Case Study: Custom Left Total
Knee Replacement in a 66-year-old male
A 66-year-old patient presented to our office for consultation regarding his left knee pain. He complained of worsening pain in the left knee for the past 1 year. He complains of associated difficulty in walking, twisting, going up and down the stairs, kneeling, and squatting. He initially experienced pain which was insidious in onset 6 years ago with periods of remittance and exacerbation.
Recently, he noticed the pain has become more constant limiting his daily activities. The patient is a veteran and feels injuries sustained during his stint in the army may have contributed to his knee pain getting worse with time. The patient was active earlier and rode his bicycle regularly. He had severely restricted his activities secondary to knee pain.
The patient is a nonsmoker with a medical history of benign prostate hypertrophy, dyslipidemia, and hypertension. He has no known drug allergies. Past surgical history includes an arthroscopic meniscal repair done ten years ago in Alabama. He was currently taking Flomax, Lopressor, and Lipitor.
His physical examination revealed a steady gait with a normal range of motion of both knees (left side end flexion was painful). There was mild effusion in the left knee with medial joint line and patellar facet tenderness. The patellar tap was negative but positive on milking the suprapatellar pouch. The bilateral hip and ankle were normal.
The patient previously had cortisone injections and viscous placement injected in the left knee. He also reported the use of heat pads and physical therapy. The patient reported only minimal relief with them. Recently, his brother underwent a total knee replacement surgery with good results, this led him to explore the options available for him.
Considering his lifestyle limiting knee pain, various management options including both surgical and nonsurgical were discussed with him at length. He was considered a candidate for custom left knee total replacement. Risks, benefits and potential complications were discussed with him in detail. He agreed to the plan. Imaging studies revealed severe tricompartmental osteoarthritis of the left knee joint.


