Case Study: Custom Right Total
Knee Arthroplasty – 62-year-old male
A 62-year-old male presented to our office as a new patient with complaints of bilateral knee pain (Right greater than left) for the past 5 years. The patient used to work as a Correction Officer for the NYC Department of correction. The patient stated that he sustained a slip and fall injury 5 years ago injuring his bilateral ankles, shoulders, and knees.
He was previously being treated for right knee pain by another orthopedic doctor in the form of cortisone injections and physical therapy but with no relief. The patient stated that the pain was getting worse over time despite conservative management in the form of physical therapy, heat pads, pain medications, and knee injections. The pain was disrupting his sleep at night and he felt anxious climbing stairs or walking fast.
The patient stated he was under emotional turmoil because of not being able to carry out his daily activities without pain and being unable to play with his grandkids. The patient was assessed at our office with a thorough physical exam. The patient was a nonsmoker and obese with a BMI of 31 with no other medical conditions.
Physical examination revealed genu varus deformity and mildly swollen right knee joint. There was marked joint crepitus throughout the range of motion with moderate medial and lateral joint line tenderness and patellar facet tenderness. Imaging studies revealed marked narrowing of the medial joint compartment and patellofemoral joint compartment with moderate osteophyte formation.


Pre-Operative AP and Lateral X-Ray views of the right knee (standing)
After thorough consideration of the patient’s medical conditions and needs, he was found to be a candidate for total right knee arthroplasty. He was offered a custom knee replacement system.
Risks, benefits, potential complications, and alternatives were thoroughly discussed with the patient. The patient agreed for the procedure and was motivated to get back to his job.
A custom knee replacement system has benefits of patient-specific implants and instruments.
A preoperative CT scan of the patient’s knee, including the hip and ankle, was obtained a few weeks prior to the surgery. The images were used to construct a 3D model of the patient’s knee for assessment of the anatomy and biomechanics. The data was then used to construct unique patient-specific implants and instruments. Custom implants and instruments ensure bone and soft tissue preservation with a more natural feeling knee.
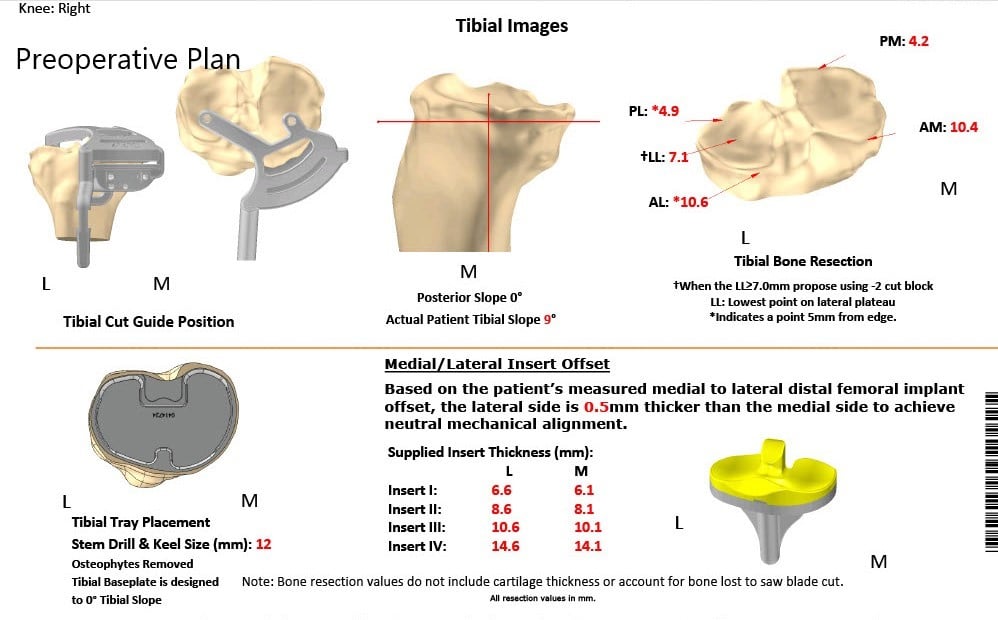
Complete Orthopedics patient-specific surgical plan for a custom-right total knee arthroplasty: 62-year-old male.
