Revision Total Knee Replacement Surgery
If knee pain worsens, interferes with daily tasks, or is accompanied by swelling and redness, it is crucial to consult a healthcare professional. At Complete Orthopedics, our expert team specializes in treating knee meniscus tears with customized treatment plans and surgical options. We prioritize understanding your symptoms, diagnosing the underlying causes, and recommending the most suitable treatments or surgeries.
Our clinics are conveniently located throughout New York City and Long Island, and we are affiliated with six top hospitals, ensuring you receive excellent care for knee issues. Book an appointment with one of our orthopedic surgeons either online or by phone. Learn about the causes and treatments for knee pain and find out when surgery might be necessary.
Overview
Revision total knee replacement is the surgical procedure to replace the components of a prior knee replacement. Primary total knee replacement is one of the most common surgeries performed by orthopaedic surgeons. Common indications for a knee replacement include arthritis caused by primary osteoarthritis, rheumatoid arthritis, psoriatic arthritis, and secondary arthritis.
Total knee replacement offers excellent pain relief and restores prior mobility. Total knee replacement is one of the most successful surgeries of the twentieth century in the history of modern medicine.
On average, a knee replacement surgery may last for 15-20 years or even more. However, due to various biological and mechanical reasons, the parts may fail. Failure requires surgery which involves removal of the prosthesis and it’s replacement with a new prosthesis.
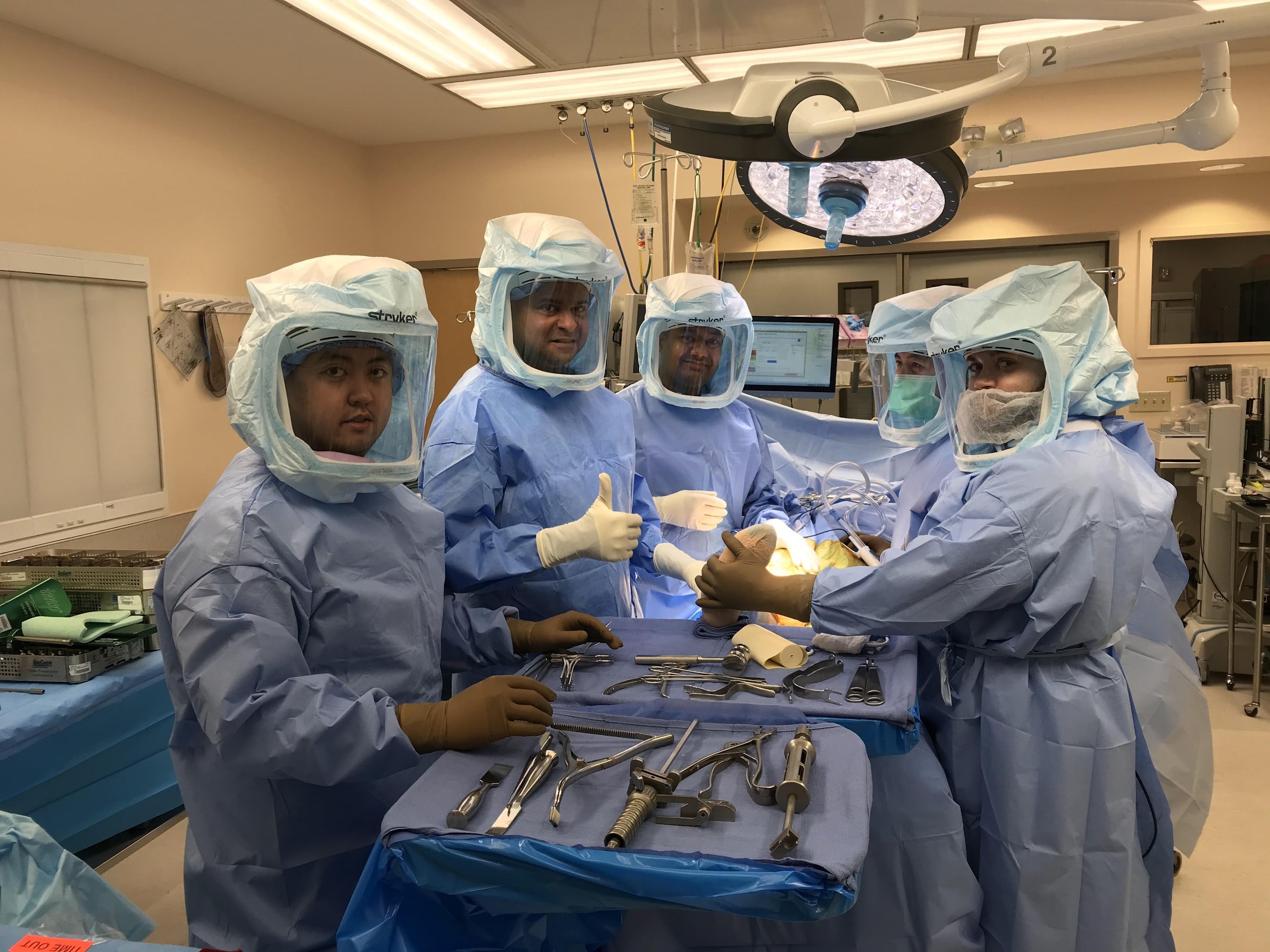
Revision knee replacement surgery is usually far more complex surgery than a primary total knee replacement. Revision surgeries require extensive planning and may require special implants and tools. The operating surgeon requires mastery of his/her technique to conquer the difficulties encountered in revision surgery.

Removed articulating cement spacer and reamers.
The ultimate goal of the revision surgery remains the same as that of the primary replacement. The aim is to provide pain-free mobility so that the patients can return to the activities they enjoy.
Causes of failure
Both mechanical and biological factors play a role in the failure of the surgery. The primary knee replacement may fail over the years or due to sudden injury/infection.
