A 63-year-old female presented to our office with worsening left knee pain. She was working as a cook for a local diner. She recalls a motor vehicle accident with injuries to the left knee 20 years ago. She stated the left knee pain started insidiously two years after the initial trauma and was intermittent and mild in intensity. However, over the past year, the pain has been consistent in frequency.
She stated that the pain is located diffusely in the left knee, especially more on the inner side of the knee. The pain is worse with activities such as walking, bending, kneeling, twisting and turning. There is an associated stiffness in the knee when sitting for a long time.
The pain is moderate to severe in intensity (8/10) and dull aching to sharp in character. She denied any radiation, fever, swelling, multiple joint pain, instability or any abnormality of the bowel and bladder movement.
She was a former smoker and quit 5 years ago. Her medical history included hypertension and dyslipidemia, both well controlled with medications. Her current medications included aleve, lisinopril, and lovastatin. She previously had a left shoulder rotator cuff repair done 6 years ago.
The patient consulted an outside physician for her knee pain. She said she was diagnosed with Osteoarthritis and received multiple knee injections. According to the patient, the relief from injections was only moderate and didn’t last. She also tried other conservative treatment options such as physical therapy and home exercise program with minimal relief.
The patient was visibly disturbed by her knee pain. She had recently decreased her working hours and stayed home secondary to pain. Additionally, she was unable to perform daily activities such as doing laundry, groceries or walking her dog.
Her physical examination revealed mild swelling in the left knee. There was tenderness in the left medial joint line and medial patellar facet. The range of motion was not restricted but was painful at the terminal flexion. There was no sign of instability or laxity. Bilateral ankle and hip were normal in the examination. There was no distal neurological deficit.
Her X-ray of the left knee revealed tricompartmental osteoarthritis with medial joint space narrowing. Considering her lifestyle limiting arthritis of the left knee, she was advised to have custom left total knee arthroplasty. Risks, benefits, and alternatives were discussed with her in detail. She agreed to the plan.


Preoperative Scanogram images obtained from CT tomography
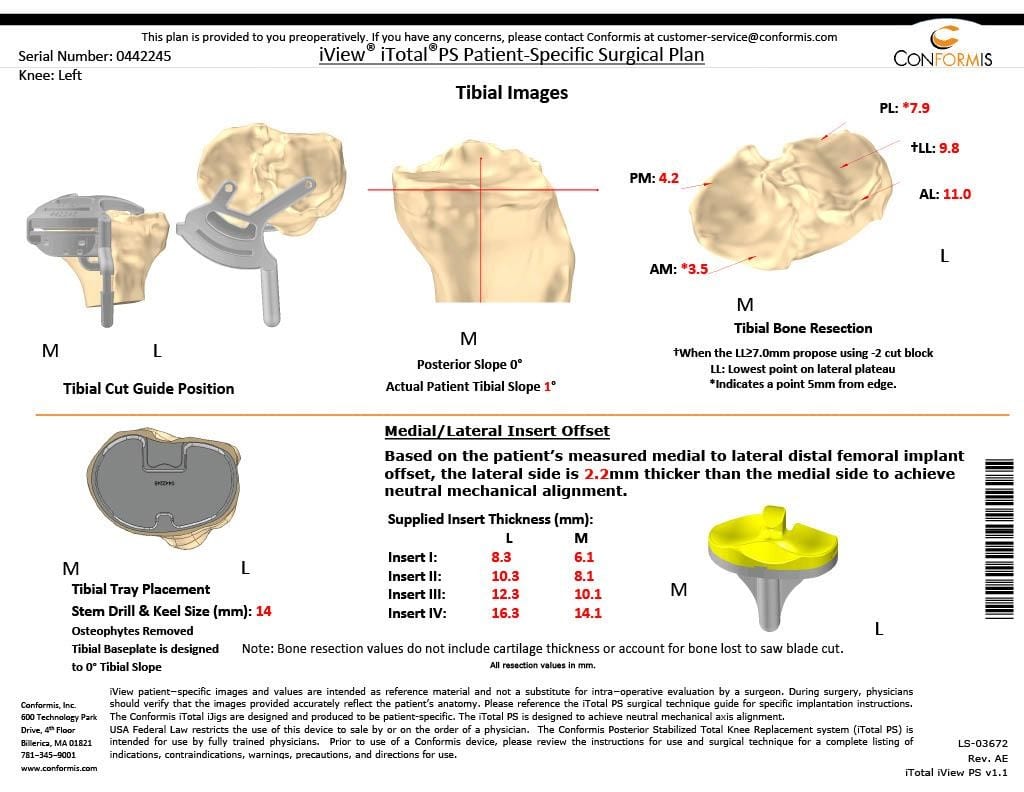
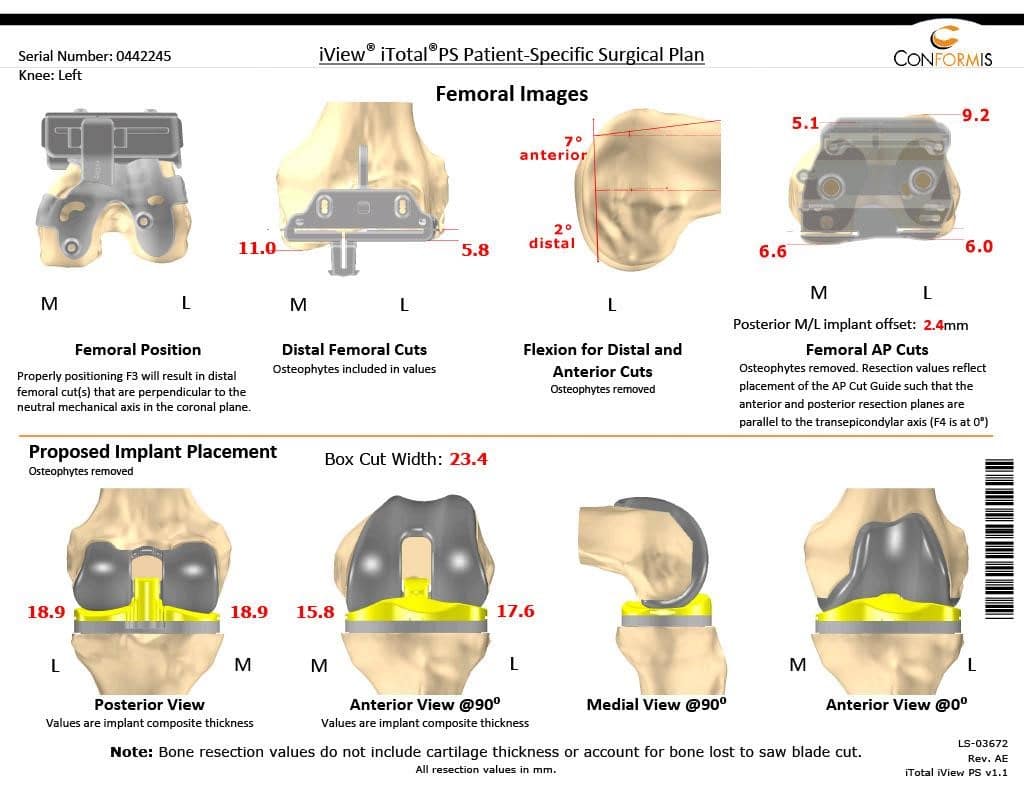
Patient detailed anatomy and biomechanics axis were obtained from a preoperative CT scan. The data obtained was used to construct custom implants. The custom implants were unique for the patient’s anatomy. Disposable 3D constructed jigs were made for accurate bone cuts. A preoperative plan was formed to aid the surgeon in the operation.
Operative notes
Implant used: Custom femoral implant with a custom tibial tray, with 8-mm polyethylene insert, with custom 32-mm x 6-m patellar implant.
