Case Study: Custom Left Knee Replacement in a 40 year male
A 40 year old male presented to our office with complaints of left knee pain for the past 5 years. The patient stated he sustained a left knee injury playing soccer 11 years ago for which he was managed conservatively. He subsequently had multiple knee injections and underwent physical therapy but with only temporary relief.
The patient works as a welder in a construction firm. His work involves frequent bending, kneeling and twisting. Recently since the past 1 year the pain had limited his work output. He experienced moderate to severe pain on walking, standing for long and activities requiring him to bend or kneel.
Additionally, he was unable to play with kids and walk his dog since the past few months. The patient was a non smoker and had a past medical history of hypertension and depression, both well controlled with medications. His past surgical history included an appendectomy and laparoscopic cholecystectomy. He was currently taking hydrochlorothiazide 12.5 mg and sertraline. He had drug allergies to sulfamethoxazole and trimethoprim.
On his physician examination, his gait was found to be antalgic with reduced stance phase on the affected side. Patellar tap was positive on milking the suprapatellar pouch suggesting mild knee effusion. Medial joint line and medial patellar facet tenderness was positive. Anterior drawer, posterior drawer, lachman test, valgus and varus stress test were negative.
His imaging studies revealed osteoarthritic changes in the left knee. After careful consideration of lifestyle limiting knee pain and his medical condition, he was advised a custom left knee total replacement. Risks, benefits and alternatives were discussed at length with him. He was motivated to get back to his daily routine without knee pain.


Preoperative X-ray of the left knee showing AP and lateral views
Several weeks before the surgery, a CT scan of the left knee was obtained. A unique 3D reconstruction was obtained from the data. This data was utilized to create unique patient specific implant. Additionally, disposable custom instruments unique for the patient’s knee were constructed. Custom implants and instruments ensured the best outcome of the procedure. A preoperative plan was made specific for the patient’s knee to preplan the bone cuts and offsets.
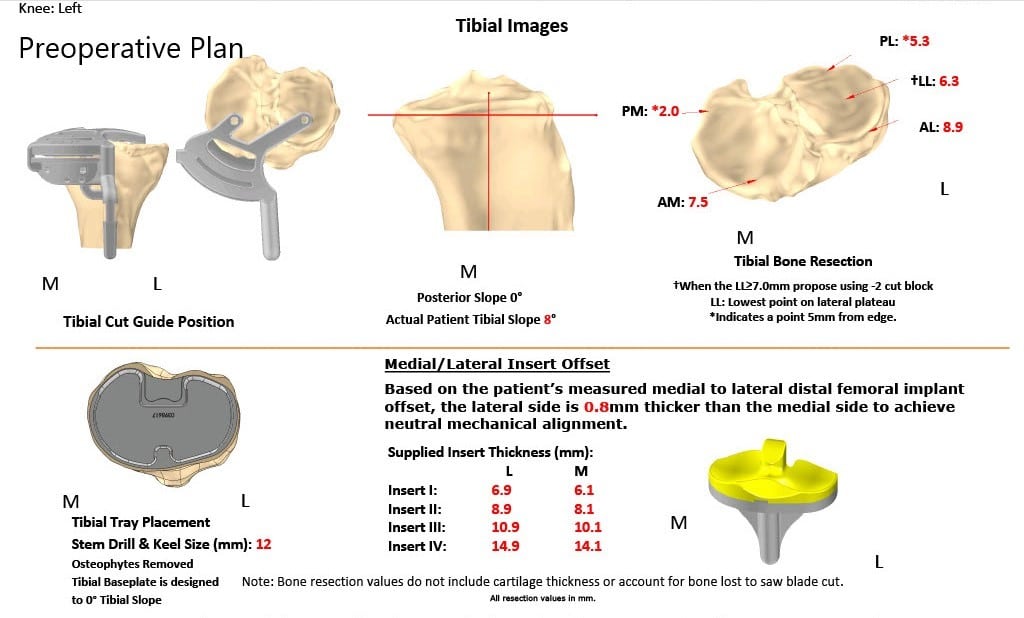
Complete Orthopedics patient-specific surgical plan for a custom left knee replacement in a 40-year-old male.

Complete Orthopedics patient-specific surgical plan for a custom left knee replacement in a 40-year-old male (scan 2)
Preoperative surgical plan outlining bone cuts and offsets
The patient underwent customized left knee arthroplasty
Implant used: Custom femur with a custom tibia and patella (38mmx8.5mm) with 10-mm polyethylene insert.
The patient was brought to the operating room after obtaining informed consent and signing the correct surgical site. The risks, benefits, alternatives were extensively discussed with the patient prior to the procedure. The anesthesia was obtained by the anesthesiologist. A tourniquet was placed over the left thigh, and the left lower extremity was prepped and draped in the usual sterile manner.
A straight incision was used for the arthrotomy. Skin and subcutaneous tissues were incised. Medial parapatellar arthrotomy was then performed. The tibial resection guide was then placed into position after exposure of the tibia, and the tibial resection was then made and was then checked. Attention was then turned towards the femur, and the distal cut was then performed using a jig.
The anterior-posterior chamfer cuts were then made using the respective cutting guides. The notch cut was then performed. The laminar spreaders were used medially and laterally, and the remainder of the meniscus and cruciate were then divided. The tibia was then prepared. A gap balancing was performed and was found to be perfect.

Attention was then turned to the patella. The patella was then resected, and drill holes were made in the patella. Trial patella was then placed into position. Trial femur was then placed into position followed by the trial tibia.
Poly was placed into position. The knee was then trialed through a full range of motion. The patellar stability was excellent. The full range of the knee was then obtained.
Trial components were then removed. The femur was cemented into position. Excess cement was then removed. The tibia was cemented into position. Excess cement was then removed. Poly was placed into position. The knee was then reduced and held in full extension with a bump under the ankle.
The patella was then cemented into position. Excess cement was removed and was held with a patellar clamp. The clamp was then removed after cement hardened. Thorough lavage was given.
The injection was given. Medial parapatellar arthrotomy was closed, and the remainder of the wound was closed in layers. Sterile dressing was applied over the wound. The tourniquet was deflated, and the patient was transferred to the postoperative care unit in stable condition.


Three months postoperative X-ray of the left knee showing AP and lateral images.
The patient was able to walk the same day of the surgery with support. The pain was well controlled with medications. The staples were removed uneventful. He underwent a regime consisting of home exercise program and physical therapy. He was prescribed aspirin 325mg BID for three months for deep vein thrombosis prophylaxis.
After three months, the patient had successfully completed his physical therapy and discontinued aspirin. He was happily back to baseline activities. He was able to play with his kids and walk his dog without any discomfort. A week weeks later he was able to return to his work and reported no discomfort. The patient stated the results from surgery exceeded all his expectations.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
