Hinged Knee Replacement
Hinged knee replacement is a type of knee replacement used for complex knee problems. It is designed for patients who have severe arthritis, major deformity, major bone loss, or ligament problems that make standard knee replacement implants insufficient. This type of implant uses a hinge or rotating mechanism to provide stability when the natural supporting structures cannot support the joint.
How Common It Is and Who Gets It? (Epidemiology)
Hinged knee replacement is far less common than standard knee replacement. It is mostly used in revision surgeries or in complex primary cases involving severe deformity, tumors, instability, or major bone loss.
Why It Happens – Causes (Etiology and Pathophysiology)
Some patients develop advanced arthritis, deformity, or ligament failure that causes severe knee instability. Others may have complications from a previous knee replacement such as infection, loosening, or fracture. These conditions make standard implants unable to stabilize the knee, leading to the need for a hinged implant.
How the Body Part Normally Works? (Relevant Anatomy)
A healthy knee allows forward and backward motion, rotation, and small side-to-side movements. These movements depend on strong ligaments, healthy cartilage, and proper bone alignment. When these structures are severely damaged, the knee becomes unstable and cannot function normally.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms may include severe pain, swelling, stiffness, difficulty bending or straightening the knee, instability, difficulty walking, a feeling that the knee may give way, pain at rest, and poor response to nonsurgical treatments. X-rays may show advanced joint damage.
Chronic Knee Pain: Persistent and severe knee pain, especially during weight-bearing activities such as walking, climbing stairs, or standing for long periods.
Decreased Range of Motion: Difficulty in fully extending or bending the knee joint, resulting in limited movement and flexibility.
Swelling and Inflammation: Swelling around the knee joint that doesn’t improve with rest, ice, or elevation. Chronic inflammation can indicate underlying joint damage.
Stiffness: Feeling stiffness in the knee joint, especially after prolonged periods of inactivity, such as sitting or sleeping.
Instability: Sensation of the knee giving way or feeling unstable during movement, which can increase the risk of falls.
Difficulty Walking: Persistent difficulty walking due to pain and limited mobility, which may require the use of assistive devices like canes or walkers.
Pain at Rest: Experience of knee pain even while at rest, which can disrupt sleep and daily activities.
Previous Failed Treatments: Inadequate relief from conservative treatments such as physical therapy, medications, corticosteroid injections, or arthroscopic surgery.
X-ray Findings: Radiographic evidence of advanced joint degeneration, bone-on-bone contact, or other structural abnormalities in the knee joint.
Functional Impairment: Significant impairment in performing activities of daily living, recreational activities, or work-related tasks due to knee pain and limitations in movement.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis is based on symptoms, physical examination, and imaging tests. X-rays show bone loss, deformity, and arthritis. These findings help determine whether a hinged knee implant is needed.
Classification
Knee replacement implants may be:
Non-constrained implants for standard cases.
Semi-constrained implants for moderate instability.
Fully constrained hinged implants for severe bone loss or ligament failure.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may resemble the need for a hinged knee include standard osteoarthritis, ligament tears, meniscus injuries, or pain after partial knee replacement.
Treatment Options
Non-Surgical Care
Options include medications, physical therapy, injections, or bracing. These may help early symptoms but are usually not effective for advanced deformity or instability.
Surgical Care
Hinged knee replacement is used when the soft tissue or bone cannot stabilize a standard implant. The prosthesis has a hinge or rotating mechanism connecting the femoral and tibial components. Hinged implants may be used in revision surgery, severe deformity, tumors, infection, fracture, or major ligament laxity.
Hinged Knee Replacement
The implants used in a total knee replacement come in different shapes and sizes. The choice of implant used in a total knee replacement depends upon the amount of the bone, quality of the bone, the soft tissue around the knee, any prior surgeries, and also on the medical history of the patient. A hinged knee replacement is a complex knee replacement that requires a special implant with either a hinge or a rotating platform.
