Cervical Degenerative Disk Disease
If neck discomfort escalates, disrupts daily routines it is essential to see a healthcare professional. At Complete Orthopedics, our specialized team is dedicated to managing neck injuries through personalized strategies and surgical interventions. We aim to comprehend your symptoms, pinpoint the root causes, and suggest appropriate therapies or operations.
Our centers are located throughout New York City and Long Island, linked to six leading hospitals, providing access to superior neck care. You can book an appointment with our orthopedic specialists either online or via phone. Explore the reasons and treatments for neck pain and understand when surgical intervention is the most effective solution.
Overview
Degeneration means wear and tear, usually due to aging process. This wear and tear can involve any joint of the body, which also includes a spine in the cervical spine or the neck.
This aging process can set in at a variable speed in different individuals depending on individual characteristics, genetics, modifiable factors like injuries, smoking, systemic diseases among others. The degeneration in the cervical spine can involve either of the three joints namely the two facet joint and the one disc space.
All the three are usually involved simultaneously, but it is the degeneration of the disc which is more often symptomatic and needs treatment. The degeneration of the disc can be accelerated due to injuries in the form of a single accident or exposure to microtrauma over a period of time. Systemic diseases like rheumatoid arthritis can also accelerate the process of degeneration.
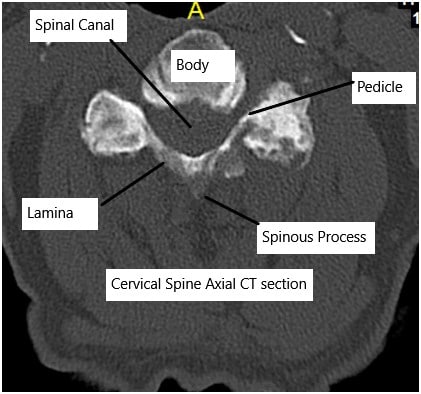
Cervical CT scan showing axial section.
The degenerative disc disease of the cervical spine usually involves the most mobile segment that is the C5-C6 followed by C6-C7 and C4-C5 disc levels. The degeneration causes decreased water content of the disc or desiccation which leads to tears in the outer ring or the annulus fibrosus.
These tear allow the herniation of the central nucleus pulposus to the periphery. When these herniations are along the back of the disc, they can compress over the spinal cord or the nerve root leading to variable symptoms and presentation
Presentation
Vast majority of patients who have degenerative cervical disc disease are asymptomatic and remain asymptomatic throughout their life. A small percentage of patients present with symptoms of neck pain or that of compression of the nerve root on one side presenting with symptoms of radicular pain going down the specific dermatome in the arm, tingling, numbness, and rarely weakness of the muscles innervated by that specific nerve root.
These radicular symptoms are caused by the disc herniation onto the side of the back of the disc thus compressing the nerve root. Rarely patients may have disc herniation to the back in midline, which can compress the spinal cord leading to symptoms in one or all four extremities along with tingling, numbness, radicular pain, electric shock-like sensations, involvement of bowel or bladder and gait abnormalities.
These patients may also have hand dexterity problems in the form of dropping things, weakness of the grip strength, change in handwriting among others. Patients may have disc degenerative disease of multiple levels causing multilevel cervical stenosis. There may also be hypertrophy and calcification of the ligament on the back of the spinal cord contributing to the stenosis.
Patients with congenital cervical stenosis may be predisposed to such disease. These patients may present with acute deterioration of their neurological symptoms following trivial trauma or whiplash type injury in the neck.
Diagnosing Cervical Degenerative Disc Disease
Medical History and Physical Examination: Doctors will review your symptoms, medical history, and conduct a physical examination to assess pain, movement, and nerve function.
Imaging Tests:
-
- X-rays: Can show the alignment of the spine and any narrowing of the disc spaces.
- MRI: Provides detailed images of the discs and nerves, helping to identify degeneration and nerve compression.
- CT Scans: Useful in assessing bone abnormalities.
Examination of patients with radicular pain may show weakness of specific muscles and dulling of reflexes while in patients with compression of the spinal cord may show increased tone of the muscles, weakness, decreased sensation as well as hyperreflexia.
Red Flags
The patients who have back or neck pain with any of these following conditions should seek medical attention as soon as possible.