- The infection of the artificial knee joint is one of the commonest causes of early failure. The metallic and plastic parts may serve as growth surfaces for infectious agents. The surfaces are inaccessible for the body’s immune system.
- Aseptic loosening is the most common cause of failure of components many years after the surgery. There is micromotion between the interface of bone cement, bone surface, and the metallic component which causes loosening of the parts.
- There may be a generation of wear particles due to micromotion. The body’s defense system tries to get rid of the wear and tear particles. But in the process, the cells may also destroy the normal bone and cause loosening of the implant known as osteolysis.
- Fractures of the bones in the region of the implant may require revision of the implant. The type of surgery depends upon the location of the fracture.
- Instability of the artificial joint may be due to inadequate fixation of the implants or improper positioning of the implants. There may be laxity of the ligaments on the inner or outer side of the knee causing instability.
- Hypersensitivity to the metal parts may require revision with patient-friendly implants.
- Scar tissue may form on the undersurface of the quadriceps tendon causing a clunk on straightening the knee.
- Certain patient factors play a role in implant failure. Young patients with an active lifestyle may require revision earlier than the older age groups. Obese patients and patients with a history of prior knee surgery have a greater risk of infection.
Symptoms
The symptoms of implant failure may be knee pain or swelling in the knee. The pain may be more pronounced on weight-bearing in case of mechanical failure. The pain may be associated with fever and malaise in case of joint infection.
There may be associated stiffness of the knee joint. The patient may walk with a limp secondary to pain or instability. The skin overlying the joint may be warm and red in case of joint infection.
Diagnosis of failure
The patients with implant failure require a thorough investigation of the cause of failure. The physician may acquire a detailed history regarding the symptoms. The physician will also test the joint in various ranges of motion and examine the gait of the patient. The physician will look for any signs of infection and instability.
Radiological examination is done in the form of an X-ray to look for the component position, loosening, and alignment. CT scan may provide a detailed view regarding the femoral rotation and the component position. MRI studies may be helpful to detect bone loss. Bone scans are helpful to detect loosening and infection.
