Case Study: Customized Right Total Knee Replacement
in a 73-year-old Male with Arthritis
A 73-year-old retired school teacher, presented with complaints of worsening right knee pain for the past 5 years. He first noticed the pain on his evening walks five years ago. He stated he gradually decreased the distance of walking and used a cane as an assistive device. Recently, for the past few months, the pain was constant and disturbing his sleep.
The patient denied any history of fall/trauma preceding the onset of pain. The pain was described as a dull ache located along the inner side of the right knee. The intensity was moderate about 6/10. The pain was exacerbated with activities such as standing, walking, sitting, getting up from a chair, navigating stairs, bending, twisting and turning.
The patient was distressed from the limitation of his lifestyle secondary to pain. He was unable to go on his evening walks, an activity he enjoyed. He was also unable to drive his car for prolonged periods. The disturbance of sleep made him sleepy during the day and he felt sad about his decreased social interactions.
He had previously tried heat and ice pads, physical therapy, cortisone knee injections and hyaluronic acid injections with minimal relief. The pain was alleviated for only a couple of weeks and returned with the same intensity. He felt he had exhausted all his conservative treatment options.
He was a former smoker having quit last year. He denied any known drug allergies. He was currently taking Lopressor 25 mg BID for tachycardia and Flomax for benign prostate hypertrophy. He denied any illicit drug intake.
On physical examination, his gait was steady. There was mild genu varum deformity. There was tenderness along the medial joint line and patellar facets. There mild swelling of the left knee. The skin overlying the left knee was normal with no evidence of scars or sinus tracts.
The range of motion was terminally restricted secondary to pain (5 degrees to 110 degrees). There was no evidence of any instability/laxity in coronal, sagittal and axial planes. The distal neurological examination was normal. The bulk and tone of muscles were normal.
The examination of the bilateral hip and ankle and left knee were normal. The bilateral lower extremity superficial and deep tendon reflexes were intact. The lower extremity pulses were palpable and good volume bilaterally.
Imaging studies revealed severe tricompartmental osteoarthritis of the right knee. Considering the patient’s lifestyle limiting knee pain, he was advised customized total knee replacement. Risks, benefits, and alternatives were discussed with the patient. He agreed to go ahead with the surgery.
As a part of assessment and planning, a preoperative CAT scan of the lower extremities was obtained a few weeks prior to surgery. Detailed images were acquired for accurate assessment of the patient’s anatomy and biomechanics. Entire data was utilized to construct custom implants and instruments unique for the patient.


Preoperative X-ray of the right knee showing AP and lateral views.
OPERATION: Right total knee arthroplasty.
IMPLANTS USED: Custom femoral implant with 6-mm polyethylene insert with a custom tibial tray and a 32-mm patella.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining informed consent and signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure. The patient was then definitively positioned and the right hip was then draped and prepped in the usual sterile manner.
A tourniquet was used to exsanguinate the extremity and then a straight incision was used for the arthrotomy. Skin and subcutaneous tissues were incised. Medial parapatellar arthrotomy was then performed.
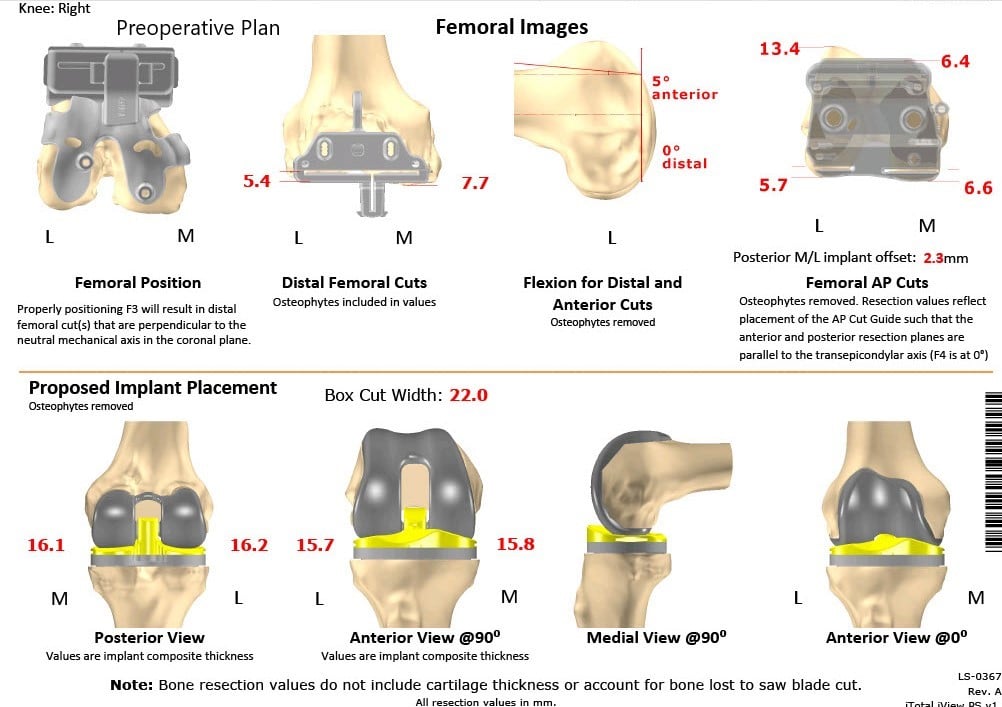
Complete Orthopedics patient-specific surgical plan for a customized right total knee replacement in a 73-year-old male with arthritis.
