Revision Total Knee Replacement Surgery
Revision total knee replacement surgery is performed when a previous knee replacement has worn out, become loose, failed, or developed a complication such as infection, fracture, or instability. This procedure removes the old implant and replaces it with a new one. Revision surgery is more complex than the first knee replacement and requires careful planning and specialized implants. The goal remains the same: to restore movement and reduce pain so patients can return to their daily activities.
How Common It Is and Who Gets It? (Epidemiology)
Revision total knee replacement is less common than a first-time knee replacement. A knee implant may last fifteen to twenty years or more, but younger patients, very active individuals, and people with certain medical conditions may need revision surgery sooner. Infection, loosening, and wear are leading reasons why patients undergo the procedure.

Why It Happens – Causes (Etiology and Pathophysiology)
Knee replacement failure can occur due to mechanical wear, infection, instability, fractures, or bone loss. Micromotion between the implant and bone may cause loosening. Wear particles from the plastic insert may trigger bone destruction called osteolysis. Infections can damage tissue and weaken the implant. Trauma or ligament problems may also cause failure.

Removed articulating cement spacer and reamers.
Both mechanical and biological factors play a role in the failure of the surgery. The primary knee replacement may fail over the years or due to sudden injury/infection.
- The infection of the artificial knee joint is one of the commonest causes of early failure. The metallic and plastic parts may serve as growth surfaces for infectious agents. The surfaces are inaccessible for the body’s immune system.
- Aseptic loosening is the most common cause of failure of components many years after the surgery. There is micromotion between the interface of bone cement, bone surface, and the metallic component which causes loosening of the parts.
- There may be a generation of wear particles due to micromotion. The body’s defense system tries to get rid of the wear and tear particles. But in the process, the cells may also destroy the normal bone and cause loosening of the implant known as osteolysis.
- Fractures of the bones in the region of the implant may require revision of the implant. The type of surgery depends upon the location of the fracture.
- Instability of the artificial joint may be due to inadequate fixation of the implants or improper positioning of the implants. There may be laxity of the ligaments on the inner or outer side of the knee causing instability.
- Hypersensitivity to the metal parts may require revision with patient-friendly implants.
- Scar tissue may form on the undersurface of the quadriceps tendon causing a clunk on straightening the knee.
- Certain patient factors play a role in implant failure. Young patients with an active lifestyle may require revision earlier than the older age groups. Obese patients and patients with a history of prior knee surgery have a greater risk of infection.
How the Body Part Normally Works? (Relevant Anatomy)
A healthy knee joint has smooth cartilage that allows the thigh bone, shin bone, and kneecap to glide easily. A knee replacement uses metal and plastic parts to recreate these surfaces. Over time, these components may loosen or wear out. The surrounding ligaments, muscles, and bone support the knee, and problems in these structures can affect implant stability.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of implant failure may include pain, swelling, stiffness, warmth, redness, fever, limp, or feelings of instability. Pain with weight-bearing is common in mechanical loosening. Fever and malaise may occur with infection. Some patients experience clunking or difficulty bending or straightening the knee.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a detailed history and examination. The doctor checks joint movement, strength, and stability. X-rays show loosening, alignment, and bone loss. Computed tomography scans help evaluate component position. Magnetic resonance imaging may show bone damage. A bone scan can detect infection or loosening. Joint aspiration and blood tests look for signs of infection.
Classification
Revision knee failures may be classified by cause—loosening, infection, instability, fracture, or component wear. Surgeries are also categorized as partial revision (only one part replaced) or full revision (multiple parts replaced). The degree of bone loss and ligament stability helps determine which implant type is used.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may resemble implant failure include tendon irritation, bursitis, spinal nerve issues, hip arthritis, or general inflammation around the joint. A thorough exam and imaging help confirm whether the problem comes from the implant itself.
Treatment Options
Non-Surgical Care
Some mild symptoms may be managed with medications, therapy, or bracing, but most implant failures require surgery.
Surgical Care
Revision knee surgery removes the old implant and replaces it with a new one. In infection, surgery may be done in one step or two steps. Two-step surgery removes the implant, washes the joint, and places an antibiotic spacer, followed by a second surgery weeks later. Special long-stem implants, cones, sleeves, and bone grafts may be used to correct bone loss or instability. The operation takes longer than a primary knee replacement.
The surgery is planned preoperatively according to the condition of the implant and the bone. The exposure and the surgery time is usually longer than the primary knee replacement surgery.
In the case of infection, the type of surgery depends upon the severity and time of onset of the infection. The surgery may be divided into two steps or done in a single step.