Aspiration of the knee joint is done to investigate the source of infection or rule out the infection. Blood investigations may also be done to look for markers of infection.
Surgery
The surgery is planned preoperatively according to the condition of the implant and the bone. The exposure and the surgery time is usually longer than the primary knee replacement surgery.
In the case of infection, the type of surgery depends upon the severity and time of onset of the infection. The surgery may be divided into two steps or done in a single step.
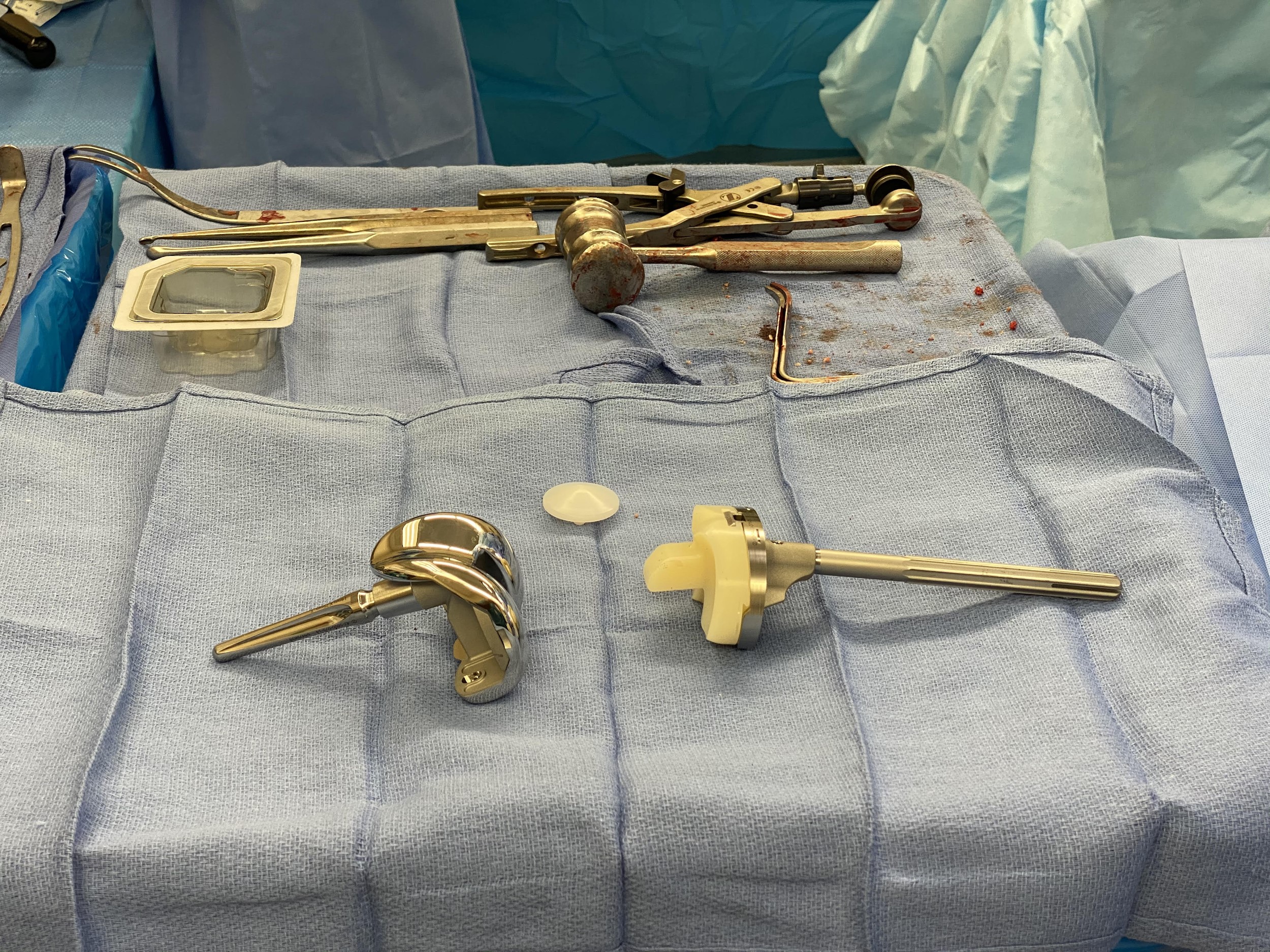
Revision knee replacement implant (semi – constrained with a long stem).
