Knee Arthroplasty Implants
If knee pain worsens, disrupts daily activities, or comes with swelling and redness, it is essential to see a healthcare professional. At Complete Orthopedics, our skilled team specializes in treating posterior cruciate ligament injuries with tailored methods and surgical options. We prioritize understanding your symptoms, identifying the root causes, and recommending appropriate treatments or surgeries.
Our locations are spread throughout New York City and Long Island, with affiliations to six major hospitals, ensuring access to high-quality knee care. Make an appointment with one of our orthopedic surgeons either online or by phone. Discover the causes and treatments for knee pain and learn when surgery may be the best option.
Overview
Knee replacement surgery is one of the most commonly performed surgery by orthopedic surgeons. The surgery offers relief from knee pain and increases mobility. Common causes for knee pain include arthritis caused by primary osteoarthritis, rheumatoid arthritis, psoriatic arthritis, and secondary arthritis. The surgery is performed when all conservative forms of management are exhausted.
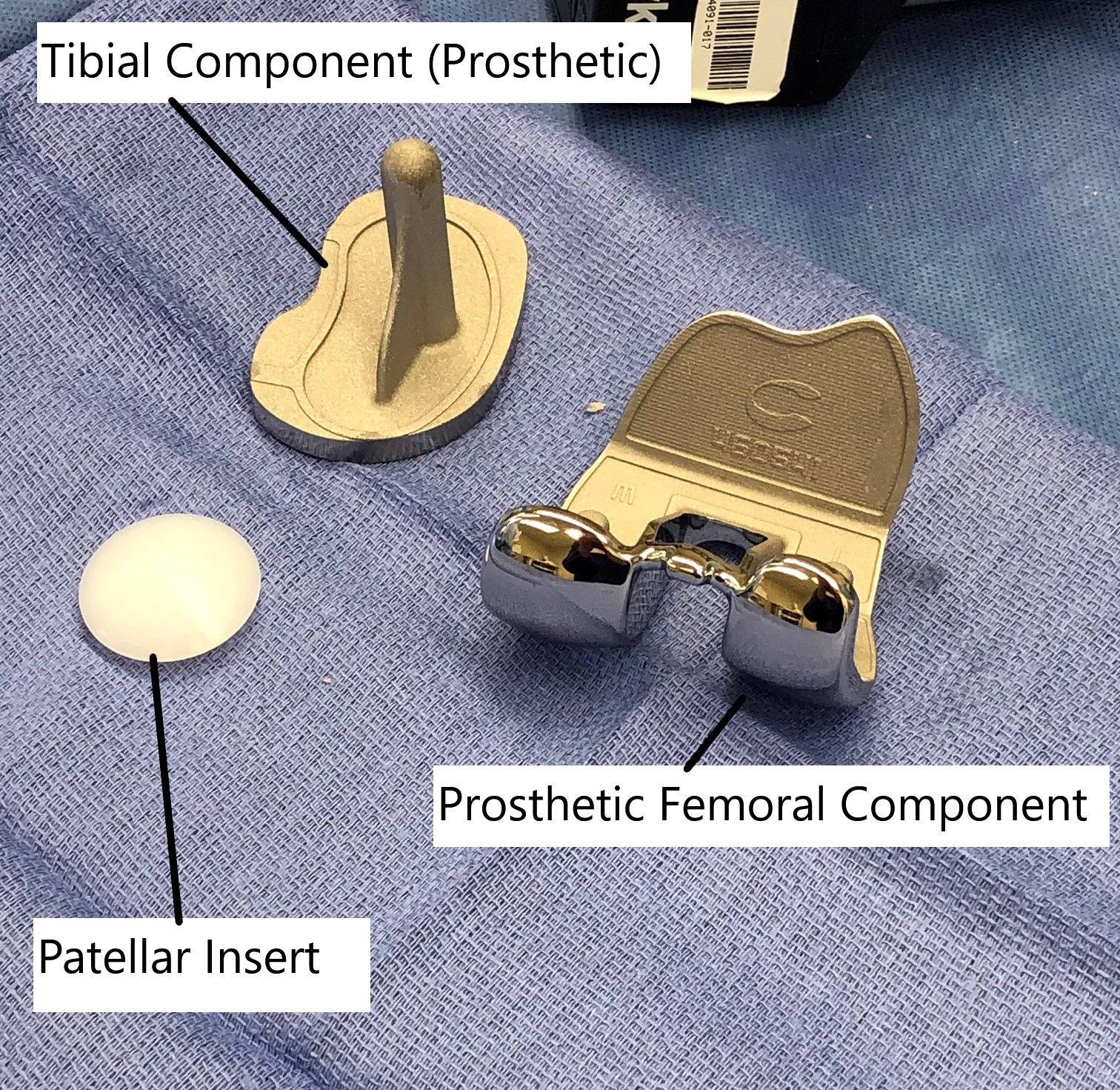
Knee arthroplasty implants.