Procedure: The patient was then definitively positioned and the left lower extremity was then draped and prepped in the usual sterile manner. A straight incision was used for the arthrotomy. The skin and subcutaneous tissues were incised. Medial parapatellar arthrotomy was performed.
The tibia was then exposed. The tibial resection was then performed using the custom tibial guide. Attention was then turned tow rds the femur. The femur was then prepared using the customized guides.
The distal chamfer and notch cuts were then performed. The tibial preparation was then performed, gap balancing was performed, and the gap was found to be correct.
Attention was then turned towards the patella. The patellar resection was performed. Drill holes were made in the patella and trial patella as then placed into position. The trial femur was placed into position, the trial tibia was placed into position, trial poly was placed into position. The knee was then reduced.
The knee was then trialed through a full range of motion. There was no flexion contracture. Full flexion was obtained. The patella tracking was excellent. The trial implants were then removed. The injection was given for postoperative pain relief. A thorough lavage was given. The bone was dried. The femur was then cemented into position.
Excess cement was removed. The tibia was cemented into position. Excess cement was removed. The poly was placed into position. The patella was then held in full extension with a bump under the ankle.
The patella was then cemented into position. Excess cement was removed. The patella was held in position with the patellar clamp. After the cement hardened, thorough irrigation was given.
The medial parapatellar arthrotomy was closed with no 1 Vicryl and barbed suture. Cutaneous tissues were closed with O Vicryl. Subcuticular tissues were closed with 2-0 Vicryl. The skin was closed using staples. Sterile dressing was applied to the wound, and the patient was then transferred to the postoperative care unit in stable condition.


Postoperative X-ray images showing AP and lateral views of the left knee.
Preoperative Surgical plans
The patient was mobilized the same day of the surgery. She was able to walk 150 feet on the day of surgery with support. She was put on aspirin 325mg for deep vein thrombosis prophylaxis. Her pain was well controlled with pain medications. During the postoperative period, her vitals remained stable and she had a regular diet.
She was discharged on a postoperative day 1 with wound care instructions. On her following visits, she displayed full movements of the joint without any discomfort. Her sutures were inspected and found to be clean, dry and intact. Sutures were removed postoperative day 14 without any complications.
On her 3 months follow up, she reported 0/10 pain and displayed a full range of motion of the left knee. She has since returned to her work and back to her baseline activities. She continues her home exercise program and physical therapy for strengthening and increasing flexibility.

