Case Study: Right Custom Knee Replacement in a 59-year-old male
A 59 years old software engineer presented to our office with complaints of right knee joint crepitus associated with pain. The patient stated the pain started insidiously 4 years ago and had significantly worsened. He was unable to perform his daily activities and the pain interferes with his sleep.
The patient describes the pain as a dull ache which was located on the right inner side of the knee joint. The pain was better with rest and exaggerated with activities such as walking, twisting, turning, going up and down the stairs, kneeling or bending. He described as associated stiffness in the knee joint which was especially worse after sitting for prolonged periods of time.
The pain was moderate to severe in intensity. The patient denied any radiation of the pain. He had previously tried heat pads and received 3 cortisone injections from an outside physician. He also reported trying physical therapy and home exercise program with no significant relief.
Secondary to pain in the right knee, he had recently changed his working hours. He found it difficult sitting on a chair for a prolonged time. He had no played golf for the past 7 months and felt sad not being able to join his friends at the game. He was consulting today for discussing options for surgery.
He was moderately overweight, well-nourished and well-formed. His past medical history was positive for well-controlled diabetes on oral hypoglycemic agents. He was also on medications for dyslipidemia and benign prostate hypertrophy. He was a former cigar smoker and had alcohol occasionally.
His physical examination revealed tenderness on medial and lateral joint lines and patellar facets. There was an absence of any swelling, erythema and local rise of temperature. The range of motion was terminally restricted secondary to pain. Examination of the contralateral knee revealed mild osteoarthritic changes.
The examination of the bilateral hip and ankles was normal. Anterior and posterior drawer test, Lachman test, valgus and varus stress test, pivot shift and dial test were negative. The power and sensory examination of the bilateral lower extremities was unremarkable.
Imaging revealed severe bilateral Osteoarthritis of the knee. The patient was symptomatic mainly in the right knee, he was advised a custom total knee replacement. Risks, benefits and potential complications were all discussed with the patient in detail. He was highly motivated to get back to his baseline and opted for custom total arthroplasty.
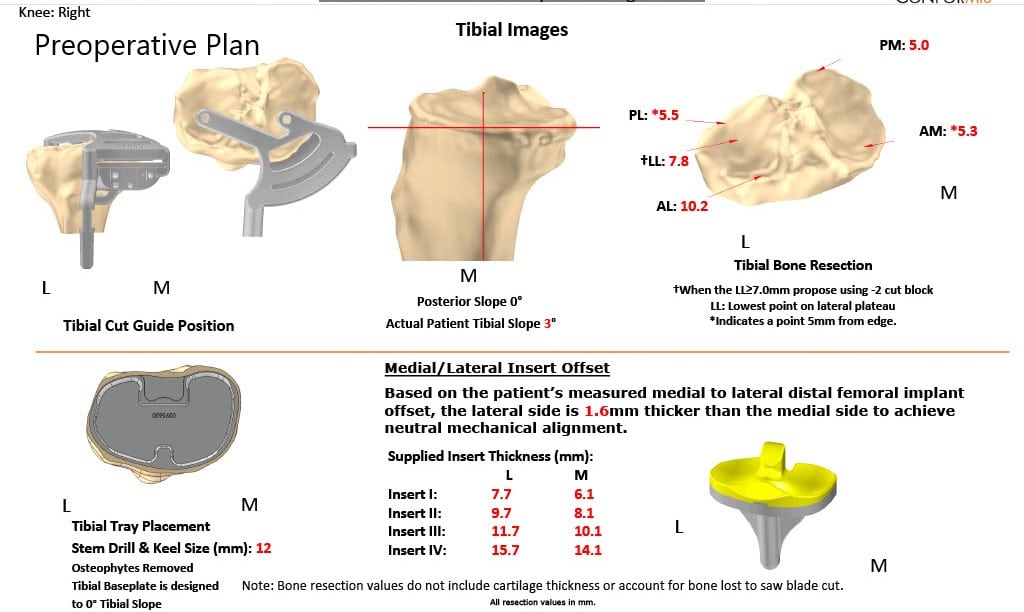
As a part of the preparation of the custom implants, a preoperative CT was obtained a few weeks prior to surgery. The results were utilized to create 3D images of the patient’s unique anatomy. Customized implants were then made along with disposable custom instruments. A preoperative plan was formalized to aid the surgery in precision cuts and alignment.
Preoperative X-ray showing AP view of the bilateral knee joints.
OPERATION: Right total knee arthroplasty.
IMPLANTS USED: Customized remodeled femoral component with a customized tibial component with a size 6 polyethylene.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room. After obtaining informed consent, signing the correct surgical site, the risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure.
The patient was then anesthetized and the right lower extremity was then draped and prepped in the usual sterile manner. An Esmarch was used to exsanguinate the limb, and the straight incision was used for the arthrotomy. Skin and subcutaneous tissues were incised. The medial parapatellar arthrotomy was then performed.
The tibial dissection was then made using the customized tibial guide. The femoral distal cutting guide was used to make the distal cut and chamfer cuts were made using the chamfer cutting guide. The notch cut was then performed.
Attention was then turned towards the patella. The patellar resection was then made and the drill holes were made in the patella. The trial patella was then placed into position. The laminar spreader was used medially and laterally and the remainder of the meniscus and the cruciates were then divided.
The flexion and extension gaps were then checked. The tibial punch was then made and the lug holes were then made in the tibia. The trial femur was placed into position followed by the trial tibia. The poly was placed into position. The knee was then trialed through a full range of motion. The extension was excellent. Complete flexion was obtained. Patellar tracking was excellent.
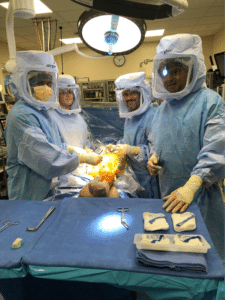
The trial components were then removed. A thorough lavage was performed. An injection was given. The femur was cemented into position. Excess cement was removed.
The tibia was cemented into position. Excess cement was removed. Poly was then placed into position. The knee was then reduced and held with full extension with a bump under the ankle.
The patella was then cemented into position and was held in position with a patellar clamp.
After the cement hardened, the patella clamp was removed. The medial parapatellar arthrotomy was closed.
‘Cutaneous tissue was closed. Subcuticular tissue was closed. The skin was closed using staples.
Sterile dressing was then applied over the wound and the tourniquet was then released. The patient was transferred to the postoperative care unit in stable condition.
Postoperative images showing AP and oblique views of the right knee.
The patient was able to bear weight on the right leg on the same day of the surgery. The pain was managed with oxycodone and acetaminophen. Aspirin was given for deep vein thrombosis prophylaxis. The patient was compliant with physical therapy and home exercise program.
He successfully concluded his physical therapy in 3 months. He was ambulatory without any support and demonstrated pain free full range of motion. He brought a picture of himself playing golf. He was back to his previous routine and was happy with the outcome of the procedure.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.