The results of this surgery are generally excellent, with most patients experiencing significant relief from their symptoms.
Anatomy of the Spine and Spinal Stenosis
The spinal cord runs through the spinal canal, which is formed by the vertebral bodies. As the spinal cord travels down the spine, it gives off branches known as spinal nerves. The spinal cord itself ends around the second lumbar vertebra, giving rise to a bundle of nerves called the cauda equina. This bundle continues down the spinal canal to supply the lower extremities and pelvic organs.
Structure of the Vertebrae
The lamina is a part of the vertebra that forms the roof over the spinal canal, surrounding the spinal cord from the back and sides. In spinal stenosis, the spinal canal narrows, causing compression of the spinal cord, the dural sac (which surrounds the spinal cord), or the cauda equina. This narrowing is often due to bone spurs, which are bony growths that intrude into the limited space of the spinal canal. These bone spurs are usually a result of degenerative changes in the spine or normal age-related changes. Other causes of spinal stenosis include herniated intervertebral discs, thickening of ligaments, and tumors.
Symptoms of Lumbar Spinal Stenosis
Patients with lumbar spinal stenosis typically experience symptoms due to the compression of the cauda equina, dural sac, or spinal cord. Common symptoms include:
- Radiating pain down the lower extremities
- Leg pain aggravated by walking and bending backward
- Numbness and tingling in the legs or feet
In advanced cases, patients may suffer from loss of sensation, muscle weakness in the lower extremities, and loss of bowel and bladder control.
Surgical Techniques for Decompression
Laminectomy involves the removal of most of the lamina of the vertebrae to relieve pressure on the neural structures. There are other related procedures as well:
- Laminotomy: Removal of only a part of the lamina.
- Laminoplasty: Creating a hinge using the lamina to increase the space in the spinal canal.
During a laminectomy, the surgeon makes an incision on the back at the affected level, determined by radiological studies. The surgeon then carefully separates the tissues, including muscles, to reach the spinal lamina. Using cutting instruments, the ligamentum flavum, a ligament covering the spinal cord, is removed to access the spinal cord. The lamina is then removed to create more room for the neural structures. Other structures that might be compressing the dural sac, such as bone spurs and herniated discs, may also be removed during the procedure. Care is taken to avoid removing more than half of the facet joint to prevent spinal instability.

MRI of the lumbar spine in the sagittal section showing disc herniations narrowing the spinal canal.
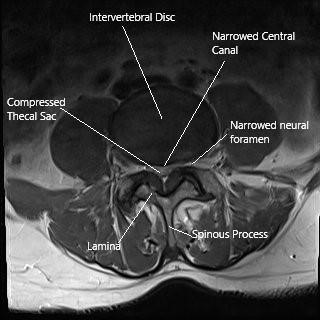
Axial section of the lumbar spine showing spinal stenosis and the lamina.

Hexagonal screw driver
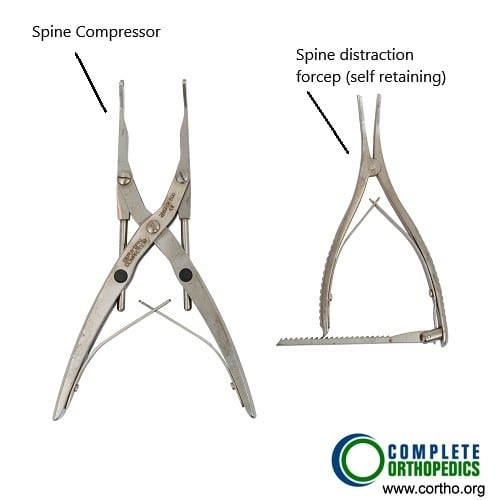
Spine compressor and distraction forceps
The images above show some of the instruments used in posterior lumbar spine laminectomy/fusion. The instruments are used to decompress the spinal nerve/dura and also aid in insertion and fixation of implants in the posterior spine if needed.
