Iliotibial Band Syndrome
Anyone can encounter discomfort in their knees occasionally. However, if the discomfort becomes intense, significantly affecting your daily activities, or if you notice swelling, sensitivity, or inflammation, it’s advisable to consult a medical professional.
At Complete Orthopedics, our specialized team of orthopedic knee specialists focuses on addressing knee discomfort through various treatments, including surgical interventions if necessary. We’re situated in New York City and Long Island, with surgical capabilities across six hospitals, ensuring access to cutting-edge knee surgery and orthopedic care. To schedule an appointment with one of our orthopedic surgeons, you can conveniently book online or reach out to us by phone.
Explore some common causes of knee discomfort and available treatment options, including when surgical intervention becomes the most viable solution.
Overview
Iliotibial band syndrome is a common condition causing pain on the outer side of the knee. The condition is quite common in people participating in sports and athletic activities that involve repetitive bending and extending the leg. The resulting overuse causes the tissues on the outer side of the knee to get inflamed.
The iliotibial band is a thick band of tissue running from the upper and outer part of the hip to the outer part of the upper shin bone. The tissue is formed from the structures connecting the tensor fascia lata muscle and the gluteus maximus muscle.
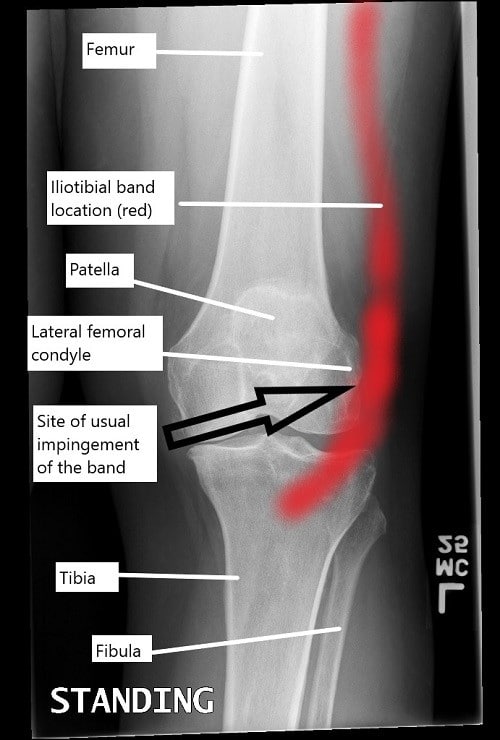
A knee x-ray illustrating the location of iliotibial band and the usual site of impingement.
Causes
Several factors can contribute to the development of ITBS:
Overuse: Engaging in repetitive activities such as running or cycling without proper rest can strain the ITB, leading to irritation and inflammation.
Poor Biomechanics: Issues with foot alignment, hip stability, or muscle imbalances can place excessive stress on the ITB, increasing the risk of developing ITBS.
Training Errors: Sudden increases in training intensity or duration can overload the ITB and result in injury.
Improper Equipment: Wearing worn-out shoes or using equipment that doesn’t provide adequate support can exacerbate ITBS symptoms.
Symptoms
The primary symptom of ITBS is pain on the outside of the knee, which may worsen with activity, especially during movements that involve bending or straightening the knee. Other common symptoms include:
Swelling or tenderness on the outside of the knee.
Pain that worsens when going downhill or downstairs.
A popping or snapping sensation over the outside of the knee.
The symptoms of iliotibial band syndrome are especially worse on walking/running, especially when the heel strikes the ground. The pain is usually described as a sharp pain that may or may not radiate down the leg or up the thigh. Some patients may also report a snapping sensation of the knee while bending or straightening the knee.
There may be an associated swelling on the outer part of the knee. Occasionally there may be redness or warmth on the outer aspect of the knee. The symptoms may be worse on navigating the stairs.
Diagnosis
The diagnosis of iliotibial band syndrome by the physician involves a detailed history and thorough examination of the knee joint. The physician may perform certain physical tests to identify the tightness of the iliotibial band. The physician may also perform more physical tests including examination of the lower spine to rule out other causes of pain.
Physical examination may involve tests such as ober test and noble compression test. The Ober test involves the patients lying on the side of the normal knee.
The examiner physician bends the knee at 90 degrees and places the thigh in line with the body but lifts the thigh up sideways. The patient is then requested to try to move the thigh inward towards the ground. Inability to move the thigh past a level may indicate iliotibial tightness.
Another test known as noble compression test involves testing the patient while he/she lies with their back on the examining table. The physician bends their knee at 90 degrees and tries to straighten it while applying pressure over the outer side of the knee. A positive test involves pain at 30-40 degrees of knee flexion.