In a two-step approach, during the first surgery, the infected implants are removed. The joint is thoroughly washed and debrided. A prosthesis made of bone cement is inserted with antibiotics.
The patient is given intravenous antibiotics and after a period of a few weeks, definite fixation is undertaken. The joint aspiration is repeated before the definite surgery.
In the case of recent onset infection, the joint is washed thoroughly and only the plastic parts are replaced. In some cases, the infected prosthesis is removed and replaced with a new one in the same setting.
Periprosthetic fractures may require the use of special long stem implants. The type of surgery depends upon the level of the fracture.
In case of failure of the plastic component, only the plastic component may require revision. The revision surgery may require bone grafts or special cones to account for bone loss during the extraction.

Cementing of the femoral component.
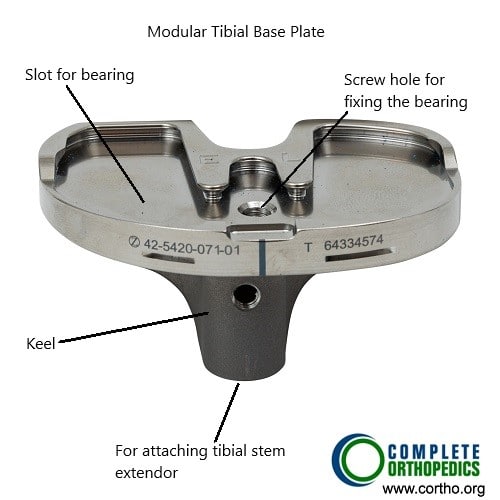
Modular Tibial Component

Modular femoral component
The above images show modular femoral and tibial components. The modular components allow the surgeon to make intraoperative adjustments to achieve greater stability. There are provisions to attach stems to the components as well as adding bone augments to account for bone loss encountered during surgery.
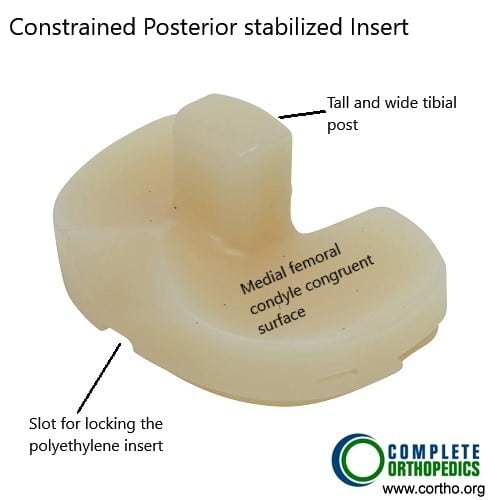
Constrained posterior stabilized polyethylene insert
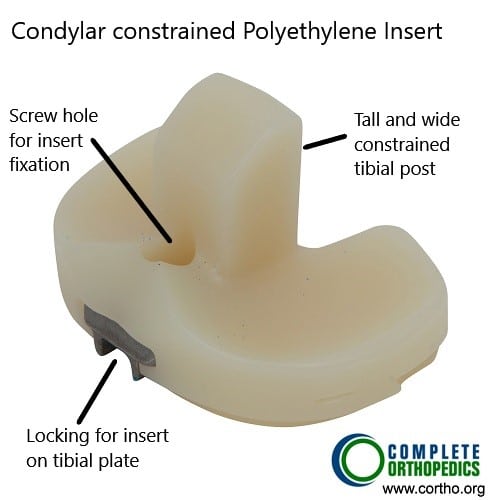
Condylar constrained Polyethylene insert
Constrained polyethylene inserts in the images above utilize a tall and wide tibial post to provide side to side and rotational stability. These inserts are usually used with femoral and tibial components with stems. The stems dissipate the additional stress arising from the constrained construct.
