Case Study: Right Knee Custom
Arthroplasty in an 83-year-old male
An 81-year-old male presented to our office with complaints of right knee pain. He stated the pain has a gradual insidious onset 6 years ago. He was diagnosed with Osteoarthritis and tried conservative management. He stated that the pain was largely under control but had recently flared up in the past year.
His previous treatment modalities included physical therapy and knee injections (cortisone and hyaluronic). He stated the relief from cortisone injections at first lasted for 4-6 weeks but his last injections lasted only a week.
The location of the pain was diffuse in the right knee and was moderate in intensity (6/10). The pain was especially worse on activities involving bending, kneeling, twisting or walking. He described discomfort and stiffness after sitting for a long time. He was unable to do his laundry or even walk to the nearby supermarket for groceries.
The patient worked previously at an art gallery and had a keen interest in sculpting wood. He expressed dissatisfaction with not being able to pursue his hobby and the inability to perform his daily activities. One of his friends recently underwent joint replacement surgery with excellent restless. Motivated by his successful outcome, he was interested to know if he was a candidate for knee replacement.
The patient was a nonsmoker, teetotaler with no known drug allergies. He was single living with his daughter who worked as a teacher. His medical history included dyslipidemia and hypertension, both well controlled with medications (hydrochlorothiazide 25mg and Lipitor 20mgz). He had a right shoulder arthroscopic surgery 4 years ago.
His physical examination revealed mild genu varus deformity. The gait was steady and coordinated. There was mild effusion in bilateral knees without any local rise of temperature or erythema. Medial and lateral joint line tenderness was positive on the right side.
The active range of motion was from 5 degrees of extension to 95 degrees of flexion. Passive flexion was possible until 110 degrees but it was painful. Stress tests for instability and laxity were negative. His examination of bilateral hip joint and ankle joint, and left knee was normal. There was no distal neurological deficit.
Imaging studies were obtained revealing tricompartmental osteoarthritis of the right knee with severe involvement of the medial compartment. Considering the patient’s condition and demands, he was deemed as a candidate for total knee replacement with custom implants. Other treatment options including nonsurgical methods were discussed in detail with him. He agreed for a custom right knee replacement.


Preoperative X-ray image of the right knee showing AP and lateral views
Further CT scan of the right knee was obtained prior to the surgery. The information was utilized to create a 3D model of the patient’s knee anatomy. Unique patient-specific implants were then constructed utilizing the information of anatomy and biomechanics. Custom disposable jigs and instruments were 3D printed to match patients’ natural anatomy of the knee. A customized preoperative plan was created for accurate bone cuts and biomechanics.
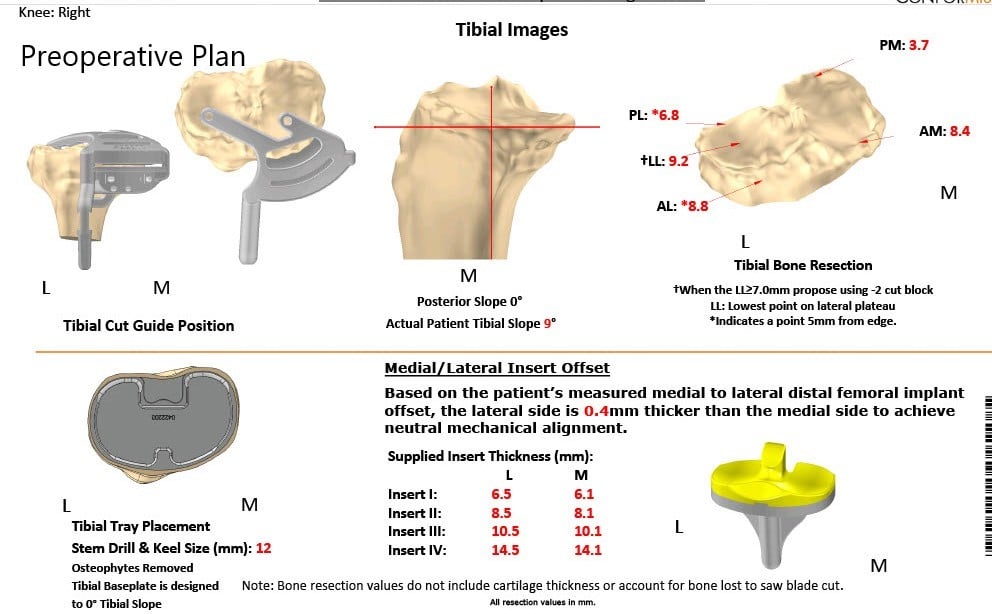
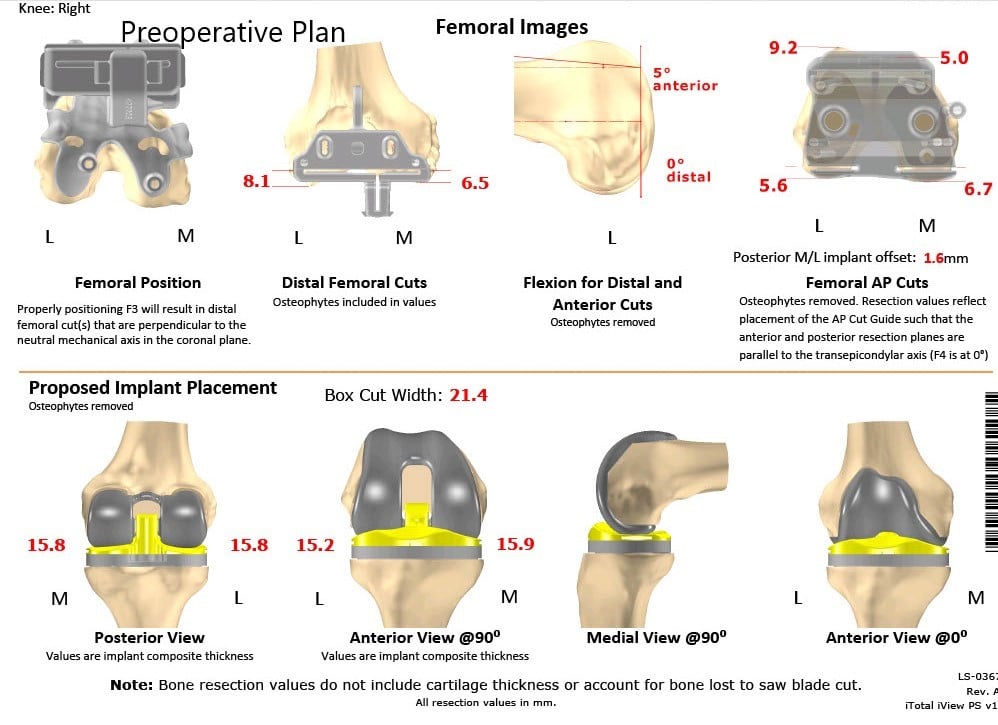