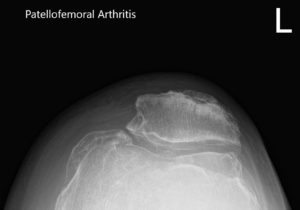
Preoperative X-ray of the left knee showing AP and lateral view of the knee with a skyline view of the patella.
A preoperative CT scan of the left knee with the hip and ankle was obtained 3 weeks prior to the surgery. The data were processed to obtain 3D images which were then used to construct unique custom implants. Additionally, unique 3D printed instruments were constructed to aid the surgeon in accurate bone cuts and accurate femoral offsets. A preoperative plan was prepared to preplan the surgical steps and bone cuts.
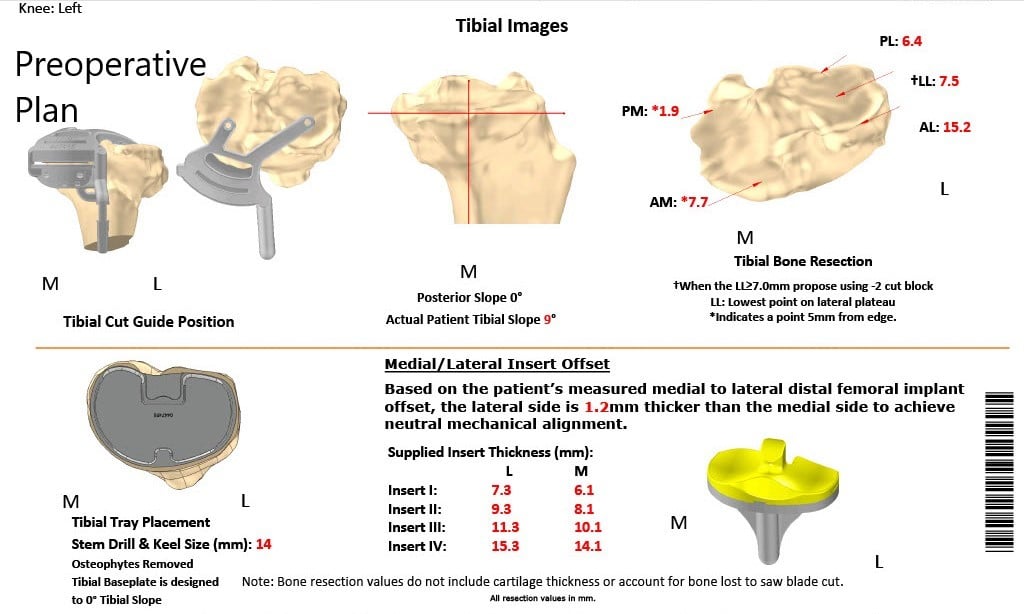
Complete Orthopedics patient specific surgical plan for a custom left total knee replacement in a 66-year-old male.
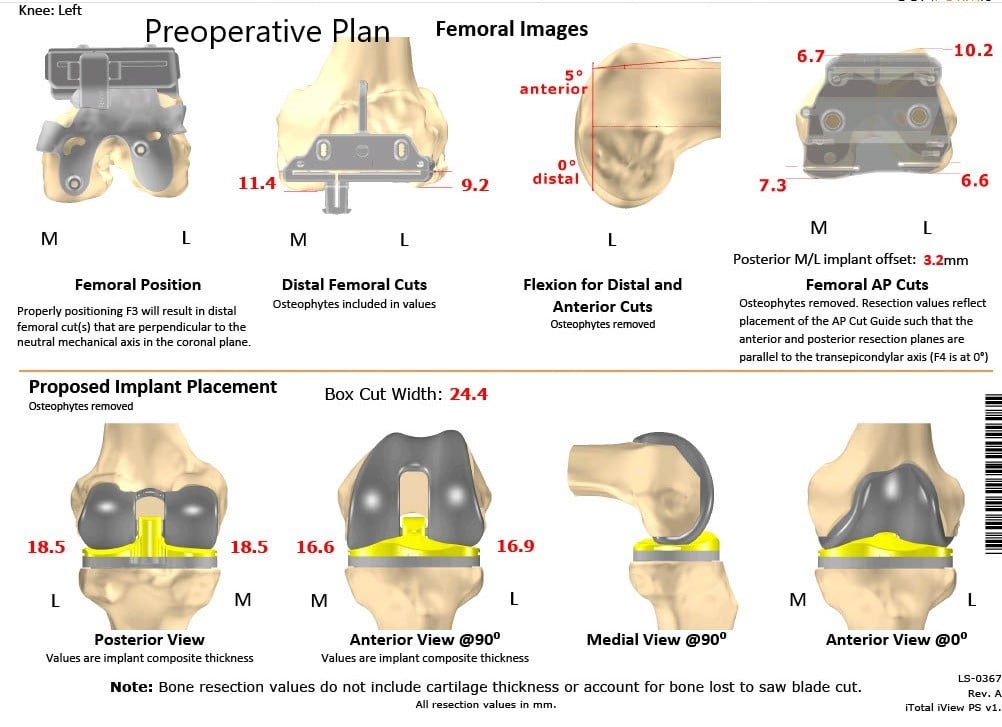
Complete Orthopedics patient specific surgical plan for a custom left total knee replacement in a 66-year-old male (scan 2)
The preoperative plan outlining the bone cuts and offsets.
Implants used: Custom femoral implant with 6 mm polyethylene insert with a custom tibial tray with a 38 mm patellar implant.
Procedure: The left knee was then draped and prepped in the usual sterile manner. Esmarch was used and the tourniquet was then elevated. A straight incision was used for the arthrotomy. Skin and subcutaneous tissues were incised.
Medial parapatellar arthrotomy was then performed. The knee was then exposed. There was significant tightness because of osteophytes. It was decided to do the patella first.

Attention was then turned towards the tibia. The tibial cut was then performed. Lamina spreaders were used medially and laterally and the remainder of the meniscus and the cruciates were then debrided. Posterior osteophytes were then removed. A gap balancing was performed.
A trial femur was placed in position followed by the trial tibia which was placed into position after preparation of the tibial surface. The trial poly was then placed into position.
The knee was then reduced and trialed through a full range of motion. Full-extension was obtained. Full reflection was obtained. Patellar tracking was excellent.
The trial components were then removed. A thorough lavage was given. The femur was then cemented into position. Excess cement was removed. Tibia was cemented into position. Excess cement was removed. The poly was then placed into the tibia.
The knee was then reduced. The knee was then held in full extension with a bump under the ankle. The patella was then cemented into position and held with a patellar clamp. Excess cement was removed. Thorough lavage was given.
Medial parapatellar arthrotomy vas closed with O Vicryl in Stratafix. Cutaneous tissues were closed with O Vicryl, subcuticular tissues were closed with O Vicryl. Skin was closed using staples and sterile dressing was then applied over the wound. The tourniquet was then let go and the patient was then transferred to the postoperative care unit in stable condition.


Postoperative X-ray showing AP and lateral images of the left knee.
The patient was able to walk bearing weight the same day with good control of pain with medications. He was given aspirin for DVT prophylaxis. The patient was advised to undergo physical therapy and a home exercise program. His wound healing was unremarkable.
Three months post the surgery he complained of no pain (0/10) and had a full range of motion of the left knee. The patient was enthusiastic about the outcome of the procedure and had recently started riding his bicycle again. He was able to walk, climb stairs and drive without experiencing pain.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