1. Cancer, neoplasia or malignancy.
2. Unexplained weight loss of more than 10 pounds in the last 6 months.
3. Immunocompromised comorbidities like on chemo or radiotherapy or having disease like HIV or AIDS or being on prolonged corticosteroid therapy.
4. IV drug users.
5. Urinary tract infection.
6. Fever of more than 100 degrees centigrade.
7. Significant trauma from a fall or accident.
8. Bowel or bladder involvement in the form of incontinence or retention.
9. Weakness in the major joint of arm or leg.
Treatment
Most people with cervical degenerative disc disease are asymptomatic and remain asymptomatic for their life.
These patients may never visit a physician for the complaints with regard to the cervical degenerative disc disease. Some of these patients may have neck x-rays for unrelated reasons and may be found to have degenerative disc disease.
Such patients do not need any active treatment. Patients who present with occasional neck pain can also be treated with exercises and occasional medications.
Patients with symptoms of radiculopathy are usually treated conservatively for 4 to 6 weeks with excellent chances of resolution of symptoms. These patients are usually treated with physical therapy and medications. Neck collar may be used for a short period. If the patient fails conservative treatment, an MRI is usually performed to confirm the level of disease and collaborate with clinical findings.
These patients are offered surgical management to relieve them of the pain. Surgical management for cervical degenerative disc disease with compression of the nerve root or the cord from the front is usually in the form of cervical fusion or disc replacement done from the front. Another option include microscopic posterior foraminotomy, done from the back, which is a motion sparring (non-fusion) minimal invasive surgery.
Patients who have compression of the spinal cord from the back may need surgery from the back to relieve the pressure. Surgery from the back may involve removing of the bony elements from the back, relieving of the pressure and cervical fusion over multiple levels (Laminectomy and Fusion) or opening of the bony elements of the back using many plates to increase the space available for the spina (Laminoplasty).
A decision between varied surgical procedure is usually made on patient characteristics and presentation. Patients with spinal cord compression may need an emergent treatment plan especially in presence of deteriorating neurological status or acute onset to contain the neurological damage as well as allow possible recovery.
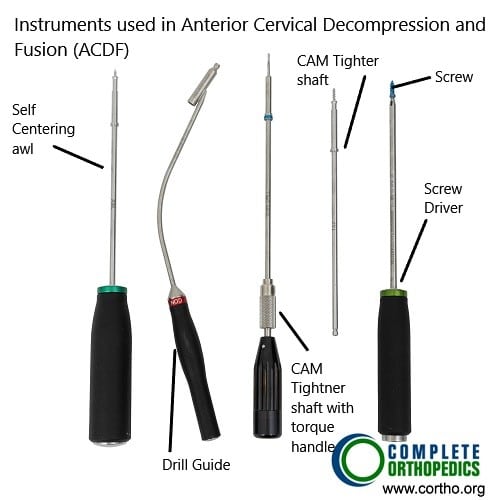
Instruments used in ACDF
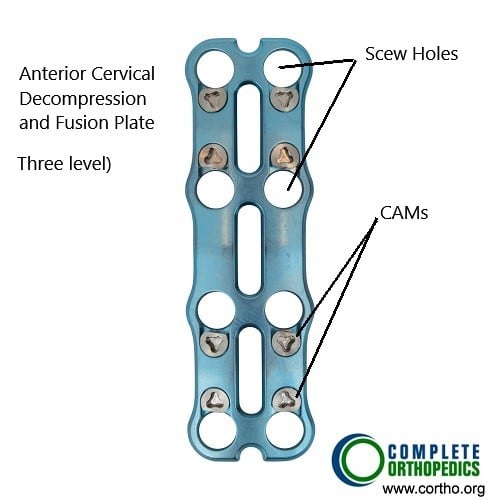
ACDF Plate (3 level fusion)
The images above show ACDF (anterior cervical decompression and fusion) plate and instruments used to fuse the cervical vertebrae from the front of the neck. The surgery helps to decompress the spinal nerves/spinal cord and prevent movement between the segments to alleviate the symptoms and achieve stability.
Recovery
Patients who undergo conservative treatment usually have excellent chance of complete recovery of their symptoms over a span of 4 to 6 weeks. Patients who fail conservative treatment may need surgical management for resolution of symptoms.