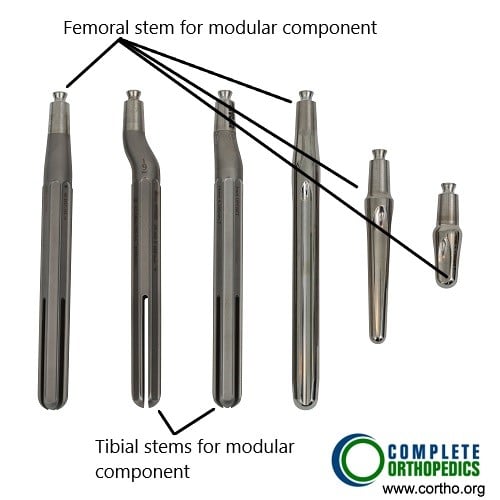
Tibial and femoral stems for modular knee components
A bone graft may be taken from the patient from a different location or may be taken from a bone bank. Metallic cones and metaphyseal sleeves may be used to compensate for bone loss. Specialized implants with a long stem or constrained tibial implants may be used to reduce instability and provide better fixation.
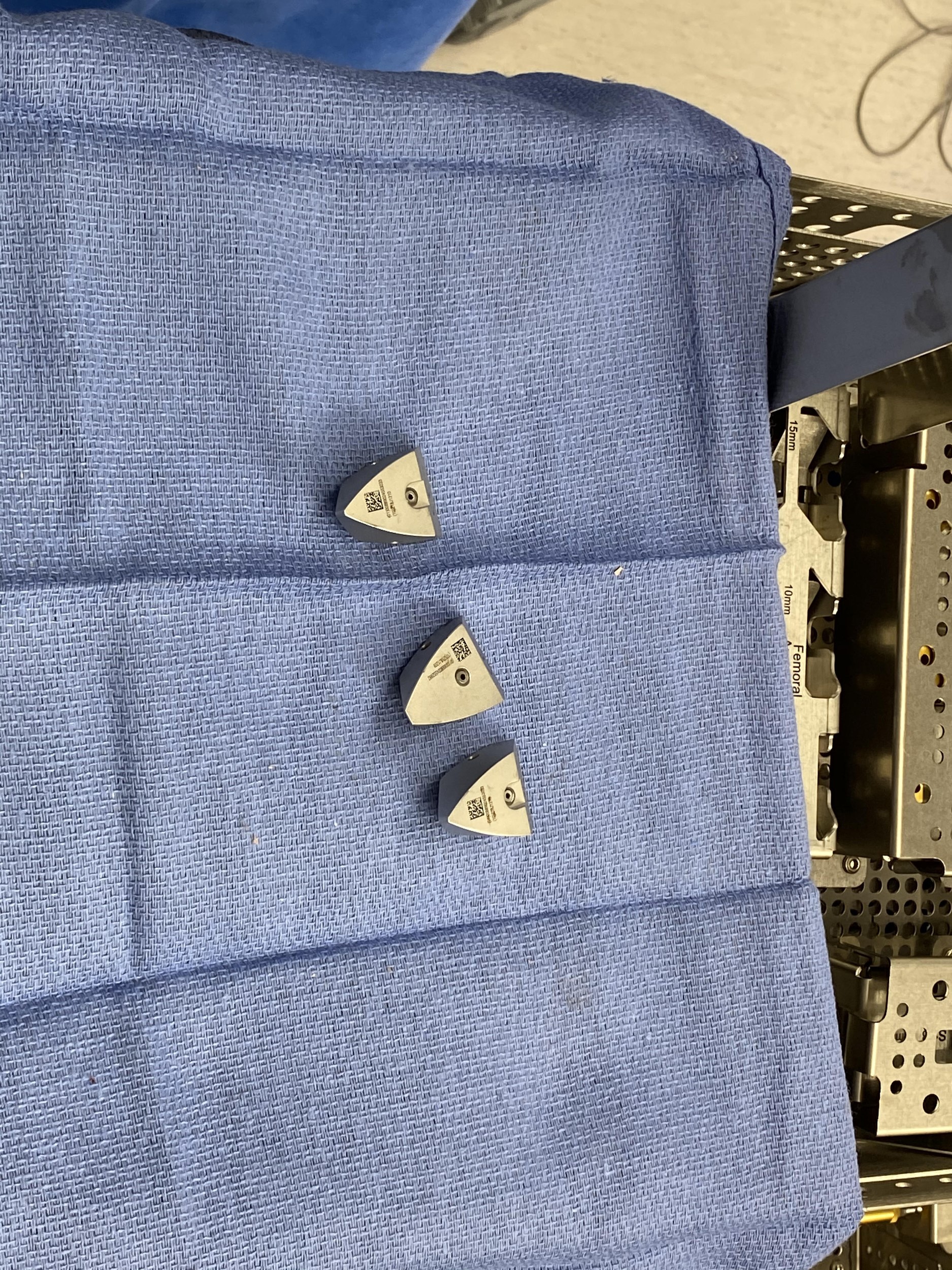
Metallic cones.

Metaphyseal sleeves.
Complications
The risk of complications is slightly more in knee revision surgery than the primary procedure. They may be potential complications such as heart attack, stroke, or pneumonia. There may be intraoperative complications such as fractures, shortening, instability, nerve, or blood vessel damage.
During the few weeks after the surgery, there is an increased risk of blood clots in the leg, infection, or dislocation.
Advances in Revision Knee Surgery
Recent advancements have improved the outcomes of revision knee surgery:
Better Implants: Newer implants are designed to be more durable and to fit better, which can improve function and longevity.
Enhanced Techniques: Advances in surgical techniques have made the procedure more precise, reducing complications and improving recovery times.
Infection Control: Improved methods for preventing and treating infections have led to better outcomes.
Customized Implants: Some patients may benefit from customized implants designed specifically for their anatomy, which can improve the fit and function of the knee replacement.
Success
The vast majority of the revision knee replacements are done without any complications. A few may complain of residual knee pain, which can be managed with medications and physical therapy. With the increasing effectiveness of the implant materials and surgical techniques, revision surgeries are being done successfully.
