Adjacent Segment Disease after Cervical Fusion
If neck discomfort becomes intense enough to interfere with daily routines or is accompanied by swelling, sensitivity, or redness, it’s crucial to obtain medical help.
At Complete Orthopedics, our proficient spine physicians are experts in managing cervical spine and neck discomfort through surgical and non-surgical approaches. We assess symptoms, pinpoint the issue, and recommend appropriate treatments, including surgery if needed.
We serve New York City and Long Island and collaborate with six hospitals, providing leading-edge cervical spine surgery and extensive orthopedic services. You can schedule a consultation with our orthopedic surgeons online or via phone.
Explore common reasons for neck pain and the available treatment options, including when opting for surgery is most recommended.
Overview
Adjacent segment degeneration is the appearance of degenerative changes with or without clinical symptoms in the level up or below the fused cervical segment. Adjacent segment disease may lead to symptoms of radiculopathy or myelopathy. The initial treatment of adjacent level disease is conservative but a fusion surgery of the adjacent level may be needed in the case of continued symptoms.
The vertebrae are stacked upon each other connected by intervertebral disks and facet joints. Additionally, various ligaments provide stability to the spine during motion. The fusion of a segment may result in increased stress at the segment adjacent to the fused vertebrae as the adjacent segment tries to compensate for the loss of motion.
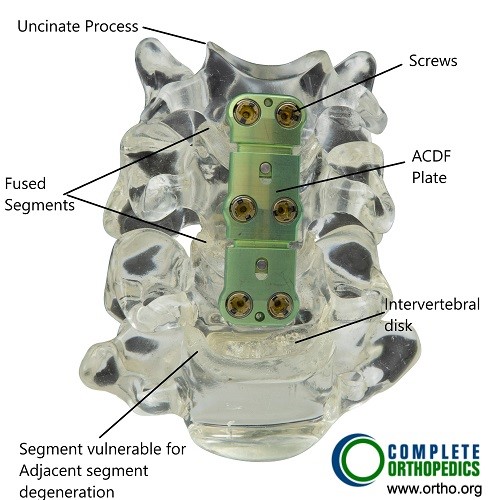
Bone model showing ACDF.
The increased compensatory motion and stress may cause accelerated intervertebral disc degeneration in the adjacent segment. The increased pressure in the adjacent segment may cause disc herniation and loss of disc height. As a result, there may be degenerative changes in the facet joint (facet joint syndrome) and formation of bone spurs.
The degenerative changes may cause cervical canal stenosis which may present as cervical radiculopathy or cervical myelopathy. The adjacent segment disease has also been attributed to damage to ligament and muscles during anterior cervical decompression surgery.
Key Factors Contributing to ASD
Increased Mechanical Stress: After fusion, the adjacent segments experience greater motion and stress.
Pre-existing Degeneration: If the adjacent segments were already showing signs of degeneration before the surgery, they are more likely to develop ASD.
Surgical Technique: The method and extent of the fusion can influence the likelihood of developing ASD.
Patient Factors: Age, activity level, and overall health can also affect the risk of ASD.
The adjacent segment degeneration
is more common in the lower segments of the cervical spine, especially C5-C6. Female patients and patients under the age of 60 years are more susceptible for adjacent level degeneration after ACDF (anterior cervical decompression and fusion). Similarly patients with a history of smoking and pre-existing degenerative changes in the adjacent segments are at an increased risk of accelerated degeneration.
The chances of adjacent level degeneration increase after 10 years of ACDF surgery. The symptoms of adjacent level degeneration depends upon the level of encroachment of the space occupied by the neural structures.
Symptoms of ASD
The symptoms of ASD can be quite similar to the original spine issues that led to the need for cervical fusion. Common symptoms include:
- Neck Pain: Persistent or worsening pain in the neck.
- Radiating Pain: Pain that radiates from the neck into the shoulders, arms, or upper back.
- Stiffness: Reduced range of motion in the neck.
- Neurological Symptoms: Numbness, tingling, or weakness in the arms or hands due to nerve compression.
