Case Study: Right Total Knee Replacement with
Custom Instruments in a 66-year-old male
A retired commercial pilot presented for consultation regarding his worsening right knee pain. The pain started when he had a slip and fall about 3 years ago. He went to a hospital where he was told he had a hairline fracture. He subsequently had an MRI which revealed no fracture or ligament tear.
The patients carried on his activities but noticed pain again after a month. He substantially undertook outpatient physical therapy. He also received gel injections in his knee. Both physical therapy and gel injections provided minimal relief to the patient.
He reported the subsequent use of an assistive device in the form of a cane. He received cortisone knee injections twice, with relief lasting roughly for a month. He currently took over the counter pain medications for his knee pain.
The pain was described as a dull ache with no radiation. The pain was constant and also disturbed his sleep. He was unable to walk more than two blocks without discomfort. The pain was especially worse on activities such as climbing stairs, getting up from a chair, turning, twisting, bending and kneeling. The pain was better in rest.
He was a lifelong teetotaler and a nonsmoker. He reported no known drug allergies. He was currently taking medications for high blood pressure, hypothyroidism, asthma, and benign prostate hypertrophy. All his conditions were well managed with medications.
His physical examination revealed an antalgic gait with reduced stance phase on the right side. There was mild swelling with a positive patellar tap. Tenderness was present on the medial and lateral joint line. The patellofemoral grind test was positive for tenderness.
There was crepitus throughout the arch of motion of the right knee. The range of motion was from 10 degrees to 100 degrees. The quadriceps and patellar tendons were intact with no tenderness. The examination of the left knee, bilateral hips and ankles were normal.
There was no distal neurological deficit. The bilateral distal pulses were palpable and comparable. The bulk and tone of the bilateral lower extremities were normal. There was no bladder or bowel dysfunction.
The patients lived with his son and were quite dismayed at his lack of physical activity due to pain. He was unable to enjoy his time with his friends or drive for an extended period of time.
The imaging results revealed severe tricompartmental osteoarthritis of the knee. Considering his lifestyle limiting knee pain, he was advised right total knee replacement with custom instruments. The risks, benefits, and alternatives were discussed with the patient at length. He agreed with the plan.
A preoperative MRI was done a few weeks prior to the procedure to get data for custom implants. Custom implants ensured less tissue trauma and accurate bone cuts for the procedure.


Preoperative X-ray showing the anteroposterior and lateral view of the right knee.
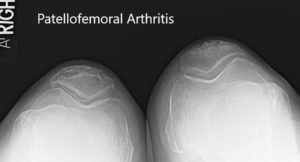
Preoperative x-ray showing the merchant view of both the knees.
OPERATION: Right total knee replacement.
IMPLANTS USED: Femur posterior stabilized size 3 with a Persona tibia 5-degree stemmed size C with polyethylene 10-mm posterior stabilized insert with 14-mm diameter stem extension with 29-m cemented patella.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining informed consent and signing the correct surgical site, the risks, benefits, and alternatives were extensively discussed with the patient as well as her husband prior to the procedure. The anesthesia was obtained by the anesthesiologist.
The patient was then definitely positioned, and the right lower extremity was then draped and prepped in the usual sterile manner with the cuff of tourniquet over the right thigh. Before the surgery, the time-out was performed and the limb was exsanguinated.
A straight incision was used for the arthrotomy. Skin and subcutaneous tissues were then incised. Medial parapatellar arthrotomy was then performed. The femoral PSI guide was then placed into position and the distal femoral cut was then performed. The anterior and posterior chamfer cuts were then performed.
The tibial cut was then performed using the PSI guide and gap balancing was performed. The notch cut of the femur was then made, and then the laminar spreaders were used medially and laterally, and posterior soft tissue osteophytes were then excised. Gap was balanced.
Patellar resection was made. Drill holes were made in the patella. The trial patella was placed into position. The trial femur was placed into position, followed by the tibia. The poly was placed into position, and the knee was trialed through a full range of motion. There was no flexion contracture that existed earlier, and the patellar tracking was excellent.
The trial components were then removed. A periarticular injection was then performed. The bone was then dried. The femur was cemented into position; excess cement was then removed. The tibia was cemented into position; excess cement was removed.
The poly was then placed into position. The knee was then reduced and with a bump under the ankle. Patella was then cemented into position; excess cement was removed.
After the cement hardened, the patellar clamp was removed. Medial parapatellar arthrotomy was closed. Cutaneous tissues were closed, subcuticular tissues were closed, and the skin was closed using layers. Sterile dressing was then applied over the wound, and the patient was then transferred to the postoperative care unit in a stable condition.


Postoperative x-rays showing the anteroposterior and lateral views of the right knee.
The recovery was excellent with same-day weight-bearing. He was able to walk 100 feet without discomfort. He was given aspirin for deep vein thrombosis prophylaxis. The pain was managed well with medications. Physical therapy was started on an outpatient basis.
The patient was compliant with his home exercise program. Two months later, he reported with a full range of motion and zero pain. He was able to walk, climb stairs, and drive his car without any limitation. He was extremely happy with the outcome of the procedure.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