Revision knee surgery can significantly improve the quality of life for many patients. However, the success rates vary based on several factors:
Patient Health: Overall health and comorbidities (other health conditions) can affect recovery and outcomes.
Reason for Revision: The underlying reason for the revision (e.g., infection, loosening) can influence the success rate.
Surgical Expertise: The experience and skill of the surgeon performing the revision are crucial for a successful outcome.
Recovery and Rehabilitation
Recovery from revision knee surgery can be extensive. Here’s what to expect:
Hospital Stay: Patients usually stay in the hospital for a few days after surgery. During this time, they receive pain management and start physical therapy.
Physical Therapy: Physical therapy begins almost immediately to help improve mobility and strengthen the muscles around the knee. This therapy can continue for several months.
Home Adjustments: Patients may need to make adjustments at home, such as installing handrails or using a walker, to help with mobility during recovery.
Follow-Up Visits: Regular follow-up visits with the surgeon are necessary to monitor the progress of healing and ensure that the new implant is functioning correctly.
Long-Term Recovery: Full recovery can take up to a year. Patients are encouraged to stay active and maintain a healthy weight to reduce stress on the new knee.
Do you have more questions?
How long does a revision knee surgery take?
The duration of revision knee surgery can vary, but it generally takes between 2 to 3 hours, depending on the complexity of the case and the extent of the damage or complications with the initial implant.
