Case Study: Exploration of Spinal Fusion, Explanation of Spinal Hardware, Segmental Spinal Instrumentation, Use of Stereotactic Image-guided Neuronavigational, Fluoroscopy with data interpretation and use of morselized allograft
This patient presented to the Mather Hospital Emergency Room with right-sided lower extremity pain, numbness, and weakness. They were status post recent lumbar fusion surgery at an outside hospital by different surgeons. Since their previous surgery they had noted a new right lower extremity pain and progressive numbness and weakness.
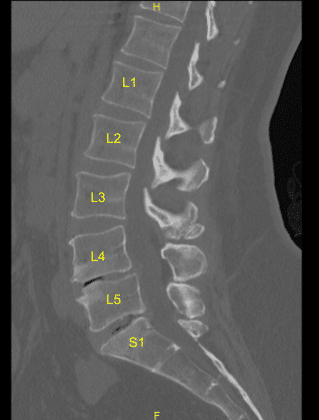
The imaging showed malfunction and suboptimal placement of the right sacral pedicle screw. Surgery was recommended to decompress the lumbar nerve root being impinged by the pedicle screw and stabilize the lumbar spine.
The risks, benefits, alternatives, and potential complications of the surgery were explained to her, and all her questions were answered until no further issues were raised and they provided written informed consent which was placed in the chart.
The patient was brought to the operating room. Their identity was verified. Surgical timeout was performed. General anesthesia was induced. They were intubated by the Anesthesia Service. Respiratory and cardiac monitoring leads were placed. They received preoperative prophylactic IV antibiotics.
They were positioned prone on a Jackson Relton-Hall frame with pressure points carefully padded. Lumbar area was cleaned with chlorhexidine and prepped with DuraPrep solution and sterile drapes were placed in the usual manner. Their right-sided lumbar incision was demarcated. Small dehiscence was noted on the caudal aspect of the left-sided incision. Sterile drapes were placed in the usual manner.
The right-sided incision was opened with a #10 blade scalpel. Hemostasis was obtained with bipolar. I noted a moderate amount of yellow-tinged fluid. Culture swabs were used in the superficial and deep areas and sent to microbiology for aerobic and anaerobic cultures.
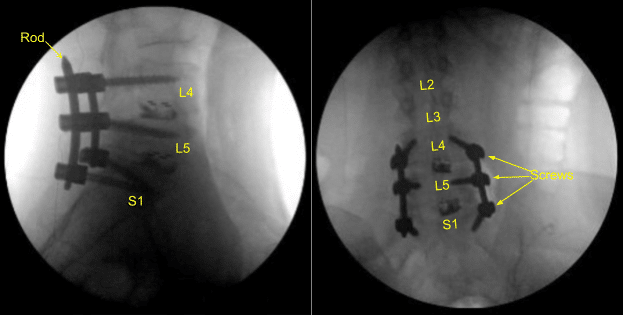
The wound was irrigated clear. Bovie monopolar and Cobb elevators were used to follow the Wiltse approach, divided the fascia and exposed the spinal hardware on the right side. Gelpi self-retaining retractors were placed. The L4, L5 and sacral pedicle screw locking caps were removed with the appropriate driver and anti torque device.
The titanium rod was then removed with curettes and rod gripper. The right S1 pedicle screw was noted to be loose and was removed easily with a screwdriver. The hole was then palpated with a ball-tip feeler probe and was noted to have a ventral breach.
No cerebrospinal fluid was seen to egress from this area. Surgiflo hemostatic matrix was placed. Next, the right S1 pedicle screw starting point was exposed with the Bovie monopolar at the inferolateral aspect of the L5-S1 facet joint and just inferolateral to the sacral ala.
Next, stereotactic frameless image-guided neuronavigation array was placed in the left posterior superior iliac crest, after infiltrating with local anesthesia creating a #15 blade stab incision. The Schanz pins were gently tamped into the crest with a mallet and neuronavigation array was affixed. The patient was draped sterilely.
Intraoperative CT scan was obtained, and data was transferred to the neuronavigation computer and accuracy was verified. Neuronavigation techniques were used to cannulate the right-sided first sacral segment which was then palpated for breaches and measured at the depth of 35 mm. A 6.0 mm navigated tap was used to thread the cannulation. It was again palpated for breaches and a 7.5 x 35 mm titanium pedicle screw was placed with good bony purchase and tightness.
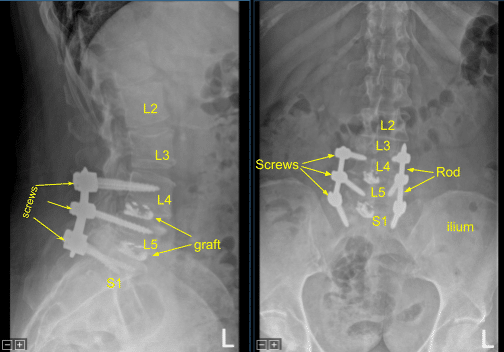
Next, the patient was re draped and a second intraoperative CT scan was obtained showing correct positioning of this pedicle screw. Neuromonitoring signals were stable throughout. Next, the L5-S1 transverse process and ala were decorticated with a high-speed drill for the arthrodesis after exploring the fusion and failing to identify bony arthrodesis and bone graft.
Again, a precut-precontoured titanium rod was placed across the pedicle screw tulips from L4 to S1 and secured with the locking caps which were tightened with a torque and anti torque device. Morselized bony allograft was placed across L5-S1 on the right side for the arthrodesis.
The wound was irrigated copiously with sterile saline throughout the procedure. Hemostasis was confirmed with the Aquamantys and bipolar. A medium size Hemovac was tunneled in a subfascial manner and secured to the skin with a 3-0 nylon suture.
Next, the fascial closure was performed in watertight fashion with 0 Vicryl sutures. Exparel long- acting local anesthetic was infused into soft tissues. Vancomycin powder was applied. The subdermal layer was closed with 2-0 Vicryl sutures and the skin was reapproximated with surgical staples.
The Schanz pins were removed from the iliac crest. Surgiflo hemostatic matrix was applied, and the stab incisions were closed with a single surgical staple each.
The small dehiscence on the left-sided incision was debrided and the skin was reclosed. All the incisions were cleaned and dried sterilely, and dressings were applied in a sterile manner. A Hemovac canister was applied with suction. C-arm unit was draped sterilely and used for AP and lateral fluoroscopic confirmation of correct hardware and instrumentation positioning, specifically the rod placement.
The patient was then turned supine on the cart, extubated uneventfully and transported to the recovery room in stable condition. At the end of the case, all sponge counts, needle counts, and instrument counts were correct. The patient tolerated the procedure well.
The patient followed up two weeks after the surgery and then continued to follow up in 4, 6, 8, 12, 24 weeks. In their last office visit the patient stated they were at home and able to do their usual activities. They also stated that physical therapy was going well.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