During a knee replacement surgery, the surgeon removed the diseased ends of the lower end of the thigh bone and the upper part of the shin bone. The prosthetic replacement of the removed parts recreates the natural knee joint without any disease.
The prosthetic parts are made of metal and high-grade plastic. The femoral and the tibial component are made up of metal while the insert or the spacer is made up of high-grade plastic. The plastic spacer helps in the smooth gliding of the opposing metal surfaces.
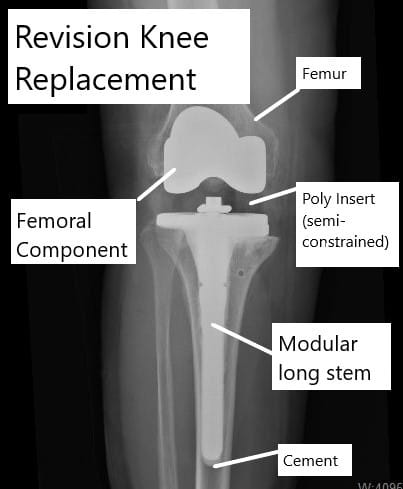
Revision knee replacement showing use of semi-constrained components.
A natural knee has motion in the forward and the backward direction as well as a small amount of rotation and side-to-side motion. The thigh bone also slides back on the upper part of the shin bone during bending of the knee which is known as femoral rollback.
Constrain is the ability of the implant to provide stability in forward-backward and side-to-side motion. The constrained implants are needed in the face of bone loss or labor of the ligaments. Implants may be non-constrained, semi-constrained, or fully constrained depending upon the amount of stability they provide.
During a primary knee replacement for arthritis, only the bony ends are diseased and may be associated with mild to moderate deformity. The surgeon removes only the diseased ends and may stretch or release ligaments to correct the deformity.
The bone quantity and the soft tissue support is however adequate to provide stability to the prosthetic joint. Therefore the commonly used knee replacement implants in primary surgery are non-constrained.
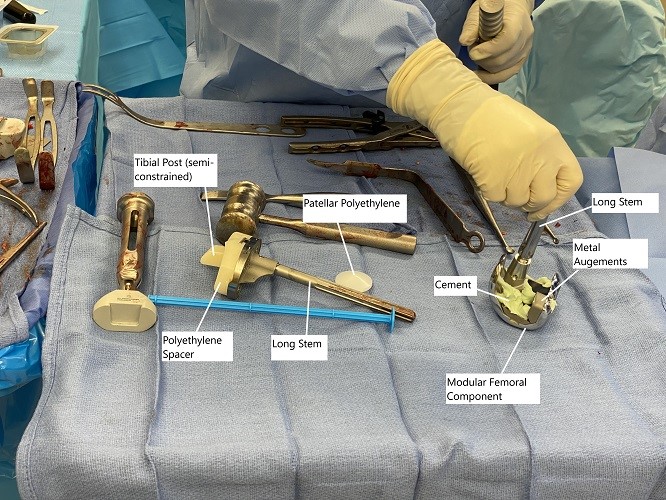
Intraoperative image showing modular knee replacement implants.
All prosthetic implants are limited by their self-life as they wear down over the years. The life of a usual knee implant may be well over more than 20 years and for patients over 60 years of age, they may last their lifetime.
Owing to the success of the surgery, knee replacement is increasingly being performed in the younger age groups. In younger age groups after many years, the implants may need revision surgery. Additionally, revision surgery may be needed in patients with complications of primary surgery such as infection, aseptic loosening, fracture, instability, etc.
During revision surgery, at times there may be an excessive bone loss that may warrant a modular constrained implant. Similarly, in patients with excessive ligament laxity, a constrained implant may be necessary to provide stability. Patients suffering from some kinds of tumors of the bone may require removal of the stabilizing structures of the joint along with the bone tumor. These patients may also require constrained implants.
