Case Study: Customized Total Knee
Replacement in a 59-year-old male
A 59-year-old male who worked as a nurse at a hospital presented today with complaints of left knee pain for the past 5 years. The patient states he first noticed the pain in the left knee while climbing up the stairs. The pain was insidious in onset and gradually progressed to a dull ache which was moderate in intensity (5/10).
The patient worked as a volunteer for a children’s hospital and enjoyed playing tennis. But since the past 1 year, he had been restricting his activities and was unable to play tennis. He described difficulty in daily activities such as climbing stairs, walking, squatting and kneeling. The patient stated he enjoyed performing yoga regularly but had difficulty squatting in different postures.
The patient had in the past undergone various treatment modalities for the left knee in the form of injections and physical therapy. The patient stated he experienced only temporary relief and was looking for an option of total knee replacement.
The patient was a nonsmoker with a medical history of hypertension, dyslipidemia, gastroesophageal reflux disease, and insomnia. The conditions were well controlled with medications and she was motivated for physical therapy and home exercise program.
On physical examination, the patient had a steady gait, there were no scar, sinuses or erythema. There was no varus or valgus deformity in both the sitting and standing positions. There was no local rise in temperature. Medial joint line and patellar facet tenderness were positive. On standing, after milking the suprapatellar pouch, the patellar tap was positive indicating mild effusion. The range of motion was complete with no fixed flexion deformity.
He was stressed about the pain which had recently started disturbing his sleep. He stated the pain was lifestyle limiting. Imaging studies revealed severe tricompartmental osteoarthritis. Various nonoperative and operative management options were discussed with the patient in-depth. He was deemed a candidate for custom left knee total replacement.
Risks and benefits were explained to the patient and he agreed to go ahead with the procedure. The patient recently had a cortisone injection in the left knee, so he was asked to wait for 3 months to decrease the chances of infection.


Preoperative X-ray showing AP and lateral images of the left knee
The patient underwent a CT scan 3 weeks prior to the procedure. A preoperative plan was formulated based on the patient’s anatomy and biomechanics. The plan outlined the bone cuts for maximum bone preservation and accurate duplication of natural knee biomechanics. The CT scan images were used to construct custom implants and instruments uniquely designed for the patient.
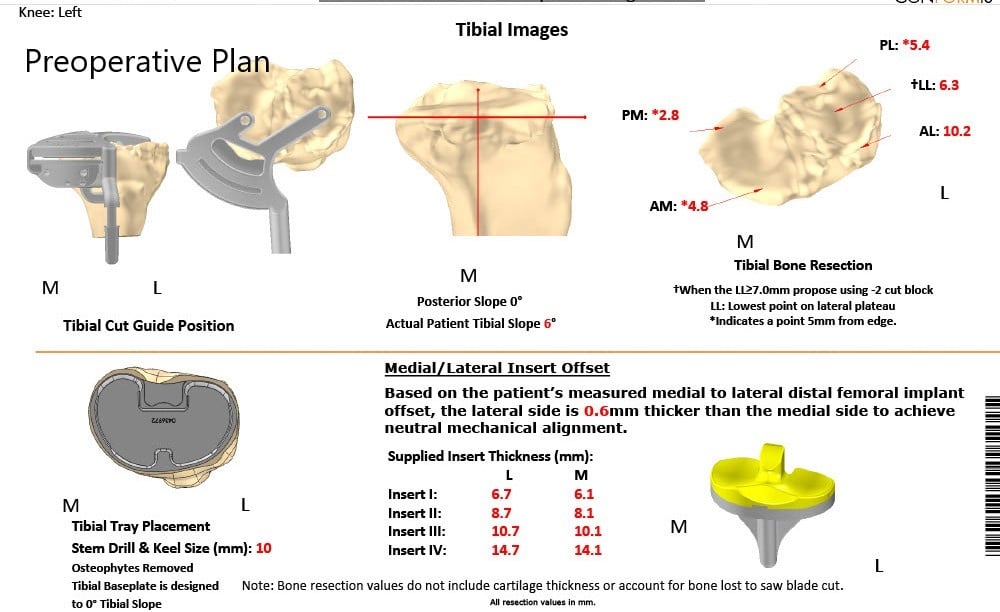
Complete Orthopedics patient-specific surgical plan for customized total knee replacement in a 59-year-old male.