A total knee replacement involves the replacement of the ends of the bones forming the knee joint with artificial parts. The prosthetic parts are made of metal and plastic components. The type of implants used in the surgery depends upon the anatomy of the patient, patient’s medical conditions, age, physical activity, and surgeon’s expertise.
Procedure
During the surgery, the joint is opened from the front and the damaged bone along with cartilage is removed. Bone cuts are made with specially designed jigs to prepare the joint surface. Both the anterior and posterior cruciate ligaments are usually sacrificed in posterior stabilized implants. The medial and lateral collateral ligaments are retained and surgically released to balance the alignment.
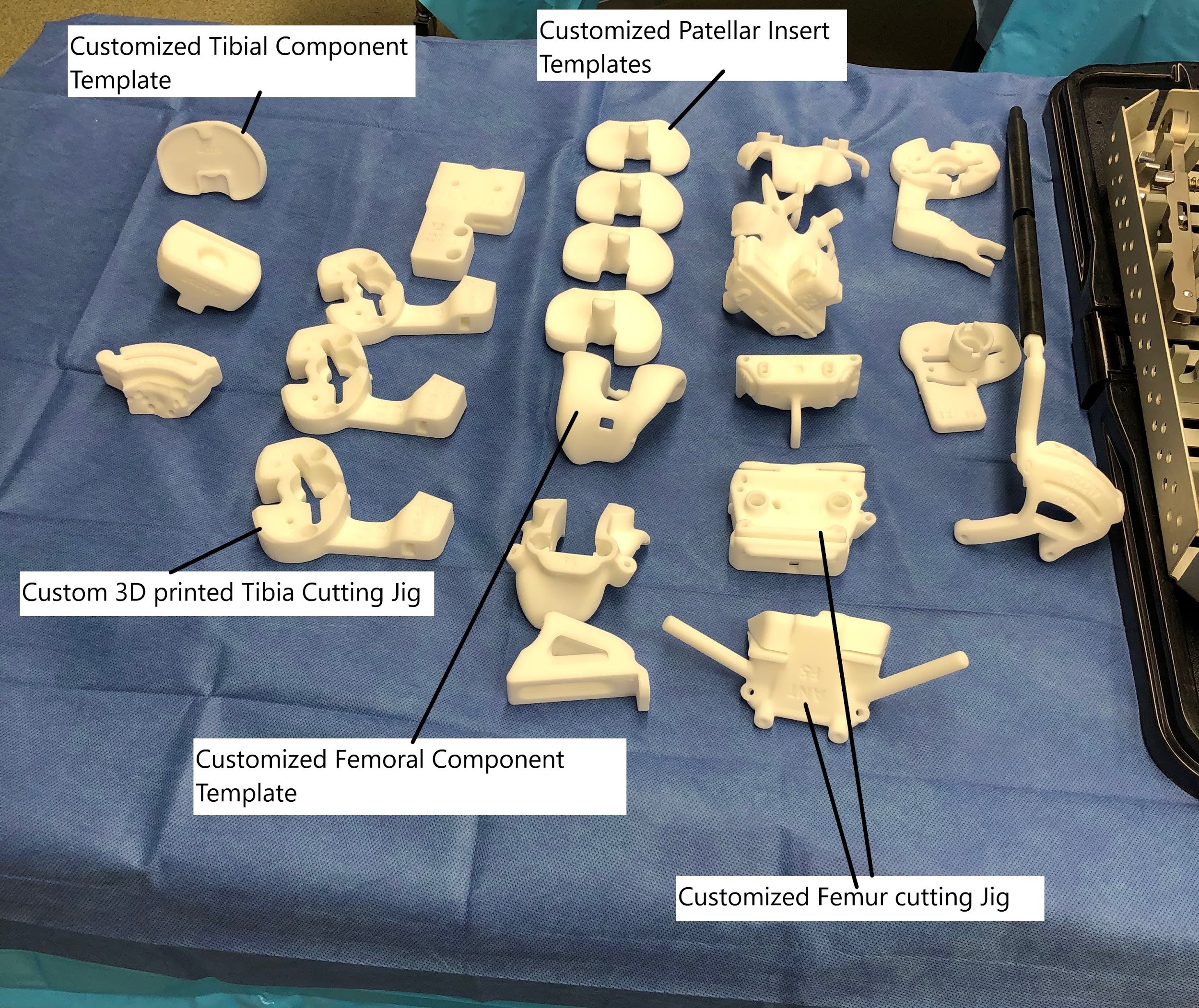
Customized 3D printed instruments and templates for assisting knee arthroplasty.
The metal parts are then introduced and are glued with acrylic bone cement. A special high-grade plastic (Polyethylene) is inserted between the metal parts acting as a stabilizer and cushion. The metal parts are made of a cobalt-chromium alloy and are designed to allow smooth gliding. The undersurface of the patella is resurfaced and a special plastic is cemented to the undersurface.
The joint is thoroughly irrigated, cleaned, and closed. Intraoperative medications may be injected to reduce post-op pain. The patient is shifted to the recovery room where their vitals are closely monitored.
Ideal Implants
The biomechanics of the knee joint are complicated rather than simply bending and straightening. Movements such as rollback and gliding occur in a natural knee to provide stability.