The constrained implants come in different designs. The originally used hinged constrained implant has been largely superseded by a rotating constrained implant. In a hinged knee replacement implant, there is a connecting rod in between the femoral and tibial components.
The connecting rod has a hinge mechanism to prevent overextension of the joint. This design only allows forward and backward motion and prevents any side to side and rotating motion.
The loss of side to side and rotating motion puts additional stress at the bone-implant interface and may lead to implant loosening or periprosthetic fracture. The rotating constrained implant additionally allows rotating motion about the prosthetic hinge. The hinge is located near the femoral component and a rotating platform is attached to the tibial plate.
The rotating action helps to distribute the stresses more evenly during motion while maintaining stability in the face of bone loss or ligament laxity. The hinged implants are primarily used in revision surgeries and in complex primary knee replacement surgery involving severe deformity or tumors, or salvage surgeries, etc.
The hinged knee replacement implants are also modular that allows the addition of metal wedges or triangles to compensate for bone loss. The stem modularity also allows the addition of long stems to provide stability.
The constrained implants wear out earlier compared to non-constrained but provide excellent stability in difficult cases. The results of constrained hinged knee replacement are better when performed by a surgeon with expertise in performing complex knee replacement surgeries.
Recovery and What to Expect After Treatment
Recovery includes physical therapy, pain control, and the use of walkers or crutches early on. Follow-up visits, wound care, and activity guidelines are important. Therapy helps restore strength and movement.
Possible Risks or Side Effects (Complications)
Risks include infection, nerve or vessel injury, loosening, implant wear, stiffness, fractures, and the need for future revision. Constrained implants may wear out sooner than non-constrained implants.
Long-Term Outlook (Prognosis)
Hinged implants give excellent stability for difficult cases. They are most successful when performed by surgeons experienced in complex knee replacement. Although these implants may not last as long as standard implants, they provide reliable function in situations where no other implant type is suitable.
Out-of-Pocket Cost
Medicare
CPT Code 27447 – Hinged Knee Replacement: $303.02
Medicare generally covers most of the approved amount for this advanced knee replacement, and the patient is responsible for the standard twenty percent portion. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield usually take care of that remaining share. These plans work with Medicare to eliminate the co-insurance gap, which often results in little to no remaining cost when the procedure is Medicare-approved.
Secondary coverage, including employer-based insurance, TRICARE, or the Veterans Health Administration, steps in after Medicare. These plans may pay the remaining balance once their deductible is met. Most secondary deductibles fall between $100 and $300, and after that amount is satisfied, the policy may cover the rest of the charges related to the hinged knee replacement.
Workers’ Compensation
If the need for a hinged knee replacement results from a work-related injury, Workers’ Compensation pays the full cost of surgery and recovery. You will not have any out-of-pocket expense.
No-Fault Insurance
If a motor vehicle accident caused the knee condition that requires a hinged knee replacement, No-Fault Insurance covers the entire procedure. You may only be responsible for a small deductible depending on your specific policy.
Example
A patient required a hinged knee replacement due to severe instability and joint damage. Under Medicare, the expected out-of-pocket cost was $303.02. Because the patient had secondary insurance, the remaining portion was fully covered, leaving the patient with no out-of-pocket expense.
Frequently Asked Questions (FAQ)
Q. Why would someone need a hinged knee replacement?
A. It is needed when there is severe deformity, major bone loss, ligament failure, or complications from prior knee surgery.
Q. Is a hinged implant used in first-time knee replacement?
A. Only in rare, complex cases.
Q. Does it provide more stability?
A. Yes. It stabilizes the knee when ligaments cannot.
Q. Do hinged implants last as long as standard ones?
A. They may wear faster but they are essential for severe cases.
Q. Is recovery different from standard knee replacement?
A. The basic recovery steps are similar, but therapy is essential for strength and stability.
Summary and Takeaway
Hinged knee replacement is used for severe knee damage when standard implants cannot provide stability. It uses a hinge or rotating mechanism to restore movement and control. It is mainly used in revision surgery and complex primary cases. With proper care, it can greatly improve function and stability.