Surgical Techniques for Decompression
Laminectomy involves the removal of most of the lamina of the vertebrae to relieve pressure on the neural structures. There are other related procedures as well:
- Laminotomy: Removal of only a part of the lamina.
- Laminoplasty: Creating a hinge using the lamina to increase the space in the spinal canal.
During a laminectomy, the surgeon makes an incision on the back at the affected level, determined by radiological studies. The surgeon then carefully separates the tissues, including muscles, to reach the spinal lamina. Using cutting instruments, the ligamentum flavum, a ligament covering the spinal cord, is removed to access the spinal cord. The lamina is then removed to create more room for the neural structures. Other structures that might be compressing the dural sac, such as bone spurs and herniated discs, may also be removed during the procedure. Care is taken to avoid removing more than half of the facet joint to prevent spinal instability.
Types of Laminectomy Procedures
- Unilateral Laminectomy: Performed on one side of the spine.
- Bilateral Laminectomy: Performed on both sides of the spine.
In unilateral laminectomy, the surgery can also be performed using an endoscope, which allows for minimally invasive techniques and smaller incisions. In cases where extensive decompression might lead to instability at one or more levels, a lumbar fusion is performed alongside the decompression. Lumbar fusion involves joining adjacent vertebrae using a cage filled with bone graft, and may also include the use of screws and rods to stabilize the fusion.
Indications and Contraindications
Lumbar laminectomy is indicated for patients with clinical and radiological signs of lumbar spinal stenosis who have not responded to conservative treatments. Conservative management includes physical therapy, medications, and epidural steroid injections. Surgery is considered only when these treatments have failed to provide adequate relief.
Post-Operative Care and Complications
Most patients can go home the same day after surgery, although those undergoing lumbar fusion may require a longer hospital stay. As with any surgery, lumbar laminectomy carries potential complications, including:
- Leakage of spinal fluid
- Hematoma formation (a collection of blood outside of blood vessels)
- Infection
- Bleeding
- Nerve injury
Surgical Instruments
Various instruments are used in posterior lumbar spine laminectomy and fusion procedures. These include tools for decompressing the spinal nerve and dura, as well as instruments for the insertion and fixation of implants in the posterior spine.
Conclusion
Lumbar laminectomy is a well-established surgical procedure for relieving the symptoms of spinal stenosis. With advancements in surgical techniques and a better understanding of spinal anatomy and pathology, the outcomes of this surgery continue to improve. Patients considering lumbar laminectomy should discuss the potential benefits and risks with their healthcare provider to make an informed decision. The combination of laminectomy with other procedures, such as lumbar fusion, should be carefully evaluated based on the patient’s specific condition and overall health.
Do you have more questions?
What is laminectomy and what is the purpose?
Laminectomy involves removal of the back of the vertebrae so as to remove pressure from the spinal cord or the spinal nerves in the vertebral column. This can be performed in the neck, chest, or lower back area depending on the location of the compression over the neural elements.
Who does the laminectomy?
A laminectomy is performed by spine surgeons or surgeons who specialize in doing spine surgeries.
Will the laminectomy remove all my pain?
Laminectomy in the lower back is very helpful in patients who have radicular pain going down their legs. In most of the patients, the symptoms are well resolved, and these patients are able to get back to their normal life within six to ten weeks after the surgery.
What if, during my surgery, you encounter a different issue other than expected?
Usually, before the surgery, we discuss with the patient regarding all the possible spine issues that we may expect and how to manage them. If there is an unexpected issue, which has not been discussed earlier, we would go ahead and discuss it with the patient’s relative and treat it accordingly from there. If there is something which can wait, and is not detrimental to the patient, and relatives are not able to make decision on it, we may leave it for a later date to be discussed with the patient after the surgery.
How long is it possible to stay for back surgery?
Most of the patients with back surgery can be discharged within one to four days after the surgery depending on the type of surgery and the type of recovery that they have. Patients who undergo complex spine surgeries may need longer period of hospitalization and recovery.
Which pain medications will I be sent home with? What are the possible side-effects of these prescriptions?