Patients who undergo surgical management for radicular pain in the form of cervical discectomy and fusion, disc arthroplasty or posterior foraminotomy usually have near complete recovery along with resolution of symptoms.
Patients who have spinal cord compression may have guarded prognosis. The recovery is inversely proportional to the deterioration of neurological deficit prior to surgery. Though the surgery may optimize and allow good environment for spinal cord to recover, it may take many months to years for a partial or a near complete recovery.
Occasionally despite all measures, patient may not get any recovery. Patients with spinal cord compression have a prolonged rehabilitation period and are at risk for multiple other problems including urinary tract infection, lung infection, deep vein thrombosis, pulmonary embolism, aspiration pneumonia, respiratory depression, death among others.
Complications
As for all surgeries there are certain but rare risks for anesthesia including cardiac arrest, stroke, paralysis, and rarely death.
Risks of Cervical spine surgery may include though not limited to:
• Hematoma or hemorrhage
• Damage to the carotid or vertebral artery which may result in a stroke or excessive bleeding, even death
• Blindness
• Damage to the nerve in the neck resulting in hoarseness or swallowing difficulties
• Damage to the food or wind pipe
• Damage to the dura, resulting in a cerebrospinal fluid leak
• Failure, loosening or pull out of the graft, cage, implant or plate
• Wound infection
• Failure of fusion to happen
• Damage to the spinal cord or nerve root(s) resulting in new onset or deterioration of preexisting pain, weakness, paralysis, loss of sensation, loss of bowel or bladder function, impaired sexual function, etc., which may or may not recover.
• A few of these conditions may warrant repeat surgery
Certain patient population is at a higher risk for complication which include but are not limited to:
• Smoking
• Seizures
• Obstructive sleep apnea
• Obesity
• High blood pressure
• Diabetes
• Other medical conditions involving your heart, lungs or kidneys
• Medications, such as aspirin, that can increase bleeding
• History of heavy alcohol use
• Drug allergies
• History of adverse reactions to anesthesia
WHO IS A GOOD CANDIDATE FOR CERVICAL DEGENERATIVE DISC DISEASE SURGERY?
Patients with radicular pain involving one or more than one nerve roots who have failed conservative treatment are good candidate for surgical management.
The surgical treatment stops the progression of the symptoms and allows optimum environment for the nerve root to heal and recover and resolve the symptoms as well as restore muscle power.
Patients who develop acute deterioration of neurological symptoms or acute onset of symptoms have a good chance of halting the progression as well as allowing recovery of the spinal cord nerve root and neurological function.
Patients who have had neurological deterioration for a long time may not be benefitted with the surgery especially if the symptoms have been stable.
Though a surgery may provide an environment for the spinal cord to heal and recover, but any recovery may not be complete. Patients with pain usually have good relief, those with numbness and tingling may take some time.
WHAT OTHER SURGERIES FOR DEGENERATIVE CERVICAL DISC DISEASE?
The surgeries for cervical degenerative disc disease include anterior cervical discectomy and fusion (ACDF), anterior cervical corpectomy and fusion (ACCF), or hybrid procedure including ACDF and ACCF, posterior microscopic foraminotomy, total cervical disc replacement, posterior laminectomy and fusion, and laminoplasty.
Conclusion
Cervical disc degenerative diseases are common phenomena in aging population. Patients are asymptomatic in vast majority of population and do not need any treatment.
Patients who are symptomatic can usually be treated with conservative means with a successful outcome. Patients who have failed conservative measures and patients with sudden or rapid onset or deterioration of neurological symptoms can be treated with surgery with good results.
Patients who have profound neurological involvement may have guarded recovery even after surgical management.
Do you have more questions?
What are the earliest signs of Cervical Degenerative Disc Disease?
The earliest signs often include mild neck pain and stiffness, which may be more noticeable after activities that strain the neck. Some people may experience a slight decrease in neck flexibility.
How does cervical disc degeneration differ from other types of arthritis in the spine?
Cervical disc degeneration primarily involves the breakdown of the intervertebral discs, while other types of arthritis, like osteoarthritis, affect the joints and bone surfaces. Both conditions can coexist, contributing to neck pain and stiffness.
Are there specific activities I should avoid to prevent worsening of CDDD?
Avoid activities that involve heavy lifting, repetitive neck movements, and prolonged periods of poor posture, such as looking down at your phone or computer screen for extended times.
