Case Study: Custom Left Knee Total
Replacement in a 68-year-old Female
A 68-year-old female presented to our office with complaints of left knee pain for the last 12 years. The patient sustained an injury to her left knee while playing with her grandkids. She went to a physician and was advised conservative management for knee pain. The pain had since worsened and recently became constant.
The pain was relieved for a few months with conservative management in the form of physical therapy, ice and heat pads, and laser therapy. The pain returned and she received cortisone knee injections with minimal relief. Her physician told her she would need a total knee replacement surgery.
She was a retired store manager and was currently living with her daughter. She was active physically and enjoyed riding a bicycle and going for a walk. Recently for the past few months, she was unable to go for a walk and perform her daily activities.
The pain was located along the inner side of the left knee and sharp in character. The frequency was constant with the disturbance of her sleep. The pain was moderate to severe in intensity. Activities such as getting up from a chair, kneeling, bending, navigating stairs made the symptoms worse.
She was a nonsmoker and nondrinker. She had no known drug allergies. Her past medical history was positive for depression and anxiety, and high blood pressure. She was currently taking sertraline and Vasotec. She had a tubal ligation and myomectomy done 30 years ago.
On physical examination, there was mild genu varum deformity. The gait was antalgic with a reduced stance phase on the left side. The patient used a cane as an assistive device. The skin overlying the left knee was normal. There was mild swelling of the left knee.
Tenderness was positive on the medial joint line and patellar facets. There were no signs of instability or laxity in coronal, sagittal, and axial planes. There was bursitis on the bilateral trochanter of the hips. The examination of the bilateral ankles and right knee was normal.
There was no distal neurological deficit and the bilateral pulses were good volume and comparable. Imaging studies revealed severe tricompartmental osteoarthritis of the left knee. Considering the patient’s lifestyle limiting knee pain, she was advised customized left knee total replacement. Risks, benefits, and alternatives were discussed with her at length. She agreed with the plan.
A CAT scan was obtained a few weeks prior to the procedure. Accurate information regarding the patient’s anatomy and biomechanics was obtained. Unique patient-specific Implants and instruments were constructed for the surgery. They would ensure accurate bone cuts with minimal bone loss. A preoperative plan was made for the surgery.


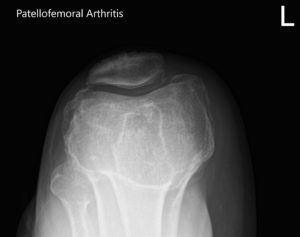
Preoperative X-ray of the left knee showing AP, lateral and merchant views.
OPERATION: Left total knee arthroplasty.
PROSTHESIS: Custom tibial tray with a custom femoral component with 6-mm polyethylene insert with a 32 -mm patella.
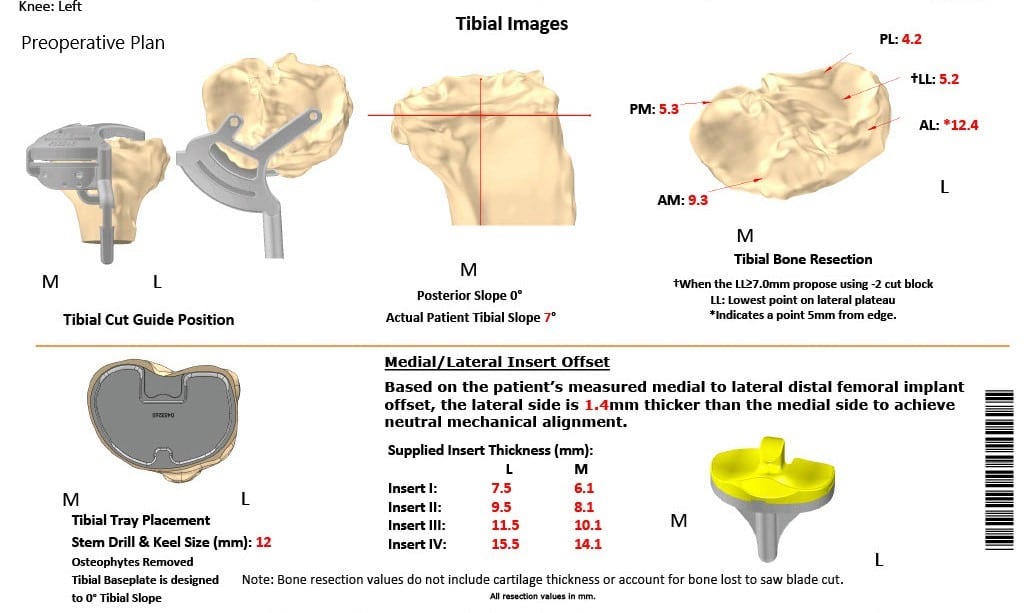
Complete Orthopedics patient specific surgical plan for a custom left knee total replacement in a 68-year-old female.