Ideally, any prosthetic implant replacing the knee joint should have an anatomic femoral and tibial surface. The implant should be able to reduplicate the function of menisci and cruciate ligaments. The implant should be able to maintain contact throughout the normal range of motion. The implant should be stable through 110 degrees of flexion and full extension.
There are 3 compartments in the knee joint, the inner and the outer compartment and the patellar compartment. All three are usually replaced in a total knee replacement. However, some patients with limited arthritis may benefit from a unicompartmental or bicompartmental arthroplasty. The implant designs are made for the compartment there are to replace.
Constrained and Non-constrained Implants
The constraint is the ability of the implant to provide stability in the front-back and sideways. The ligaments, bone anatomy, and various soft tissues provide stability to the knee during motion. In advanced arthritis, there may be loss of the stabilizing structures causing instability. The constraints implants are used in severely unstable knees.
The most commonly used implants are non-constrained, posterior-stabilized (PS), and cruciate-retaining (CR).
Posterior cruciate ligament retaining (CR) implants utilize the native PCL to provide stability in flexion and extension. The native PCL also allows for some femoral rollback, but because the ACL (anterior cruciate ligament) is sacrificed, the rollback is not anatomical.
The CR implant is used mainly in knees with minimal arthritis and soft tissue laxity. The implants require a functioning posterior cruciate ligament.