The examining physician may also request imaging studies such as an MRI or ultrasound to aid in the diagnosis and rule out other causes. Other causes of pain on the outer side of the knee may include degenerative joint disease, patellofemoral stress syndrome, damage to the structures forming the knee joint such as ligaments and meniscus.
Management
The treatment of iliotibial band syndrome is mostly nonsurgical. Activity modification is the first step of managing iliotibial band syndrome. The activity modification may involve complete cessation of the offending activity or modification in the form of decrease in intensity, frequent rest, changes to other forms of activity, etc.
Other conservative forms of treatment such as icing, heat therapy, physical therapy and ultrasound therapy etc may be used to decrease the pain and inflammation. Non-steroidal anti-inflammatory medications such as aleve and ibuprofen may be used to reduce pain.
Physical therapy is done to improve flexibility and strength of the muscles. The improvement of the strength of the hip abductor muscles is linked with improved stability of the hip that may lead to improved function of the iliotibial band.
In rare circumstances, surgical management may be required for the treatment of iliotibial band syndrome. The surgery may involve cutting a small part of the band near the knee to increase the length of the band. Speak with your orthopedic surgeon regarding the best management for your symptoms.
Recovery
Step 1:
Rest and Activity Modification: The first step in recovering from ITBS is giving your knee time to heal. This means avoiding activities that worsen your symptoms, such as running or cycling, and opting for low-impact exercises like swimming or yoga instead. Rest doesn’t mean complete inactivity; it’s about finding a balance that allows your body to recover while staying active in ways that don’t aggravate your knee.
Step 2:
Ice Therapy: Applying ice packs to the affected area can help reduce inflammation and alleviate pain. Ice therapy is most effective when applied for 15-20 minutes several times a day, especially after activities that may strain your knee.
Step 3:
Stretching and Strengthening Exercises: Physical therapy plays a crucial role in ITBS recovery, focusing on stretching and strengthening exercises to improve flexibility and stability around the knee. Simple stretches targeting the ITB and surrounding muscles, such as the hip flexors and quadriceps, can help alleviate tightness and reduce strain on the knee.
Step 4
Foam Rolling: Foam rolling is another effective way to massage the ITB and surrounding muscles, releasing tension and promoting blood flow to the affected area. Using a foam roller regularly can help prevent stiffness and improve mobility as you progress through your recovery.
Step 5:
Gradual Return to Activity: As your symptoms improve, gradually reintroduce activities that may have caused discomfort in the past. Start with shorter durations and lower intensities, gradually increasing as your knee tolerates. Listen to your body and avoid pushing through pain, as this can delay your recovery or lead to setbacks.
Preventing ITBS
While ITBS can be challenging to prevent entirely, there are several steps you can take to reduce your risk of developing this condition:
Gradually increase training intensity and duration to avoid overloading the ITB.
Incorporate cross-training activities to vary the types of stress placed on your muscles and joints.
Ensure proper footwear and equipment to provide adequate support and cushioning.
Incorporate regular stretching and strengthening exercises into your routine to improve flexibility and muscle balance.
Listen to your body and address any early signs of discomfort or pain to prevent worsening of symptoms.
Conclusion:
Iliotibial Band Syndrome (ITBS) is a common overuse injury that affects many individuals, particularly athletes and runners. Understanding the causes, symptoms, diagnosis, and treatment options for ITBS is essential for effectively managing this condition and preventing future injuries. By incorporating proper training techniques, biomechanical corrections, and self-care strategies, you can reduce your risk of developing ITBS and continue to enjoy your favorite activities pain-free. Remember to consult with a healthcare professional for personalized guidance and treatment recommendations tailored to your specific needs and circumstances.
Do you have more questions?
What are the long-term consequences of untreated ITBS?
Untreated ITBS can lead to chronic knee pain and instability, potentially interfering with daily activities and reducing quality of life. It may also increase the risk of developing other knee-related conditions, such as patellofemoral pain syndrome or osteoarthritis, in the long term.
Can ITBS affect other parts of the body besides the knee?
While ITBS primarily affects the knee, it can also cause compensatory changes in gait and posture, leading to secondary issues such as hip pain, lower back pain, or foot problems.
Is surgery ever necessary to treat ITBS?
In rare cases where conservative treatments fail to provide relief, surgical intervention may be considered. Procedures such as ITB release or bursectomy may be performed to alleviate persistent symptoms and restore function.
How soon can I return to physical activity after experiencing ITBS symptoms?
The timeline for returning to physical activity varies depending on the severity of symptoms and individual healing rates. It’s crucial to gradually reintroduce activities once symptoms have resolved and to listen to your body to avoid exacerbating the condition.
Are there any specific stretches or exercises I should avoid if I have ITBS?
While stretching and strengthening exercises are generally beneficial for managing ITBS, certain movements that place excessive stress on the ITB, such as deep lunges or leg presses with heavy weights, may exacerbate symptoms and should be approached with caution.