OPERATION: Right total knee arthroplasty using custom femoral component with a custom tibial tray with polyethylene 6 mm with patella 32 mm x 6mm.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining informed consent, signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure. The patient was brought to the operating room. Anesthesia was obtained by the anesthesiologist.
The patient was then definitively draped and prepped and the right knee was draped in the usual surgical fashion. A timeout was performed. The tourniquet was elevated after exsanguinating the limb. A straight incision was used for the arthrotomy. Skin and subcutaneous tissues were incised. Medial parapatellar arthrotomy was then performed.
The femur was exposed and the tibia was exposed. The tibial cutting guide was then placed into position and the tibial cut was performed. The alignment was checked. Attention was then turned towards the femur. The distal femur was then cut followed by the anterior and posterior Chamfer cuts as well as the anterior and the posterior cuts as well as the additional cut. The notch cut was then performed. Lamina spreaders were used medially and laterally and gap balancing was then performed.
Attention was then turned towards the tibia. The tibial preparation was then made. The trial tibia was then placed into position. The trial femur was then placed into position. The trial poly was then placed into position. The patella was then prepared. The holes were made in the patella and the trial patella was then placed into position.
Osteophytes on the medial side of the tibia were removed during the balancing process.
The knee was trialed through a full range of motion. The patella tracking was excellent. Full range of the knee was obtained intraoperatively. The trial components were then removed . The injection was given. Through lavage was given.
The femur was cemented into position. Excess cement was removed. The tibia was cemented into position, excess cement was removed. The poly was then placed into position. The knee was then reduced. Patella was cemented into position and excess cement was then removed. The knee was then held in full extension with a bump under the ankle. The patella clamp was removed after the cement hardened. Aricept was used for irrigation.
Medial parapatellar arthrotomy was closed with Vicryl and Stratafix. Cutaneous incisions were closed with O Vicryl, 2-0 Vicryl and the skin was closed using staples. Sterile dressing was then applied over the wound. The patient was then transferred to the postoperative care unit in stable condition.


Postoperative X-ray of the right knee showing AP and lateral views
The pain was well managed with Percocet and acetaminophen. He was started on aspirin 325mg for deep vein thrombosis (DVT) prophylaxis. He was walking the same day of the procedure with support. Further, he was advised physical therapy and continuous passive motion machine for some stiffness he complained after the procedure.
Staples were removed uneventful. On his 3 month post-surgery follow up, he was completely pain-free on the right knee. He was advised to discontinue aspirin. He was successfully able to return to his baseline daily activities. The patient was extremely happy with the outcome and follows as needed.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