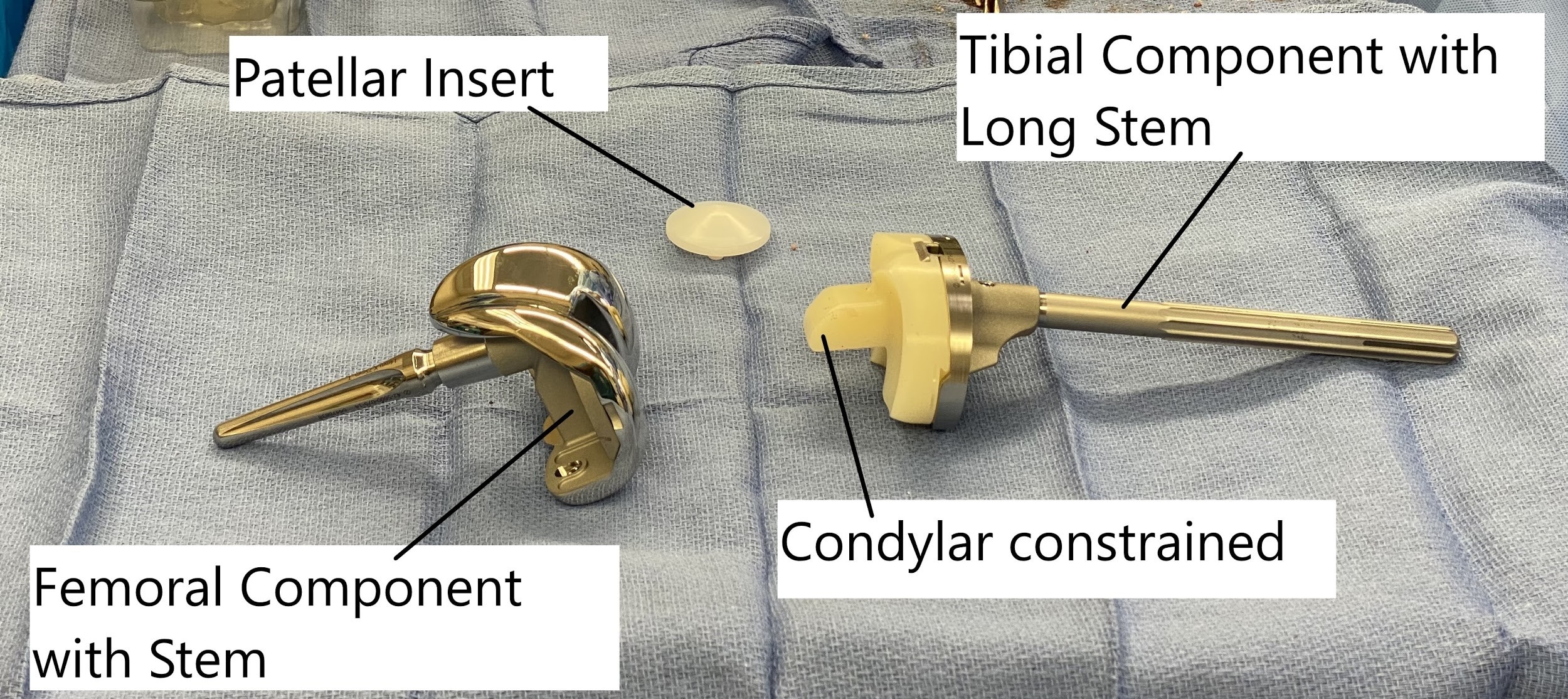
Revision knee replacement implants (Condylar constrained)
The posterior cruciate substituting (PS) also known as posterior stabilized implants are more commonly used than CR. The implant design includes a special post on the polyethylene insert and a cam mechanism on the femoral component. The cam-post mechanism prevents the thigh bone from dislocating forward when straightening the knee.