Most of the patients with cervical spine surgery, will be sent with some narcotic pain medication to take care of their pain. These medications do have their multiple side-effects, which may be constipation, nausea, vomiting, impaired judgement, drowsiness, headache. Though patients who are treated with narcotic pain medication for acute pain, mostly do not lead to addiction, but these medications do have addiction potential.
Will you know before the surgery if I need a brace afterwards? If so, will I be fitted for one before the surgery?
Most of the patients with spine surgery do not need a brace. If we expect that the patient will need a brace, we will get the patient pre-fitted with a brace so that it is available immediately after the surgery. Occasionally the need for brace may be decided at the time of surgery. In such cases a brace is arranged in immediate post-operative period.
Will I need any other medical equipment like a walker when I go home? Should I get an adjusted bed or sleep downstairs?
Patient may need other medical equipment like walker or a stick. If that is required, patients are provided with such equipment in the hospital before their discharge and are trained how to use them by the physical therapist and occupational therapist. If the patient needs to use stairs, patients are trained by the physical therapist before they are let go home. If the patient needs an adjustable bed, they are informed about that. That can be done prior to the surgery. It is desirable for patients to stay downstairs for a few weeks if possible.
Who can I call if I have questions after the surgery?
In case patient has routine questions regarding after the surgery or regarding the surgery, they can call the physician’s office and talk to the nurse or secretary or the physician. If they’re not available on the phone, they can leave a voice mail and they will be answered later. In case the patient has a medical emergency, then they should not call the physician office but rather call 911 or get to the hospital ER as soon as possible.
How often will I see you after my surgery?
Patients are usually followed at two weeks, six weeks, three months, six months, and a year after surgery.
What symptoms would warrant a call to your office after the surgery?
If the patient develops problems like chest pain, breathing problems, sudden neurological deterioration, or any other emergency they should call 911, or go to the emergency room directly. Patients who develop worsening pain at the surgery site, discharge from the wound, fever; they should call in the office.
How long should I wait to bathe after the surgery?
Patients are usually asked to avoid bathing, until the incision heals, which may take two to three weeks. Patient can take shower after 72 hours of surgery with an impervious dressing in place. The dressing can be changes if the wound is visibly soaked. Patients are asked not to rub the area of surgery for about two to three weeks. They can gently dab it dry with a towel.
How long will I be out of work?
Patients with low demand work and desk job, can be back to work as soon as three to six weeks after the surgery depending on patient pain control as well as recovery. Patients who are in heavy lifting or control of heavy machinery or handyman job, may take three to four months, or even more to get back to work depending on their recovery from the surgery.
How soon after the surgery can I start physical therapy?
Patients after back surgery are usually started on physical therapy, if they need, depending on physician’s advice, at two to four weeks after the surgery. Many of the patients do not need physical therapy. A decision to go into physical therapy will depend on the surgery as well their recovery.
What if I get an infection?
If the patient has a superficial infection, few days of antibiotics will help heal these infections. Occasionally patient may develop deep infection. In these patients may need IV antibiotics for a longer period. If despite all efforts or in patients with rapid deterioration due to infection, surgery may be needed to help clean off the infection.
How common is surgery?
Most of the patients do not need surgery and can be treated with conservative means. When the patients do not respond to conservative measures, or if they have worsening neurological deficit, or worse pain, they may need surgery.
Will I have irreversible damage if I delay surgery?
Patients who develop neurological deficit in the form of weakness or involvement of bowel or bladder may have irreversible damage if the surgery is delayed enough.
When do I need fusion?
When patient has back pain or has a surgery in which enough bone is removed to destabilize the spine, in these cases patient may need a fusion surgery to stabilize the spine, as well as to alleviate the symptoms.
What are my risks of low back surgery?
General surgical risks of low back surgeries include bleeding, infection, persistence of pain, reversible/irreversible nerve damage leading to tingling, numbness, or weakness down the legs or involvement of bowel or bladder, failure of resolution of symptoms, failure of fusion, failure of implants. Most of the patients can undergo a safe surgery due to the development of vision magnification as well as refined surgical techniques. There are anesthesia risks also associated with this surgery.