Clinical Insight and Recent Findings
A recent study presented a complex case in which a patient with severe post-infectious knee deformity—including major bone loss, absent menisci, and instability—underwent reconstruction with a rotating-hinge knee replacement and achieved good pain relief, stable alignment, and functional improvement at more than two years of follow-up.
This aligns with your explanation that hinged knee implants are reserved for situations where the ligaments or bone stock can no longer support a standard prosthesis, such as in revision surgery, tumor reconstruction, or advanced deformity.
The study reinforces that modern hinged and rotating-hinge designs can provide dependable stability and restore mobility when other knee replacement options are not feasible. (“Study of hinged knee reconstruction in severe deformity – See PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons specializing in complex knee replacement perform hinged knee replacement. The team includes anesthesiologists, nurses, and physical therapists.
When to See a Specialist?
A specialist should be consulted for severe knee pain, deformity, instability, or when nonsurgical treatments no longer help.
When to Go to the Emergency Room?
Go to the emergency room for high fever, sudden severe swelling, uncontrolled pain, or signs of infection after surgery.
What Recovery Really Looks Like?
Patients may begin walking with support shortly after surgery. Physical therapy focuses on strength, mobility, and stability. Progress improves over several weeks to months.
What Happens If You Ignore It?
Ignoring severe knee deformity or instability may lead to worsening pain, falls, and loss of mobility.
How to Prevent It?
Severe cases needing hinged implants are usually not preventable, but early treatment of knee injuries and arthritis may delay progression.
Nutrition and Bone or Joint Health
Healthy meals, good hydration, and balanced nutrition support healing and strength during recovery.
Activity and Lifestyle Modifications
Patients begin with protected walking and progress through guided therapy. Activities increase gradually as strength improves. Heavy strain should be avoided until cleared by the surgeon.
Do you have more questions?
How long does hinged knee replacement surgery typically take?
Hinged knee replacement surgery usually takes around two to three hours, depending on the complexity of the case and any additional procedures required.
What type of anesthesia is used for hinged knee replacement surgery?
Most hinged knee replacement surgeries are performed under general anesthesia, although regional anesthesia such as a spinal or epidural may also be used in some cases.
How soon after surgery can I expect to be able to walk?
Patients typically begin walking with the assistance of a physical therapist and a walker or crutches within the first day or two after surgery. Full weight-bearing may take several weeks to achieve.
Are there any dietary restrictions following hinged knee replacement surgery?
While there are no specific dietary restrictions, maintaining a balanced diet rich in nutrients can support the healing process and overall recovery.
What activities should I avoid after hinged knee replacement surgery?
Initially, you should avoid high-impact activities such as running or jumping. Your surgeon will provide guidance on gradually reintroducing activities based on your individual progress.
How long does it take to fully recover from hinged knee replacement surgery?
Recovery time can vary depending on factors such as age, overall health, and adherence to rehabilitation protocols. Most patients experience significant improvement within three to six months post-surgery, with continued gains over the following year.
Will I need physical therapy after hinged knee replacement surgery?
Yes, physical therapy is an essential component of recovery after hinged knee replacement surgery. It helps improve strength, flexibility, and function in the knee joint.
Can I drive after hinged knee replacement surgery?
You should avoid driving until you have regained sufficient strength, mobility, and reflexes, which typically takes about four to six weeks.
Will I need to use assistive devices like walkers or crutches after surgery?
Yes, you may need to use assistive devices such as walkers or crutches initially to support your weight and facilitate walking. Your physical therapist will guide you on their proper use.
How long will the implants used in hinged knee replacement surgery last?
The longevity of knee replacement implants varies depending on factors such as implant design, patient activity level, and overall health. However, modern implants are designed to last 15-20 years or more in many cases.
Can hinged knee replacement surgery be performed on both knees simultaneously?
