Case study: Left Customized Knee Replacement
in an 80-year-old male
An 80-year-old male presented to our office with complaints of worsening left knee pain. He had the pain for the past many years and is unable to recall any specific time of onset. The patient previously had a right total knee replacement 4 years ago.
He was a retired driving instructor and was living with his son. He was fond of driving and going places, but the worsening pain in the left knee had severely affected his mobility. He was unable to climb stairs to go to the second floor. Walking from the house to the local deli was described as a great ordeal.
He stated he had an extremely good recovery and results from his previous replacement surgery. He had tried physical therapy, cortisone injections and home exercise program with minimal relief. The pain was associated with stiffness and crackling sound from the joint.
The pain was described as a dull ache to sharp located diffusely in the left knee. The intensity varied from mild at rest to severe with activity. The pain was especially worse on walking, bending, twisting, turning and going up and down the stairs. There was no radiation of the pain. The patient felt the pain flares up with changes in the weather.
He was a former smoker having quit 20 years ago (36 pack-years). He was well-nourished and had a past medical history of hypertension, benign prostate hypertrophy, coronary artery disease, and gastroesophageal reflux disease. All his medical conditions were well controlled and stable with medications.
He was mobile with the support of a cane. The gait of the patient was steady and antalgic. Genu varus deformity was present on the left knee. There were no scar, sinus or discharge from the skin overlying left knee. There was mild swelling with a positive patellar tap.
The range of motion was moderately restricted with painful terminal movements. Tests for coronal, sagittal, and axial plane instability were negative. There was tenderness in the medial joint line and medial patellar facet. The examination of the contralateral knee demonstrated a full range of motion and no swelling. There was a linear scar present anteriorly from the past surgical incision.
The examination of bilateral hips was unremarkable except for bilateral trochanteric tenderness suggesting bursitis. There was no broadening or thickening of the trochanters. There was no distal neurological deficit. The bilateral distal pulses were palpable and good volume.
Imaging revealed severe osteoarthritis of all three compartments of the left knee. After considering his comorbidities, he was advised to undergo left custom total knee replacement. Risks, benefits, and alternatives were discussed with him at length. He agreed to go ahead with custom left total knee arthroplasty.
A few weeks prior, CT of the patient was obtained to accurately determine the knee anatomy. The correct bone cuts needed to have a physiological alignment were also determined. The information was outlined in a preoperative surgical plan. Disposable bone jigs were constructed. Patient-Specific implants were made to fit uniquely into the patient’s knee.

Topogram image of the patients lower extremities, suggesting severe tricompartmental osteoarthritis of the left knee.
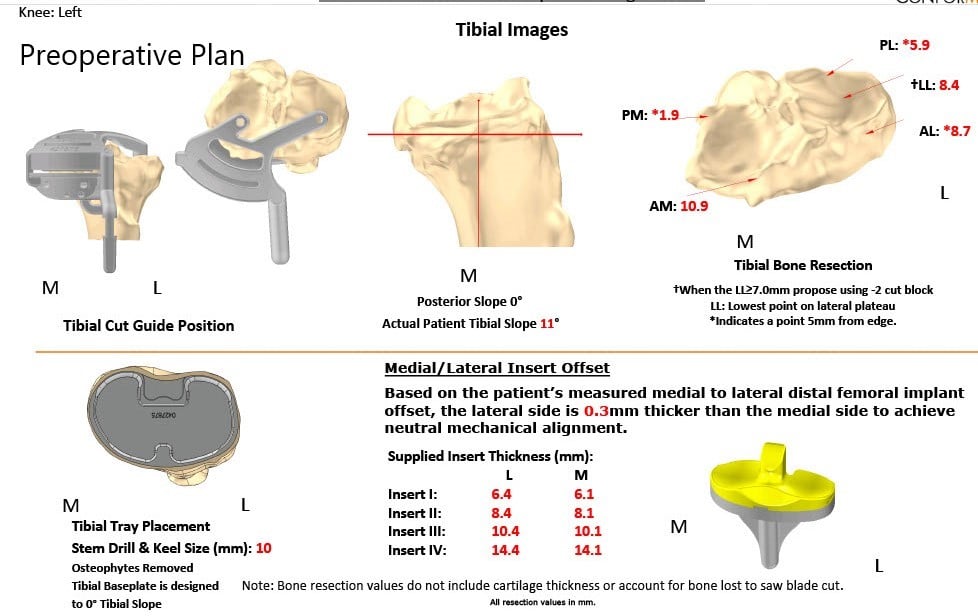
Complete Orthopedics patient-specific surgical plan for a left customized knee replacement in an 80-year-old male.