When will I be back to my normal activities?
Though these things depend on the type of surgery patient has undergone, patient can usually be progressively back to their normal activities, starting from three to five days from surgery. Patients are encouraged to take care of their activities of daily living, as well as light household activities. Patients can get back to driving once they are free from pain medication and are able to sit for a duration of period for driving, which may take upto 2-3 weeks or more.
What type of surgery is recommended?
The type of surgery depends on the presenting complaint, examination findings, as well as imaging findings in the form of x-ray and MRI. Some patients may need to undergo just discectomy, or laminectomy, while others may need a fusion surgery on their back to relieve their symptoms. To know more about the type of surgery, the patient needs to discuss this with their spine surgeons.
How long will the surgery take?
Spine surgeries like discectomy and laminectomy usually last about one to one and a half hours. Spine fusion surgeries, may take longer periods, up to two and a half to four hours or more. It depends on type of surgery, and as well as the level of spine to be operated upon.
What is degenerative disc disease?
Degeneration means gradual damage of the tissue. Degenerative disc disease represents aging of the disc, either appropriate to the normal age of the patient, or maybe accelerated due to injury or chronic disease, or other factors like smoking, obesity.
What is Lumbar instability?
Lumbar instability means that the spine is not stable and there is excessive abnormal movement between two vertebrae. This is usually diagnosed by imaging in the form of X-rays, CT scan, or MRI of the patients. Instability may lead to compression of nerve roots causing radiculopathy with or without back pain.
What is Spinal Stenosis?
Spinal Stenosis means narrowing of the spinal canal. It is can be at the cervical or thoracic or lumbar level. Most common spinal stenosis is at lumbar level and it, when narrowed, can compress nerves, causing pain going down the legs, with or without tingling, numbness, weakness, or involvement of bowel or bladder.
What is sciatica?
Sciatica is another name for lumbar radiculopathy, in which patient has pain going down their legs. The pattern of pain depends on the nerve root involved, but the most common is pain going down the outer side of the thigh and leg into the foot.
What is lumbar disc disease? How is this problem diagnosed?
The diagnosis of Lumbar disc disease is made by history and examination of the patient. The confirmation of diagnosis is done by imaging in the form of X-rays and MRI. Occasionally the patient is having contraindication to MRI, patient may need to undergo a CT scan. When a CT scan is done, occasionally the patient may need to get injected with a dye before the CT scan and this is called CT myelography. Occasionally patient may need a CT scan along with MRI also.
When should I consider surgery for the back pain?
Most of the patients get treated with conservative means. In case the patient is not getting relief despite continuous conservative measures, or if there is worsening of pain associated with or without weakness or involvement of bowel or bladder, the patient may need surgical intervention in the form of surgery.
Am I a candidate for minimal-invasive spine surgery?
Some patients are good candidates for minimally-invasive spine surgery and they can get better with that. History, physical examination, as well as special investigations like X-ray and MRI, are needed in order to discuss regarding options of minimal invasive spine surgery. Some patients are not good candidates for minimal invasive spine surgery and doing such a surgery in such patients may lead to non-resolved solution of the symptoms or worsening.
Are there any warning symptoms?
Warning symptoms of lumbar disc disease include worsening pain, tingling and numbness, development of weakness, or worsening of weakness, involvement of bowel or bladder in the form of incontinence of urine or stools, presence of fever, unintentional weight loss. In such conditions patients should immediately seek medical attention.
Do you need any tests?
General blood workup is needed in most patients before the surgery. This will include blood counts as well as metabolic profile. Special tests may be needed in some patients if the physician has suspicion of some other disease. Most of the patients will have to undergo X-ray and MRI, or a CT scan before the surgery to confirm their diagnosis.
What are the possible surgical complications from a low back surgery?
Common complications of a low back spine surgery are bleeding, infection, leak of cerebral spinal fluid temporary or permanent neurological deficits, blindness, worsening of pain, failure of fusion, failure of implants. There may be risks due to the anesthesia also.