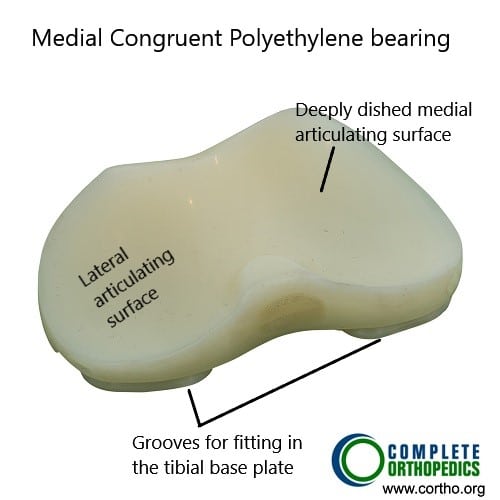
Medial congruent polyethylene
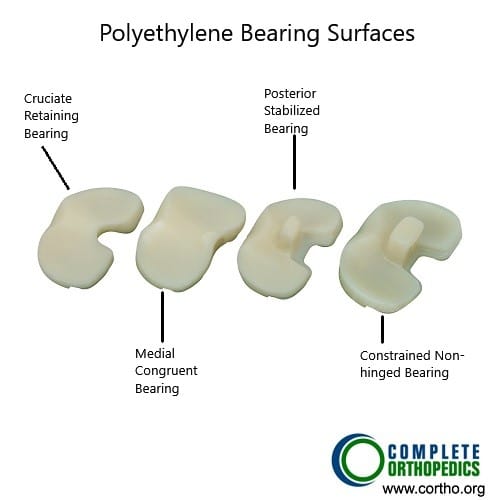
Different types of Polyethylene
The above images show different types of polyethylene inserts. The cruciate retaining and medial congruent polyethylene inserts lack a tibial post as the native posterior cruciate ligament is intact. The posterior stabilized and constrained polyethylene inserts have a tibial post for providing femoral rollback. The constrained insert has a tall and wide tibial post which provides small amount of side to side and rotational stability.
The cam-post mechanism also allows femoral rollback that helps in bending the knee without impingement. The cam-post mechanism, however, does not provide any sideways stability and requires the integrity of the stabilizing soft tissues.
In patients with a sideways instability, implant designs are modified to include a larger central post. The wider post substitutes for the medial collateral ligament (MCL) and the lateral collateral ligament (LCL). These are known as constrained non-hinged designs. The implant design however requires more resection of the femoral bone.
Constrained hinged are implant designs that involve the femoral component connected with a bar to a rotating platform of the tibia. These are used in cases of severe knee instability on all the sides of the knee.
A mobile-bearing polyethylene design includes a mobile bearing that is not attached to the tibial component. The mobile polyethylene can rotate freely on the tibial component. It may reduce the wear and tear of the polyethylene by increasing the surface area of contact. However, there may be a greater risk of dislocation of the mobile bearing implant designs.
The implants used in the knee replacement may be fixed to the bone with bone cement or maybe press-fit to the bone. The implants utilizing uncemented fixation have a special porous surface to allow bone ingrowth on the implant. Hybrid fixation involves an uncemented femoral component with a cemented tibial component. The patellar component is usually cemented due to high cases of failure with uncemented patellar fixation.
Successful knee replacement surgeries last on an average of 15 – 20 years or more. But like all mechanical machines, knee replacement implants may fail after many years. They may also fail due to other causes such as infections, misplacement, or trauma.
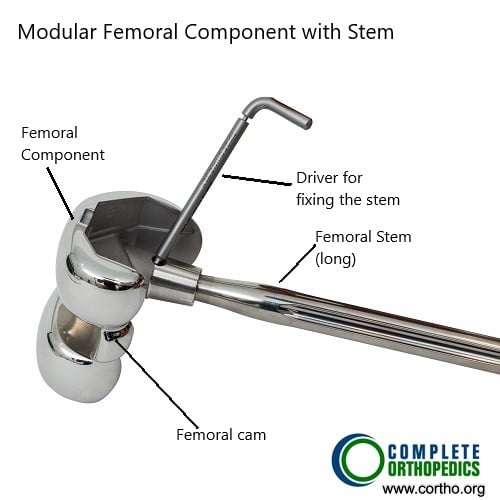
Modular femoral component with stem

Modular tibial component with stem
Modular implant designs are used in revision surgeries. The revision surgeries require the extraction of the old implants and implantation of the newer implants. The revision surgeries require implants with a longer stem to fit in the femur and tibia. The longer stem allows for greater stability and fixation of the implant.