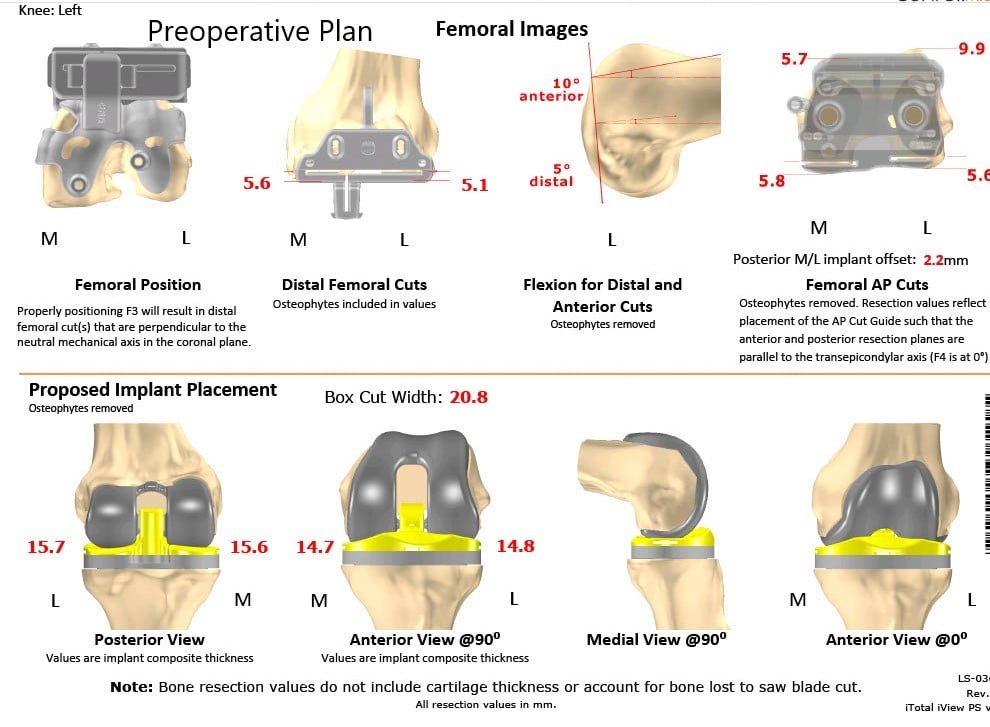
Complete Orthopedics patient-specific surgical plan for a left customized knee replacement in an 80-year-old male (scan 2)
OPERATION: Left custom total knee replacement.
IMPLANTS USED: Custom femur and Custom tibia with a 29 mm patella with PS poly.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining informed consent, signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient as well as with the daughter at length. The patient was then brought to the operating room.
Anesthesia was obtained by the anesthesiologist. The patient was then definitively positioned. The left knee was then draped and prepped in the usual sterile manner with a tourniquet cuff over the left thigh. Antibiotics were given. A timeout was performed. Tourniquet was exsanguinated and the cuff was elevated.
Skin and subcutaneous tissues were incised. Medial parapatellar fasciotomy was performed and the tibia was exposed. The tibial preparation was performed using the customized jigs. The tibial cut was made. The cut was checked. Attention was then turned towards the femur. The femoral cuts were made and the gap balancing was performed using medial and lateral eminence whereas the remainder of the meniscus and cruciate were then divided.
The notch cut was then performed. The patellar cut was then performed and the holes made in the patella. T rial patella was placed into position followed by the trial femur, trial tibia, and the poly was then placed into position. The knee was then trialed through full of a range of motion and the knee was stable. The patellar tracking was excellent.
Trial components were then removed. Cement was mixed. A thorough lavage was performed. The injection was given The femur was cemented into position. Excess cement was removed. The tibia was cemented into position. Excess cement was removed. Poly was cemented into position and excess cement around all components was then removed. 
The knee was then held in full extension with a bump under the ankle. Patellar cementation was performed. An extra bag of cement was opened for the cementation of the patella. Excess cement was removed and the patella was held in position with the patellar clamp.
After the cement hardened, a thorough lavage was performed. Medial parapatellar arthrotomy was closed with Vicryl and Quill. Cutaneous tissue was closed with 0 Vicryl, subcuticular tissue was closed with 2-0 Vicryl.
The skin was closed using staples. Sterile dressing was then applied. The patient was transferred to the postoperative care unit in stable condition.


Postoperative X-ray showing AP and lateral images of the left knee.
He had an excellent recovery and was able to walk with the help of a walker the same day. Prophylactic aspirin was started for deep vein thrombosis. The pain was well controlled with medications. The patient’s wound was found to be clean, dry and intact. Sutures were removed uneventfully. Physical therapy and gait training were started.
On subsequent follow-up visits, he was able to walk without support. The range of motion was complete without any pain. The patient was back to driving his car and playing with his grandkids. He follows up as needed.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