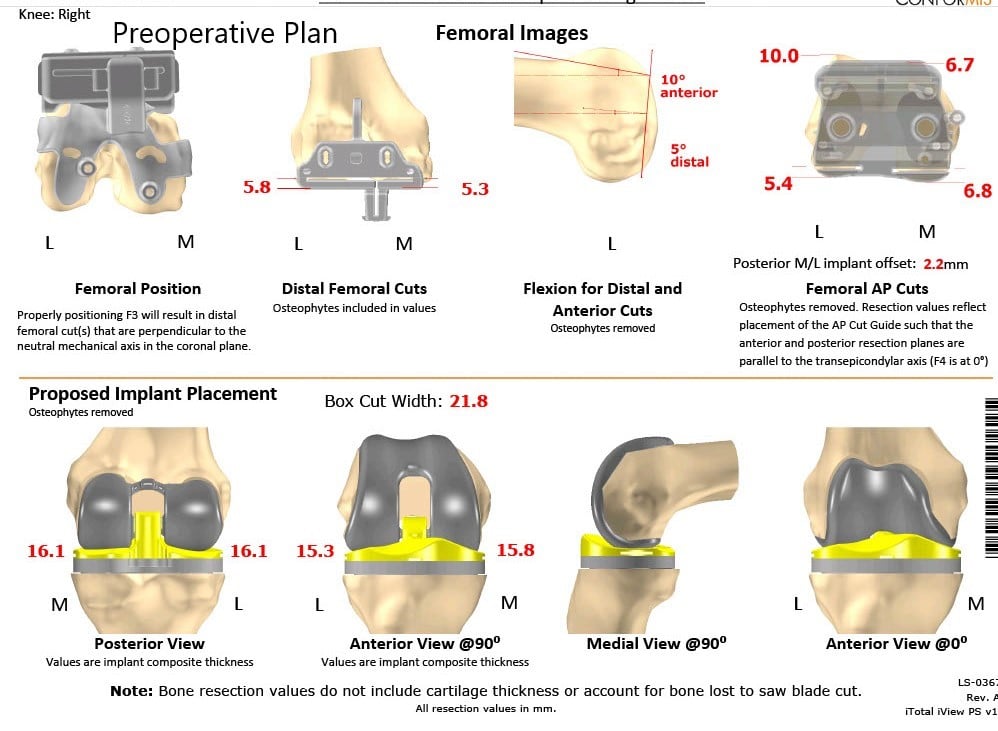
Complete Orthopedics patient-specific surgical plan for a custom-right total knee arthroplasty: 62-year-old male (scan 2)
The patient underwent a custom right total knee arthroplasty.
Implants used: 8 mm posterior stabilized polyethylene with tibial tray, femoral implant 32 mm,
6 mm thickness polyethylene with an 8 mm polyethylene insert.
The patient was brought to the operating room and was definitively positioned. Anesthesia was obtained by the anesthesiologist. The right knee was then draped and prepped in a sterile manner. A straight incision was placed over the knee joint after exsanguinating the extremity.
Skin and subcutaneous tissues were incised. Medial parapatellar arthrotomy was performed. Attention was then turned towards the femur. The distal femoral resection guide was placed into position. The distal resection was made. The anterior and posterior chamfer cuts and the oblique cuts were then made using the resection guide.
Attention was then turned towards the tibia. The tibial resection was performed. The alignments were checked with the knee extended. The patella was everted. Patellar resection was performed. Drill holes were made in the patella. Trial patella was then placed into position.
Attention was then turned towards the femur after balancing the knee and after removing the ACL and remainder of the curciates. The notch cut was performed. The trial femur was placed into position. Trial tibia was placed into position. Poly was placed into position. A full extension of the knee was achieved. The knee had full flexion intraoperatively. The patellar tracking was excellent.
The trial components were then removed. Injection was given for postoperative pain control. The femur was cemented into position. Excess cement was removed. The tibia was cemented into position. Excess cement was removed. Poly was placed into position, and the knee was then reduced and held in full extension with the bump under the anchor.
Patella was then cemented into position. Excess cement was removed. After the cement hardened, the patellar clamp was removed. A thorough lavage was given. Medial parapatellar arthrotomy was closed with Vicryl and Stratafix. The cutaneous tissues were closed with Vicryl, subcuticular tissues were closed with 2-0 Vicryl and the skin was closed using staples.


Postoperative X-ray of the patient’s right knee showing AP and lateral views
The patient was able to bear weight with support the same day of the surgery. On subsequent visits, his wound was found to be free of any infection and skin staples were removed after wound healing. He demonstrated an excellent range of motion of the knee in subsequent visits.
The patient was compliant with physical therapy and home exercise program. He demonstrated a full range of motion which was pain-free at a 3 month follow up. He stated he was able to drive a car, climb stairs and play with his grandchildren without the anxiety of precipitating the pain. The patient stated he experienced an increased quality of sleep and was able to get back to his work as a correction officer. The patient has now returned to the activities he enjoyed before the disease process.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