In some cases, bilateral hinged knee replacement surgery may be considered, but it depends on factors such as the patient’s overall health and the complexity of the procedure. This decision is made on a case-by-case basis.
Will I be able to bend my knee normally after hinged knee replacement surgery?
Yes, the goal of hinged knee replacement surgery is to restore as much normal function and range of motion to the knee as possible. However, it may take time and diligent rehabilitation to achieve optimal flexibility.
What are the potential complications of hinged knee replacement surgery?
Complications can include infection, blood clots, implant wear or loosening, stiffness, and nerve or blood vessel injury. Your surgeon will discuss these risks with you before surgery.
How soon can I return to work after hinged knee replacement surgery?
The timing of your return to work depends on factors such as the physical demands of your job, your overall health, and the progress of your recovery. Desk-based jobs may allow for a quicker return, while physically demanding jobs may require more time off.
Will I need to take pain medication after hinged knee replacement surgery?
Pain medication is often prescribed following surgery to manage discomfort during the initial recovery period. Your surgeon will provide guidance on the appropriate use of pain medication.
Can I participate in sports or exercise after hinged knee replacement surgery?
While low-impact activities such as swimming, cycling, and walking are generally encouraged after hinged knee replacement surgery, high-impact sports or activities that involve twisting or pivoting may need to be avoided to protect the implant.
What can I do to prepare for hinged knee replacement surgery?
Preparing for hinged knee replacement surgery may include attending pre-operative appointments, completing any necessary tests or screenings, arranging for help at home during recovery, and following any pre-operative instructions provided by your surgeon.
How long will I need to stay in the hospital after hinged knee replacement surgery?
Hospital stays after hinged knee replacement surgery typically range from one to three days, depending on individual factors such as overall health and progress of recovery.
Will I need to wear a brace after hinged knee replacement surgery?
A brace may be prescribed for a short period after surgery to provide additional support and stability to the knee as it heals. Your surgeon will advise you on its use.
Are there any alternatives to hinged knee replacement surgery?
Depending on your specific condition, alternatives to hinged knee replacement surgery may include traditional knee replacement, partial knee replacement, or conservative treatments such as medication, physical therapy, and injections.
How often will I need to follow up with my surgeon after hinged knee replacement surgery?
Follow-up appointments with your surgeon are typically scheduled at regular intervals after surgery to monitor your progress, address any concerns, and assess the function of the knee implant.
Will I need to make any modifications to my home after hinged knee replacement surgery?
Depending on your mobility and accessibility needs, you may need to make temporary modifications to your home, such as installing handrails or raised toilet seats, to facilitate your recovery.
Can hinged knee replacement surgery be performed on older adults?
Age alone is not a determining factor for candidacy for hinged knee replacement surgery. As long as the patient is healthy enough to undergo surgery and has realistic expectations for the outcome, age is not a barrier to treatment.

Dr. Mo Athar
A seasoned orthopedic surgeon and foot and ankle specialist, Dr. Mohammad Athar welcomes patients at the offices of Complete Orthopedics in Queens / Long Island. Fellowship trained in both hip and knee reconstruction, Dr. Athar has extensive expertise in both total hip replacements and total knee replacements for arthritis of the hip and knee, respectively. As an orthopedic surgeon, he also performs surgery to treat meniscal tears, cartilage injuries, and fractures. He is certified for robotics assisted hip and knee replacements, and well versed in cutting-edge cartilage replacement techniques.
In addition, Dr. Athar is a fellowship-trained foot and ankle specialist, which has allowed him to accrue a vast experience in foot and ankle surgery, including ankle replacement, new cartilage replacement techniques, and minimally invasive foot surgery. In this role, he performs surgery to treat ankle arthritis, foot deformity, bunions, diabetic foot complications, toe deformity, and fractures of the lower extremities. Dr. Athar is adept at non-surgical treatment of musculoskeletal conditions in the upper and lower extremities such as braces, medication, orthotics, or injections to treat the above-mentioned conditions.