Modular tibial component with metaphyseal cone
The modular implants may also allow attachments for metal parts known as augments to substitute for bone loss during extraction. The revision designs also typically have a wider cam post mechanism to allow for greater stability.
Components of Knee Arthroplasty Implants:
Knee arthroplasty implants consist of several components, including the femoral component, tibial component, and patellar component (in TKR). These components are made from various materials, such as metal alloys, ceramics, and polymers, each offering unique benefits in terms of durability, wear resistance, and biocompatibility.
Materials Used in Knee Arthroplasty Implants
Metal Alloys: Commonly used metals include cobalt-chromium and titanium alloys. These materials provide excellent strength and durability, ensuring the longevity of the implant.
Ceramics: Ceramic components are known for their smooth surface finish and wear resistance. They reduce friction within the joint, leading to improved longevity and reduced wear of the implant.
Polymers: High-density polyethylene is often used in knee arthroplasty implants due to its low friction properties and ability to mimic the natural cartilage of the knee joint.
Functionality of Knee Arthroplasty Implants
Knee arthroplasty implants aim to replicate the function of the natural knee joint, allowing for smooth movement and weight-bearing activities. The design of the implants, including their shape, size, and materials, is carefully engineered to promote stability, flexibility, and durability.
Benefits of Knee Arthroplasty Implants:
Pain Relief: Knee arthroplasty implants effectively alleviate chronic knee pain, allowing patients to engage in daily activities without discomfort.
Improved Mobility: By restoring joint function, knee arthroplasty implants enhance mobility and range of motion, enabling patients to perform tasks that were previously challenging.
Enhanced Quality of Life: With reduced pain and improved function, patients experience a significant improvement in their overall quality of life, enjoying greater independence and participation in social and recreational activities.
Risks and Complications
While knee arthroplasty surgery is generally safe and effective, there are risks associated with any surgical procedure. These may include infection, blood clots, implant failure, and stiffness of the joint. However, with proper preoperative evaluation, surgical technique, and postoperative care, the risk of complications can be minimized.
Recovery and Rehabilitation
Following knee arthroplasty surgery, patients undergo a comprehensive rehabilitation program to regain strength, flexibility, and mobility. Physical therapy exercises, along with pain management techniques, are essential for a successful recovery and long-term outcomes
Read more about Total Knee Replacement here.
Do you have more questions?
What are the primary materials used in knee implants?
The primary materials used in knee implants are metal alloys (such as cobalt-chromium and titanium), ceramics, and high-density polyethylene. These materials are chosen for their durability, wear resistance, and biocompatibility.
How do I know which type of knee implant is best for me?
The best type of knee implant for you depends on various factors such as your age, weight, activity level, bone quality, and specific knee anatomy. Your orthopedic surgeon will evaluate these factors and recommend the most suitable implant.
What is the difference between a fixed-bearing and a mobile-bearing knee implant?
A fixed-bearing knee implant has a stationary polyethylene insert between the metal components, while a mobile-bearing implant allows the polyethylene insert to move slightly. Mobile-bearing implants may offer more natural movement but require more precise surgical technique.
Can knee implants be customized for each patient?
Yes, knee implants can be customized to match the patient’s anatomy. Custom implants are designed using advanced imaging techniques to create a precise fit, which can improve outcomes and reduce recovery time.
What are the benefits of using ceramic components in knee implants?
Ceramic components are known for their smooth surface finish and high wear resistance. They reduce friction within the joint, which can enhance the longevity of the implant and provide smoother movement.
Are there any risks associated with the materials used in knee implants?
While the materials used in knee implants are generally safe and biocompatible, there is a small risk of allergic reactions or metal sensitivity. Patients with known allergies should discuss alternative materials with their surgeon.