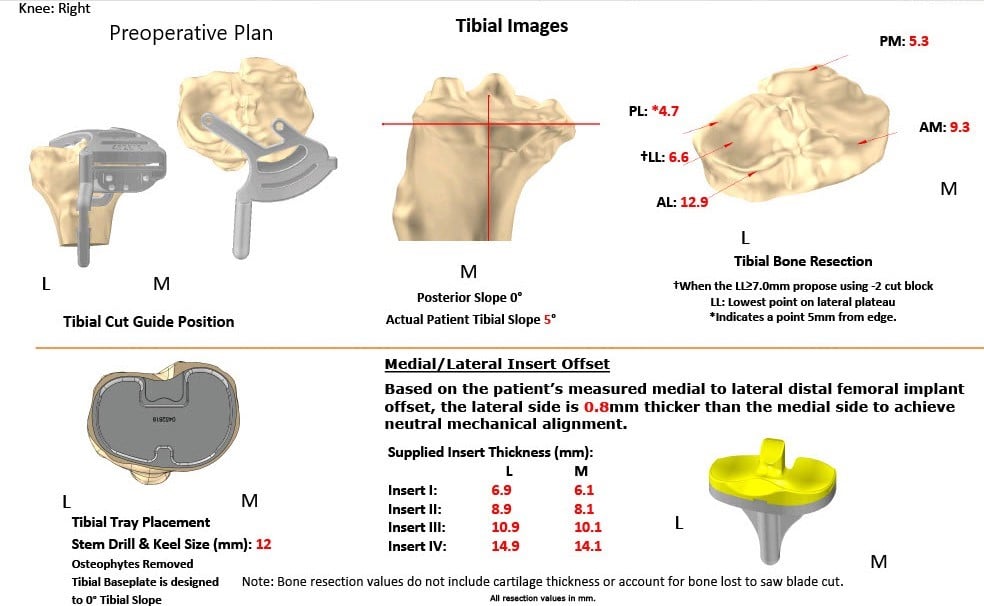
Complete Orthopedics patient-specific surgical plan for a customized right total knee replacement in a 73-year-old male with arthritis (scan 2)
The tibia was then exposed. The tibial cutting guide was used to make the tibial cut. The tibia was then prepared. Attention was then turned towards the femur. The femur was then prepared using a distal chamfer cutting guide and notch cutting guide.
Lamina spreaders were used medially and laterally and the remainder of the cruciate and meniscus was debrided.
Gap balancing was performed and gap balancing was found to be perfect. Patella was then prepared. Drill holes were made in the patella.
The trial patella was placed into position. Attention was then turned towards the femur. The trial femur was placed into position. The trial tibia was placed into position.
Poly was then placed into position. The knee was then trialed through a full range of motion and stability was excellent. Patellar tracking was excellent.
Trial components were then removed. The injection was given. The femur was cemented into position. Excess cement was removed. The tibia was cemented into position.
Excess cement was removed. The poly was then placed over the tibia and the knee was then reduced and held in full extension with a bump under the ankle. Patella was instrumented into position and held in position with a patellar clamp. Excess cement was removed.
After the cement hardened, medial parapatellar arthrotomy was closed with Vicryl and Stratafix. Cutaneous tissues, subcuticular tissues, and skin were closed in layers. The tourniquet was done. Sterile dressing was then applied over the wound and the patient was then transferred to the postoperative care unit in stable condition.


Postoperative X-ray of the right knee showing AP and lateral views.
Post-op the patient’s vitals were stable and the distal neurological status was intact. He was able to walk bearing weight the same day of the surgery. Aspirin was prescribed to prevent deep vein thrombosis. Physical therapy was started to increase range of motion and prevent stiffness.
After eight weeks of post-op, the patient was able to walk without support and reported zero pain. The range of motion of the right knee was full and patient-reported decreased pain in the left knee. He was happily back to his evening walks and enjoyed his routine without the hindrance of knee pain.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
