Case Study: Customized Left Total Knee Replacement
in a 73-year-old Male
A 73-year-old male presented to our office with complaints of bilateral knee pain (left greater than right). The patient first noticed the pain 6 years ago which gradually worsened in severity. He had a meniscal surgery done 4 years ago with limited relief. The pain had increased in severity over the past 6 months hindering his daily activities.
The patient stated that the pain started insidiously without any trauma or twisting injury. He denied any feeling of laxity or instability. The pain initially located over the inner side of both the knees progressed to the entire knee. The pain was worse with activities such as climbing stairs, walking more than a block, turning, twisting, bending, kneeling and squatting. The pain was described as a dull ache.
The patient was a retired mechanic, currently living with his wife. He was active before the onset of severe pain and enjoyed traveling, tending to his indoor garden, and walking his dog. However, he now found it difficult to even walk to the nearby grocery shop or get up from a chair after sitting for a long time.
Besides the meniscal surgery, he had tried physical therapy, cortisone and gel injections with very short term relief. He stated he had recently heard about the replacement surgery and wanted to explore it had exhausted all conservative management options.
He was present cigar smoker, and occasional drinker (beer). His medical history was positive for hypertension, hyperlipidemia, and obstructive sleep apnea. All his conditions were well controlled with medications and he was currently on Toprol XL 50 mg and Losartan 20 mg + Hydrochlorothiazide 25 mg. He used a CPAP machine for obstructive sleep apnea.
On physical examination, his gait was steady and he used a cane for ambulation. There was visible genu varum deformity. The skin overlying the knees was normal. There was no fullness or swelling in bilateral knees. Tenderness was positive on the left medial joint line and lateral joint line.
Patellar facet tenderness was positive with crepitus on range of motion. The range of motion was full of terminal pain. Anterior drawer, posterior drawer, Lachman test, valgus and varus stress, and pivot shift were negative. The examination of the bilateral hip and ankle was normal.
There was no distal neurological deficit and the bilateral distal pulses were comparable. The bilateral lower extremity superficial and deep tendon reflexes were positive and comparable. Imaging revealed osteoarthritis of bilateral knees (left > right). Smoking cessation education was given to the patient.


Preoperative X-ray showing the AP and lateral views of the left knee.
After careful consideration of the patient’s needs and comorbidities, he was advised custom left total knee replacement. Risks, benefits, and alternatives were discussed with the patient in detail. The patient agreed to undergo surgery.
As a part of the preparation for the procedure, a preoperative CT scan was obtained. The data obtained from the scan was utilized to obtain accurate information about the patient’s anatomy and biomechanics. Customized implants and bone cutting jigs were constructed uniquely to the patient. A preoperative plan was formulated to guide the surgical steps.
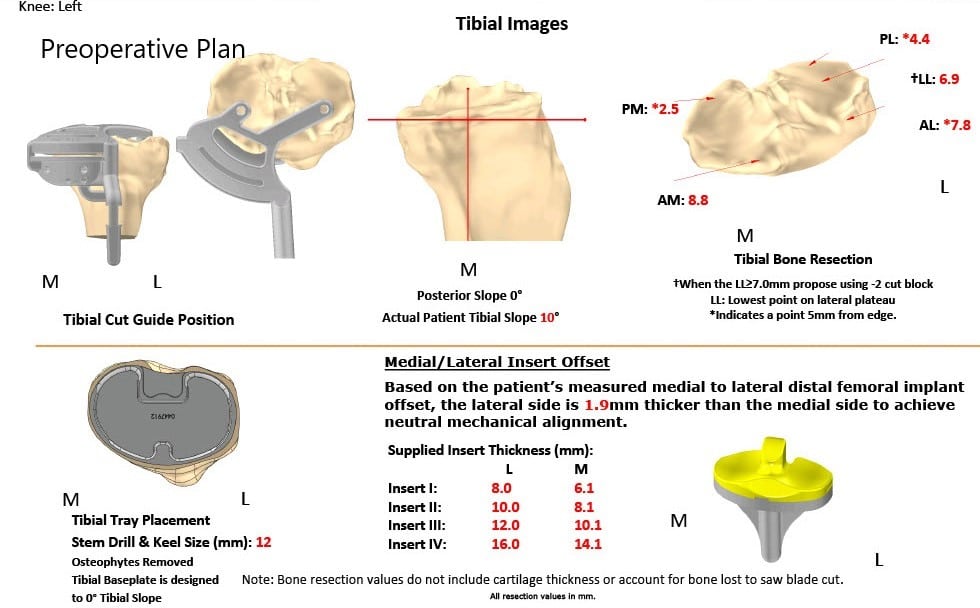
Complete Orthopedics patient-specific surgical plan for a customized left total knee replacement in a 73-year-old male.