How are knee implants attached to the bone?
Knee implants can be attached to the bone using bone cement (cemented implants) or by allowing bone to grow into a porous surface on the implant (uncemented or press-fit implants). The choice depends on factors like bone quality and surgeon preference.
What is the expected lifespan of a knee implant?
The expected lifespan of a knee implant is typically 15 to 20 years. However, factors such as activity level, weight, and overall health can influence the longevity of the implant.
Can knee implants wear out over time?
Yes, knee implants can wear out over time due to friction and stress from regular use. Advances in materials and design have improved their durability, but high-impact activities can accelerate wear.
What happens if my knee implant wears out or fails?
If a knee implant wears out or fails, a revision surgery may be necessary to replace the worn or damaged components. Revision surgery is more complex and involves removing the old implant and placing a new one.
Are there different sizes of knee implants?
Yes, knee implants come in various sizes to accommodate different patient anatomies. Surgeons select the appropriate size during surgery to ensure a proper fit and alignment.
How do knee implants mimic natural knee movement?
Knee implants are designed to replicate the natural anatomy and movement of the knee joint. They include components that allow for flexion, extension, and rotation, providing stability and smooth motion.
What is the role of polyethylene in knee implants?
Polyethylene is used in the tibial component of knee implants due to its low friction and wear properties. It acts as a cushion between the metal components, allowing for smooth joint movement.
Are there gender-specific knee implants?
Yes, some manufacturers offer gender-specific knee implants that are designed to better match the anatomical differences between male and female knees, potentially improving fit and function.
What advancements have been made in knee implant technology?
Advancements in knee implant technology include improved materials, custom-fit implants, minimally invasive surgical techniques, and enhanced implant designs that more closely mimic natural knee movement.
Can knee implants be used in patients with osteoporosis?
Yes, knee implants can be used in patients with osteoporosis, but the surgeon may choose specific implant types and fixation methods to ensure stability and reduce the risk of complications.
How do surgeons ensure the correct alignment of knee implants?
Surgeons use various techniques, including preoperative planning, intraoperative navigation systems, and alignment guides, to ensure correct placement and alignment of knee implants, which is crucial for optimal function and longevity.
What is the role of the patellar component in knee implants?
The patellar component replaces the undersurface of the kneecap (patella) and provides a smooth surface for articulation with the femoral component, reducing pain and improving knee function.
Can knee implants be affected by infection?
Yes, like any surgical implant, knee implants can be affected by infection. Preventive measures, such as antibiotics and sterile surgical techniques, are used to minimize the risk. In rare cases, an infected implant may need to be removed and replaced.
Are there different designs for the femoral component of knee implants?
Yes, there are various designs for the femoral component, including posterior-stabilized, cruciate-retaining, and bicruciate-retaining designs. Each design offers different benefits based on the patient’s specific needs and the condition of their knee ligaments.
How do knee implants accommodate different levels of activity?
Knee implants are designed to accommodate a range of activity levels. High-performance implants with advanced materials and designs are available for active patients, while standard implants are suitable for less active individuals.
Can knee implants be used in cases of severe deformity?
Yes, knee implants can be used in cases of severe deformity. Surgeons may use specialized implants and surgical techniques to correct alignment and restore function in complex cases.
What is the role of computer-assisted surgery in knee implant placement?
Computer-assisted surgery provides real-time data and precise guidance during knee implant placement, improving accuracy and alignment, which can enhance the function and longevity of the implant.
Can knee implants be made from alternative materials for patients with metal allergies?
Yes, for patients with metal allergies, alternative materials such as ceramic and special polymer-based implants can be used. Discuss your allergies with your surgeon to determine the best material for your implant
How do I care for my knee implant after surgery to ensure its longevity?
To care for your knee implant, maintain a healthy weight, stay active with low-impact exercises, avoid high-impact activities, follow your surgeon’s postoperative instructions, and attend regular follow-up appointments to monitor the condition of the implant.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