Can ITBS occur in both knees simultaneously?
Yes, ITBS can affect both knees simultaneously, especially in cases where underlying biomechanical issues or training errors are present bilaterally. Symmetrical symptoms in both knees may indicate a systemic problem that requires comprehensive evaluation and treatment.
Are there any dietary supplements or medications that can help alleviate ITBS symptoms?
While there is limited scientific evidence supporting the use of dietary supplements or medications specifically for ITBS, anti-inflammatory medications such as ibuprofen may help reduce pain and inflammation in the short term. However, it’s essential to consult with a healthcare professional before starting any new supplements or medications.
Can ITBS be prevented through specific warm-up routines?
While warming up before physical activity can help prepare the muscles and joints for exercise, there is limited evidence to suggest that specific warm-up routines can prevent ITBS outright. However, incorporating dynamic stretches and activation exercises targeting the hip and knee muscles may help reduce the risk of injury.
Is ITBS more common in a particular age group?
While ITBS can occur in individuals of all ages, it is more commonly seen in younger athletes, particularly those engaged in activities such as running, cycling, or sports that involve repetitive knee movement.
How can I differentiate between ITBS and other knee conditions with similar symptoms?
Diagnosing ITBS typically involves a thorough physical examination and may require imaging tests to rule out other potential causes of knee pain, such as patellofemoral pain syndrome, meniscal injury, or iliotibial band friction syndrome.
Can wearing a knee brace help alleviate ITBS symptoms?
While knee braces may provide temporary relief by stabilizing the knee joint and reducing strain on the ITB, they are not typically considered a long-term solution for managing ITBS. Physical therapy and biomechanical corrections are generally more effective in addressing the underlying causes of ITBS.
Are there any specific risk factors that increase the likelihood of developing ITBS?
Several factors, including training errors, biomechanical abnormalities, muscle imbalances, and improper footwear, can increase the risk of developing ITBS. Individuals with a history of previous knee injuries or those with excessive foot pronation may also be more predisposed to ITBS.
Can ITBS occur suddenly, or is it typically a gradual onset?
ITBS can occur both suddenly and gradually, depending on the underlying cause and individual factors. While sudden onset ITBS may be triggered by a specific incident or activity, gradual onset ITBS often develops over time due to repetitive stress or overuse.
Is it possible to completely recover from ITBS?
With appropriate treatment and rehabilitation, many individuals can fully recover from ITBS and return to their previous level of activity. However, it’s essential to address underlying biomechanical issues and adopt preventive measures to reduce the risk of recurrence.
Can wearing orthotic inserts in my shoes help prevent ITBS?
Orthotic inserts may help correct biomechanical abnormalities and provide additional support and cushioning, reducing the risk of ITBS in some individuals. However, they should be prescribed and fitted by a qualified healthcare professional based on individual needs and foot mechanics.
Are there any specific activities I should avoid if I have ITBS?
Activities that exacerbate ITBS symptoms, such as running downhill or on uneven surfaces, should be avoided until symptoms have resolved. It’s essential to listen to your body and modify activities accordingly to prevent further irritation of the ITB.
Can ITBS lead to permanent damage to the knee joint?
In severe or chronic cases, untreated ITBS may contribute to structural changes in the knee joint, such as cartilage degeneration or patellar malalignment, which could potentially lead to long-term complications if left unaddressed.
Is there a genetic predisposition to developing ITBS?
While genetic factors may play a role in predisposing individuals to certain biomechanical abnormalities or musculoskeletal conditions that contribute to ITBS, the condition is primarily attributed to external factors such as training errors and overuse.
Can ITBS be exacerbated by changes in weather or environmental conditions?
While there is limited scientific evidence linking changes in weather or environmental conditions directly to ITBS exacerbations, factors such as temperature extremes, humidity, or terrain may indirectly impact symptoms by affecting joint lubrication and muscle performance.
How long does it typically take to recover from ITBS with conservative treatments?
The recovery time for ITBS varies depending on the severity of symptoms, individual healing rates, and adherence to treatment recommendations. With conservative treatments such as rest, physical therapy, and activity modification, many individuals experience improvement within a few weeks to a few months.
Are there any specific strategies for managing ITBS during athletic competitions or events?
During athletic competitions or events, managing ITBS involves a combination of proper warm-up and cool-down routines, pacing strategies to avoid overexertion, and using supportive taping or bracing techniques to minimize stress on the ITB and knee joint.
Can ITBS recur even after successful treatment?
Yes, ITBS can recur, especially if underlying biomechanical issues or training errors are not addressed adequately. Implementing preventive measures such as cross-training, proper footwear, and ongoing maintenance exercises can help reduce the risk of recurrence.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