What are the signs that my knee replacement is failing?
Signs of a failing knee replacement include persistent pain, swelling, instability, decreased range of motion, and sometimes noticeable changes in the alignment of the leg.
Can revision knee surgery be done on an outpatient basis?
Revision knee surgery is generally more complex and is usually performed in a hospital setting with an expected stay of a few days, unlike some primary knee replacements that can sometimes be done on an outpatient basis.
What type of implants are used in revision knee surgery?
Revision knee surgery often uses more robust and specialized implants designed to address the specific issues of the failed primary implant, sometimes including stems and augments for additional stability.
Will I need physical therapy after revision knee surgery?
Yes, physical therapy is crucial for recovery after revision knee surgery. It helps to restore strength, flexibility, and function to the knee.
How painful is revision knee surgery compared to the initial knee replacement?
Pain levels can vary, but many patients report that the pain after revision surgery is similar to or slightly more than the initial knee replacement due to the complexity of the procedure.
What are the success rates for revision knee surgery?
Success rates for revision knee surgery can vary but are generally around 85% to 90%, depending on the reason for the revision and the patient’s overall health.
How long will the new implant last after revision surgery?
While there is no guarantee, a well-performed revision knee surgery with proper implants can last 10-20 years, similar to primary knee replacements.
What lifestyle changes should I make after revision knee surgery?
Post-surgery, it’s important to maintain a healthy weight, stay active with low-impact exercises, and avoid activities that put excessive stress on the knee.
What should I do if I experience complications after revision knee surgery?
Contact your surgeon immediately if you experience signs of infection (fever, redness, or drainage), severe pain, or if you have difficulty moving the knee.
: How can I prepare my home for recovery after revision knee surgery?
Preparing your home for recovery includes installing handrails, keeping essential items within reach, and possibly arranging for a raised toilet seat or shower chair.
Will I need help at home after revision knee surgery?
Yes, it’s advisable to have someone assist you at home during the initial recovery period to help with daily activities and transportation to follow-up appointments.
How often will I need to see my surgeon after revision knee surgery?
Follow-up visits typically occur at two weeks, six weeks, three months, six months, and then annually to monitor the implant and overall recovery.
Can revision knee surgery address alignment issues from my first knee replacement?
Yes, one of the goals of revision surgery is to correct any alignment issues that may have occurred with the initial knee replacement.
What dietary changes should I make to aid my recovery after revision knee surgery?
A balanced diet rich in protein, vitamins, and minerals can help in healing. Staying hydrated and possibly taking supplements as recommended by your doctor can also aid recovery.
What are the long-term outcomes of revision knee surgery?
Long-term outcomes are generally positive, with most patients experiencing significant pain relief and improved function, though the recovery process can be longer and more challenging than the initial surgery.
Is it normal to feel numbness around the incision site after revision knee surgery?
Yes, some numbness around the incision site is normal due to nerve disruption during surgery, and it may persist for several months.
Are there any special exercises I should do before revision knee surgery?
Preoperative exercises focusing on strengthening the quadriceps, hamstrings, and maintaining range of motion can help improve postoperative recovery.
How can I prevent infections after revision knee surgery?
Preventing infections includes proper wound care, following your surgeon’s instructions for hygiene, and possibly taking antibiotics as prescribed.
What type of support will I need for mobility after revision knee surgery?
Initially, you will likely need crutches or a walker. As you progress in your recovery, you may transition to a cane before becoming fully independent.
How does bone quality affect the success of revision knee surgery?
Good bone quality is crucial for the success of the surgery as it affects the stability and longevity of the new implant. Bone grafts may be used if there is significant bone loss.
Can I drive after revision knee surgery?
You can usually start driving again once you have regained sufficient strength and mobility in your knee and are no longer taking narcotic pain medications, typically 4-6 weeks post-surgery. Always get your surgeon’s approval before resuming driving.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