- Headaches: Pain at the base of the skull or headaches that can radiate to the front of the head.
Diagnosis
The diagnosis of adjacent segment disease in a patient with a prior history of ACDF is made after thorough history and physical examination. The surgeon may look for signs of motor and sensory weakness in all the four limbs. The physician may also inspect the walking pattern of the patient. Special tests may be done to localize the segment involved in the symptoms.
Radiological examinations include an X-ray as the first investigation which may be followed by an MRI or a CT scan. A CT scan provides a more detailed image of the bony structures as compared to an X-ray. A CT scan is particularly helpful to look for ossification of the posterior longitudinal ligament and formation of a false joint in the fused segment. The MRI provided a detailed image of the soft tissue structures including the degree of compression of the neural structures.
The investigations are aimed to diagnose and also differentiate other similarly presenting pathologies such as infection, degenerative changes at a non adjacent segment, pseudoarthrosis, etc.
Treatment
Non-Surgical Treatments
Medications: Pain relievers, anti-inflammatory drugs, and muscle relaxants can help manage symptoms.
Physical Therapy: Tailored exercises and therapies can help strengthen the neck muscles, improve flexibility, and reduce pain.
Lifestyle Modifications: Changes in daily activities, ergonomic adjustments, and weight management can reduce stress on the spine.
Injections: Corticosteroid injections can reduce inflammation and provide temporary pain relief.
The operative management is extension of the ACDF construct to the adjacent segment involved. A total cervical disc replacement may also be done in a case of adjacent segment degeneration.
Conclusion
Adjacent Segment Disease (ASD) is a potential complication following cervical fusion surgery, resulting from increased stress and movement in the spinal segments adjacent to the fused area. Symptoms can include neck pain, radiating pain, stiffness, and neurological issues. Diagnosis involves clinical evaluation and imaging studies, while treatment ranges from non-surgical options like medications and physical therapy to surgical interventions if necessary.
Understanding the risk factors, symptoms, and treatment options for ASD can help patients and healthcare providers manage this condition more effectively. With ongoing research and advancements in surgical techniques, the aim is to reduce the incidence of ASD and improve outcomes for patients undergoing cervical fusion. By staying informed and proactive, individuals can better navigate their treatment journey and maintain a higher quality of life.
Do you have more questions?
What is the typical timeline for the development of ASD after cervical fusion?
Typically, ASD can manifest anywhere from 2 to 10 years post-surgery. However, it’s crucial to understand that this timeline can vary significantly based on individual factors such as the patient’s age, the extent of the initial surgery, and their overall spinal health.
Are there specific types of cervical fusion that are more likely to result in ASD?
Yes, multi-level fusions are more prone to leading to ASD compared to single-level fusions. This is because more segments are immobilized, increasing the biomechanical stress on the adjacent unfused segments.
What are the risks of not treating ASD if symptoms are mild?
Mild symptoms can gradually worsen if left untreated, potentially leading to more severe pain, loss of function, and neurological deficits. Early intervention can help manage symptoms more effectively and prevent progression.
How is the decision made between non-surgical and surgical treatment for ASD?
The decision is based on the severity and progression of symptoms, the degree of degeneration observed in imaging studies, and the patient’s overall health and lifestyle. Typically, we start with conservative treatments and consider surgery if those measures fail to provide adequate relief.
Are there any lifestyle changes that can help manage ASD symptoms?
Absolutely. Maintaining a healthy weight, avoiding heavy lifting and high-impact activities, practicing good posture, and quitting smoking are all beneficial. Additionally, ergonomic adjustments at work and home can help reduce stress on the spine.
How effective are pain medications in managing ASD?
Pain medications, including NSAIDs and muscle relaxants, can be effective in managing pain and inflammation but should be part of a broader treatment strategy that includes physical therapy and lifestyle modifications.
Is it safe to engage in physical activities and sports after cervical fusion surgery?
Low-impact activities such as swimming, walking, and cycling are generally safe and encouraged. However, high-impact sports and activities that put significant strain on the neck should be avoided. Always consult your surgeon before resuming any physical activity.