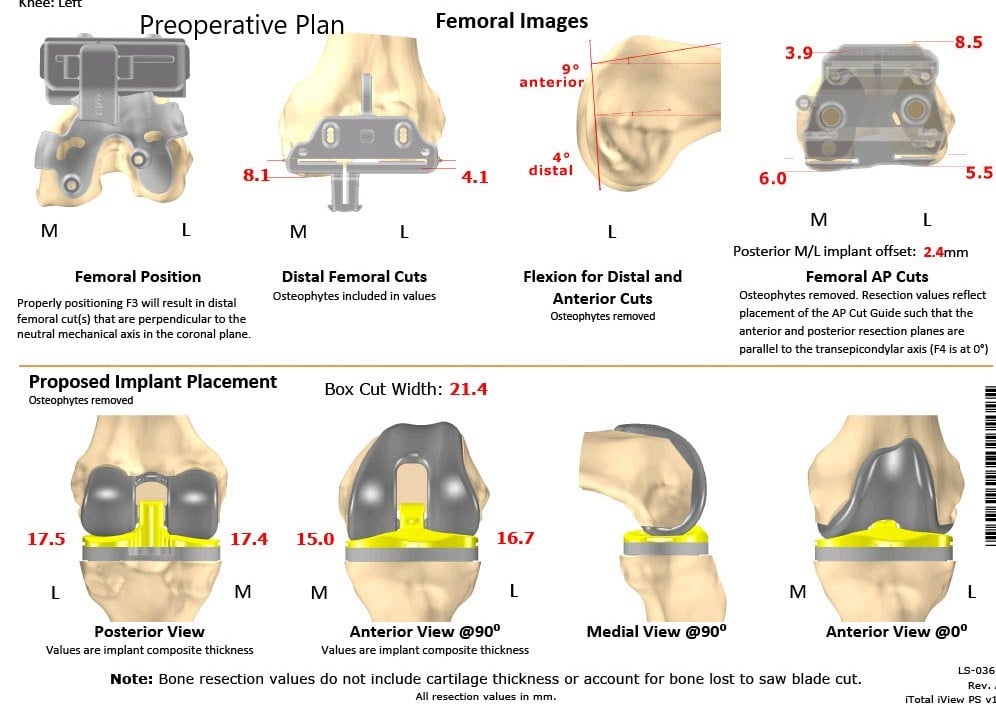
Complete Orthopedics patient-specific surgical plan for a customized left total knee replacement in a 73-year-old male (scan 2)
OPERATION: Left total knee arthroplasty.
IMPLANTS USED: Custom tibial tray with a custom femoral implant with 6-mm polyethylene insert with a patella of size 32-mm.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after signing informed consent and signing the correct surgical site. The risks, benefits, alternatives were extensively discussed with the patient prior to the procedure. Anesthesia was obtained by the anesthesiologist.
The left knee was then draped and prepped in the usual sterile manner with tourniquet over the left thigh. Esmarch was used to exsanguinate the limb and the tourniquet was elevated.
The straight incision was used for the arthrotomy. Skin and subcutaneous tissues were incised. Medial parapatellar arthrotomy was then performed.
The femur was then exposed followed by the tibia. The tibial resection was then performed with customized jigs. The femoral cuts were then performed with the customized jigs, distal cut followed by the anterior, posterior and the chamfer cuts as well as the notch cuts.
Laminar spreaders were used medially and laterally and the remainder of the meniscus and the cruciates were then debrided.
Posterior osteophytes were then removed. Gap balancing was performed and was found to be corrected. The tibia was then prepped. Attention was then turned towards the patella.
The patellar resection was then performed. The drill holes were made in the patella. The trial patella was then placed into position followed by the trial femur and the tibia.
The poly was then placed into position. The knee was then reduced and trialed through a full range of motion. Full-extension was obtained, full flexion was obtained. Patellar tracking was found to be correct. The trial components were then removed.
At this point, there was some tourniquet malfunction which led to some bleeding. The tourniquet was, therefore, let down. Thorough lavage was given. The Esmarch was then used again and the tourniquet was again elevated at a higher pressure. The field was satisfactory for instrumentation.
The bone was then dried. The femur was cemented into position, and excess cement was removed. The tibia was cemented into position. Excess cement was removed. Poly was placed over the tibia. The knee was then reduced and held in full extension with a bump under the ankle. The patella was then cemented into position.
Excess cement was removed, and the patella was held in position with a patellar clamp. After the cement hardened, the patellar clamp was removed. Thorough lavage was given. The injection was given. Medial parapatellar arthrotomy was closed with Vicryl and Stratafix. Cutaneous tissues were closed with O Vicryl and subcuticular tissues were closed with 2-0 Vicryl and skin was closed using staples. The tourniquet was then let down, and the patient was then transferred to the postoperative care unit in stable condition.


Postoperative X-ray showing the AP and lateral view of the left knee.
Recovery was excellent in the post-op period. The vitals were stable and there was no distal neurological deficit. He was able to walk the same day of the procedure. Aspirin 325 mg BID was started for deep vein thrombosis prophylaxis. The pain was managed with medications. Physical therapy was initiated for increasing range of motion and strengthening.
Three months post-op, the patient demonstrated a full range of motion with zero pain. He was able to walk, drive a car and do daily activities without experiencing any pain. He reported decreased pain in the right knee secondary to offloading of the weight. He follows up as needed.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