How effective are non-surgical treatments for managing CDDD?
Non-surgical treatments like physical therapy, medications, and lifestyle changes are effective for many people in managing pain and improving function. They can significantly reduce symptoms and delay the need for surgery.
Can physical therapy completely cure CDDD?
Physical therapy cannot cure CDDD but can effectively manage symptoms, improve neck strength and flexibility, and enhance overall function, thus improving quality of life.
Are there any alternative therapies that might help with CDDD?
Alternative therapies such as acupuncture, chiropractic care, and massage therapy can provide symptom relief for some individuals. Always consult with a healthcare provider before starting any alternative treatments.
How do I know if my CDDD is severe enough to consider surgery?
Surgery is considered if conservative treatments fail, symptoms significantly impact your daily life, or if there is evidence of nerve compression causing severe pain, weakness, or loss of function.
What are the risks associated with cervical spine surgery?
Risks include infection, bleeding, nerve damage, spinal cord injury, persistent pain, and complications from anesthesia. Discuss these risks thoroughly with your surgeon.
How long is the recovery period after cervical spine surgery?
Recovery time varies but typically ranges from several weeks to a few months, depending on the type of surgery and individual factors like overall health and adherence to rehabilitation protocols.
Can cervical disc degeneration lead to permanent disability?
While rare, severe cases of CDDD can lead to significant nerve damage and permanent disability if left untreated. Early intervention and appropriate management are crucial.
Is cervical disc replacement surgery better than spinal fusion?
Cervical disc replacement preserves more natural neck motion and may reduce the risk of adjacent segment disease. However, suitability depends on individual factors, and both procedures have their own benefits and risks.
Can wearing a neck brace help with CDDD?
A neck brace can provide short-term relief by limiting motion and allowing the neck muscles to rest. However, long-term use is not recommended as it can weaken neck muscles.
How can I differentiate between neck pain from CDDD and other conditions like a muscle strain?
CDDD-related pain often includes stiffness and radiating pain to the shoulders, arms, or hands. Muscle strain pain is usually localized and may improve with rest and simple treatments.
Is it safe to exercise with CDDD?
Yes, exercise is generally safe and beneficial. Low-impact activities like walking, swimming, and specific stretching and strengthening exercises recommended by a physical therapist can help manage symptoms.
How does smoking affect cervical disc health?
Smoking reduces blood flow to the discs, accelerating degeneration and impairing healing. Quitting smoking can improve overall spine health and reduce pain.
Can cervical degenerative disc disease cause headaches?
Yes, CDDD can cause cervicogenic headaches, which originate from neck issues and can radiate to the back of the head and temples.
Are there specific sleeping positions recommended for those with CDDD?
Sleeping on your back or side with a supportive pillow that keeps your neck in a neutral position is recommended. Avoid sleeping on your stomach as it can strain the neck.
What is the prognosis for someone diagnosed with CDDD?
The prognosis varies. Many individuals manage symptoms well with conservative treatments, while some may require surgical intervention. Early diagnosis and proper management can lead to a good quality of life.
Can stress worsen the symptoms of CDDD?
Yes, stress can increase muscle tension and pain perception, exacerbating symptoms. Stress management techniques like mindfulness and relaxation exercises can be beneficial.
How often should I have follow-up appointments if diagnosed with CDDD?
Follow-up frequency depends on symptom severity and treatment response. Initially, more frequent visits may be necessary, tapering off as symptoms are managed effectively.
Can I use a heating pad or ice pack for pain relief?
Both can be effective. Use a heating pad to relax muscles and improve blood flow or an ice pack to reduce inflammation and numb the area. Use for 15-20 minutes several times a day.
Are there any specific ergonomic adjustments for workstations to help with CDDD?
Ensure your monitor is at eye level, use an ergonomic chair that supports your lower back, keep your feet flat on the floor, and take regular breaks to avoid prolonged neck strain.
Is it normal to feel tired or fatigued with CDDD?
Chronic pain can lead to fatigue. Managing pain effectively, getting adequate rest, and maintaining a healthy lifestyle can help reduce fatigue.
Can CDDD affect my ability to drive?
Severe CDDD can impair neck movement and reaction times, affecting driving ability. If you experience significant symptoms, it’s advisable to consult your doctor about driving safety.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