What role do ergonomic adjustments play in managing ASD?
Ergonomic adjustments are crucial. Proper workstation setup, supportive chairs, and correct posture during daily activities can significantly reduce the mechanical stress on the cervical spine, helping to manage ASD symptoms.
Can chiropractic care help with ASD?
While some patients find relief from chiropractic care, it is essential to approach this cautiously. Manipulations should be gentle, and it is crucial to consult with your surgeon before undergoing chiropractic treatment to ensure it’s safe for your specific condition.
How often should follow-up appointments be scheduled after cervical fusion surgery?
Follow-up appointments should be scheduled immediately post-surgery, at six weeks, three months, six months, and annually thereafter, or more frequently if there are symptoms suggestive of ASD.
Can ASD be detected early through regular imaging?
Yes, regular imaging such as X-rays, MRIs, or CT scans can help detect early degenerative changes in adjacent segments, allowing for earlier intervention and better management of the condition.
Are there any genetic factors that increase the risk of developing ASD?
While there is no specific genetic marker for ASD, individuals with a family history of degenerative disc disease or other spinal conditions may be at a higher risk.
How does the recovery process from ASD surgery compare to the initial cervical fusion surgery?
The recovery process for ASD surgery is generally similar to the initial surgery, involving a period of immobilization followed by rehabilitation. However, the specifics can vary based on the extent of the surgery and the patient’s overall health.
What are the potential complications of surgery for ASD?
Potential complications include infection, blood loss, nerve damage, and the risk of further degeneration at other adjacent segments. Nonunion or improper healing of the fusion site is also a concern.
Can wearing a cervical collar help in managing ASD?
Wearing a cervical collar can provide short-term relief by stabilizing the neck and reducing movement. However, long-term use is not recommended as it can lead to muscle atrophy and decreased neck strength.
Are there any new advancements in technology or techniques that might reduce the risk of ASD?
Yes, advancements such as artificial disc replacement and motion-preserving surgical techniques aim to maintain more natural movement in the spine, potentially reducing the stress on adjacent segments and lowering the risk of ASD.
How does age affect the risk and progression of ASD?
Older age is associated with increased risk due to the natural degenerative processes of the spine. Older patients often have pre-existing degenerative changes, which can accelerate the development and progression of ASD.
What kind of support systems are beneficial for patients dealing with ASD?
Support systems including physical therapy, patient education programs, counseling, and support groups can help patients manage symptoms and improve their quality of life. A multidisciplinary approach often yields the best outcomes.
Can nutritional supplements help in the management of ASD?
Nutritional supplements like glucosamine and chondroitin may support joint health, although evidence of their efficacy varies. Omega-3 fatty acids may help reduce inflammation. Always consult with your doctor before starting any supplements.
How does obesity impact ASD?
Obesity increases the mechanical load on the spine, which can accelerate degeneration and worsen ASD symptoms. Weight management through diet and exercise is an important aspect of treatment.
What is the role of alternative therapies like acupuncture in managing ASD?
Acupuncture can provide pain relief for some individuals and may be a useful adjunct to conventional treatments. It’s important to discuss this with your healthcare provider to ensure it’s safe and appropriate for your condition.
Can psychological factors impact the experience of ASD symptoms?
Yes, psychological factors such as stress, anxiety, and depression can exacerbate the perception of pain and impact overall health. Addressing these factors through counseling and stress management techniques is important.
How can patients prepare for potential future ASD when planning their initial cervical fusion surgery?
Patients should discuss the potential for ASD with their surgeon and consider surgical options that minimize stress on adjacent segments. Engaging in pre-surgical physical therapy and adopting a healthy lifestyle can also help.
What are the long-term outlooks for patients who develop ASD after cervical fusion?
The long-term outlook varies but can be positive with appropriate management. Many patients manage symptoms effectively with conservative treatments, and surgical intervention can restore function and alleviate pain when necessary. Regular follow-ups and a proactive approach to spine health are key.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