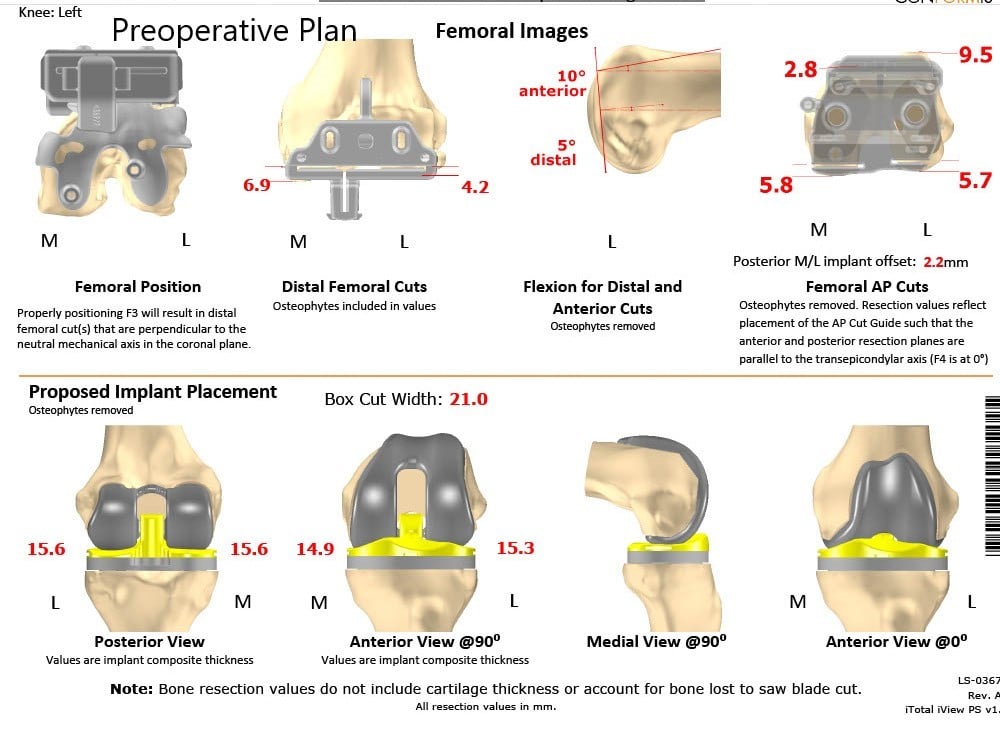
Complete Orthopedics patient-specific surgical plan for customized total knee replacement in a 59-year-old male (scan 2)
The patient underwent a custom left total knee arthroplasty.
IMPLANTS USED: Custom femur with custom tibia with a posterior stabilized polyethylene with a 29-mm patellar insert.
The patient was brought to the operating room after obtaining informed consent signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure. The patient was anesthetized and the tourniquet was placed over the left thigh. The left lower extremity was then draped and prepped in the usual sterile manner. An Esmarch was used to exsanguinate the extremity. A straight incision was used for the arthrotomy. Skin and subcutaneous tissues were incised. The fascia was then divided.
A medial parapatellar arthrotomy was then performed. The tibia was then exposed and the tibial cutting guide was used for making the tibial cut. The cut was then checked. Attention was then turned to the femur. The distal femur and chamfer cuts were made using the custom cutting guides.
A notch cutting guide was used to make the notch cut medially and laterally. Laminar spreaders were used and the remainder of the meniscus and the cruciates were then departed laterally. Gap balancing was performed and gap balancing was found to be correct after removing the posterior osteophytes.
The patella was then resected. Drill holes were made in the patella. The trial patella was placed into position. The trial femur was placed into position and the remainder of the tibia was then prepped. A trial tibia was then placed into position. The poly was placed into position and the knee was then reduced. The knee was trialed through a full range of motion. There was excellent stability. Patellar tracking was excellent. There was a full extension and full.l flexion achieved intraoperatively.
Trial components were then removed. A thorough lavage was performed. The injection was given. The femur was cemented into position. Excess cement was removed. The tibia was cemented into position. Excess cement was removed. Poly was then placed over the tibia. The knee was then reduced and held with a bump under the ankle. The patella was then placed into position and held with a patellar clamp. Excess cement was then removed.
After the cement hardened, the lavage was given. The patellar clamp was removed. Medial parapatellar arthrotomy was closed with #1 Vicryl and cutaneous tissues were closed with 2-0 Vicryl. Subcuticular tissues were closed with 2-0 Vicryl. The skin was closed using staples. Sterile dressing was then applied over the wound. The patient was then transferred. to the postoperative care in stable condition.


Postoperative X-ray showing AP and lateral view of the left knee
Postoperatively, he was walking the same day and was started on aspirin for deep vein thrombosis prophylaxis. He had excellent pain relief with multimodal pain management. The patient was subsequently seen for sterile dressing change and his wound was found to be dry, clean and intact. Staples were removed and the patient demonstrated a full range of motion.
The patient was extremely happy with the outcome and after 3 months he successfully concluded his physical therapy. He had since returned to playing tennis and volunteering at a children’s hospital. He was able to resume his work as a nurse and was active without any pain or stiffness. The patient follows up as needed.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