What is foraminotomies?
Foraminotomies is the surgery done from the back in the neck or the lower back area in which a small amount of bone is removed to increase the size of the foramen where the nerve roots pass to give more space to the nerve root and to relieve the symptoms. These surgeries do not involve removal of enough bones to require insertion of screws and rods to fuse the spine.
What are the risks of laminectomy?
Apart from the usual risks of having some back surgery, the risk of laminectomy includes injury to the nerve roots of the spinal cord, bleeding, injury to the sac, covering the spinal root or spinal cord leading to leakage of the fluid, persistence of pain or worsening, temporary or permanent worsening of symptoms. It may also lead to delayed restenosis as well as destabilization of the fragment leading to forward bending of the spinal column.
What is post laminectomy pain syndrome?
Post laminectomy pain syndrome usually involves the lower back and presents in patient who have undergone laminectomy for spinal stenosis. These patients, due to worsening of their degenerative condition or osteoarthritis of the back, start having pain involving the disc in their lower back. They may also develop flattening of the back due to weakness and muscle spasm.
Is laminectomy an outpatient surgery?
One or two level laminectomy of the lower back can be done through outpatient. Laminectomies more than two levels or laminectomies of the cervical spine or thoracic spine are usually performed in a hospital setting due to the complexity of the surgery.
What is the difference between a laminectomy and discectomy?
The disc is present in the front of the spinal cord or nerve roots and the lamina are present behind the spinal cord of the nerve roots. Discectomy involves surgery usually from the front, though it can also be performed from the back especially in the lower back and involves removal of the disc to remove the pressure from the front of the neural elements. Laminectomy on the other hand is performed from the back and involves removal of pressure from the neural elements from the back. Sometimes especially in the lower back area, both the surgeries can be combined and usually performed from the back.
What is laminectomy of the neck?
Laminectomy of the neck involves removing the lamina from the vertebrae or the bones of the neck. These laminae are present on the back of the neck and the surgery is done through the back of the neck. These patients also need to undergo fusion with screws and rods so as to prevent later complications of laminectomy. This is usually done for patients who have impingement of their nerves in the neck from the back side rather than the commoner form that is from the front.
What is thoracic laminectomy?
Thoracic laminectomy involves removal of the lamina from the back of the vertebrae or bones of the thoracic spine or the chest region. The surgery is done from the back and may or may not involve fixation with screws and rods. This surgery is usually performed for patients who have compression on their spinal cord in the thoracic spine.
What is cervical decompressive surgery?
Cervical decompressive surgery is removal of pressure that is on the spinal column or the spinal cord in the neck region. This can be performed from the front or from the back depending on the location of the compression on the spinal cord. This surgery may or may not be accompanied with fixation of the vertebrae using screws, rods or plates.
What is laminectomy and what is the purpose?
Laminectomy involves removal of the back of the vertebrae so as to remove pressure from the spinal cord or the spinal nerves in the vertebral column. This can be performed in the neck, chest, or lower back area depending on the location of the compression over the neural elements.
Who does the laminectomy?
A laminectomy is performed by spine surgeons or surgeons who specialize in doing spine surgeries.
What is laminoplasty of the neck?
The laminoplasty involves cutting of lamina on one side so as to open it up and fixing it in an open position with the use of mini plates so as to increase the size of the spinal canal and decrease the pressure on the spinal cord. This surgery is performed from the back of the neck and does not involve fusion of the neck thereby decreasing the restriction of movement of the neck as may be present after laminectomy and fusion surgery.
What is cervical spine foraminotomy?
Cervical spine foraminotomy is a minimal invasive surgery which is performed from the back of the neck for pinched nerve in the neck. These patient’s usually have radiating pain into the arm and the surgery helps in decreasing the pressure over the cervical spine nerve root to allow space for the nerve and eliminate the symptoms. This surgery if done in suitable candidate can avoid fusion surgery that is traditionally needed to decrease the pressure of the spinal roots.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