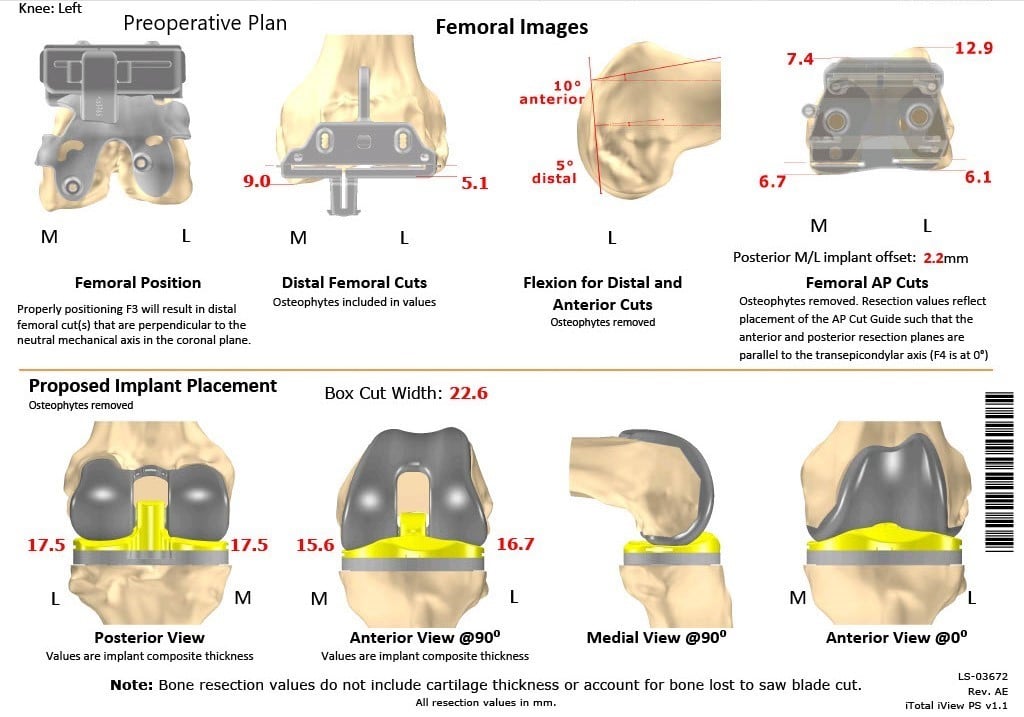
Complete Orthopedics patient specific surgical plan for a custom left knee total replacement in a 68-year-old female (scan -2)
DESCRIPTION OF PROCEDURE: The patient was brought to the operating mom after obtaining informed consent and signing the correct surgical site. The risks. benefits and alternatives were extensively discussed with the patient prior to the procedure.
Anesthesia was performed. The left lower extremity was then prepped and draped il the usual sterile manner.
Esmarch was used to exsanguinate the extremity. Tourniquet was elevated. A straight incision was used for the arthrotomy. Skin and subcutaneous tissues were incised.
Medial parapatellar arthrotomy was then performed. The tibial resection was made using the customized cutting guide and the tibia was then prepared. Attention was then turned towards the femur.
The femur was then prepared using the femoral cutting guide. The notch cut was then performed. Lamina spreaders were then used medially and laterally and the remainder of the cruciate and the meniscus was then debrided. Gap balancing was performed and found to be corrected.
Attention was then turned towards the patella. Patellar resection was then performed. Drill holes were then made in the patella and the trial patella was then placed into position. Attention was then turned towards the femur. The trial femur was placed into position followed by the trial tibia.
Poly was then placed into position. The knee was then ranged through a full physiological range of motion. The stability was excellent. Patellar tracking was excellent. Trial components were then removed. Thorough lavage was given. The injection was given. The femur was cemented into position followed by the tibia.
The poly was then placed over the tibia. The knee was then reduced and held in full extension with a bump under the ankle. Patella was then cemented into position and was held in position with the patellar clamp.
After the cement hardened, the clamp was removed. Thorough lavage was given. Medial parapatellar arthrotomy was closed with Vicryl and Strataflx. The wound was then closed in layers. The tourniquet was let down. The patient was then transferred to the postoperative care unit in a stable condition.


Postoperative X-ray of the left knee showing AP and lateral views.
Post-surgery, she was able to walk the same day with support. Her vitals remained stable and she was able to go home the same day. Her distal neurological status was intact. She was started on aspirin to prevent deep vein thrombosis.
Sutures were taken down uneventfully. After eight weeks, she was able to walk with support and reported zero pain. The physical therapy was continued. She had a full range of motion and was back to her baseline activities. She was extremely satisfied with her outcome of the surgery.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