Revision knee replacement implant (semi – constrained with a long stem).
In a two-step approach, during the first surgery, the infected implants are removed. The joint is thoroughly washed and debrided. A prosthesis made of bone cement is inserted with antibiotics.
The patient is given intravenous antibiotics and after a period of a few weeks, definite fixation is undertaken. The joint aspiration is repeated before the definite surgery.
In the case of recent onset infection, the joint is washed thoroughly and only the plastic parts are replaced. In some cases, the infected prosthesis is removed and replaced with a new one in the same setting.
Periprosthetic fractures may require the use of special long stem implants. The type of surgery depends upon the level of the fracture.
In case of failure of the plastic component, only the plastic component may require revision. The revision surgery may require bone grafts or special cones to account for bone loss during the extraction.

Cementing of the femoral component.
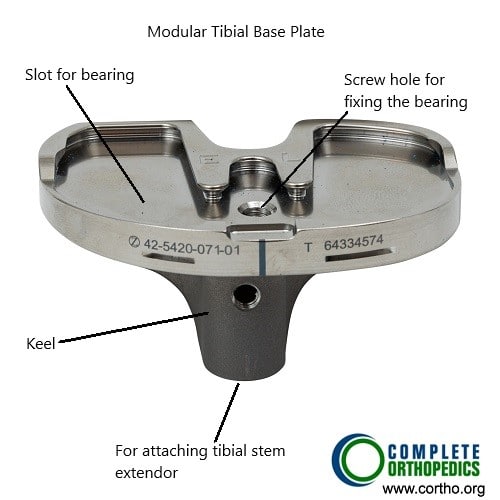
Modular Tibial Component
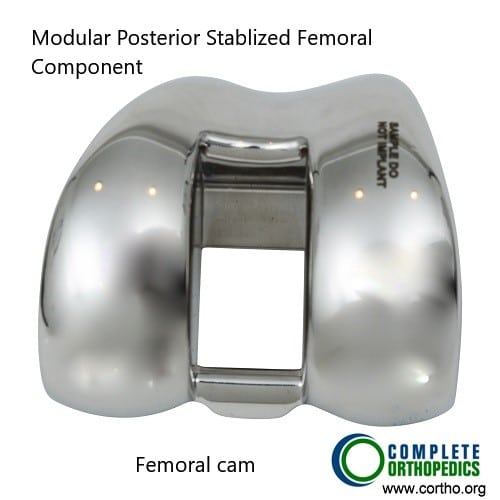
Modular femoral component
The above images show modular femoral and tibial components. The modular components allow the surgeon to make intraoperative adjustments to achieve greater stability. There are provisions to attach stems to the components as well as adding bone augments to account for bone loss encountered during surgery.
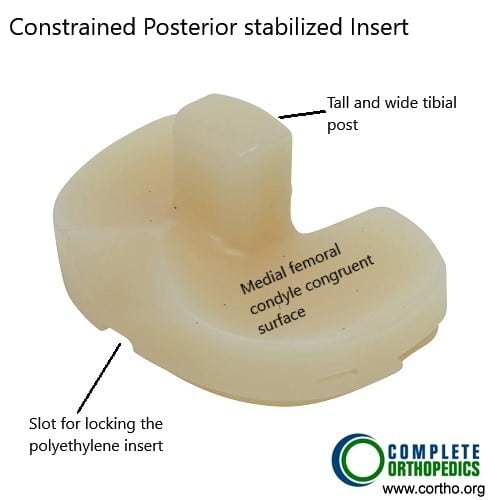
Constrained posterior stabilized polyethylene insert
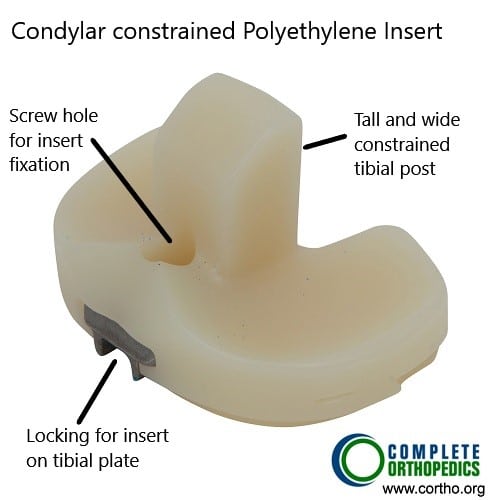
Condylar constrained Polyethylene insert
Constrained polyethylene inserts in the images above utilize a tall and wide tibial post to provide side to side and rotational stability. These inserts are usually used with femoral and tibial components with stems. The stems dissipate the additional stress arising from the constrained construct.
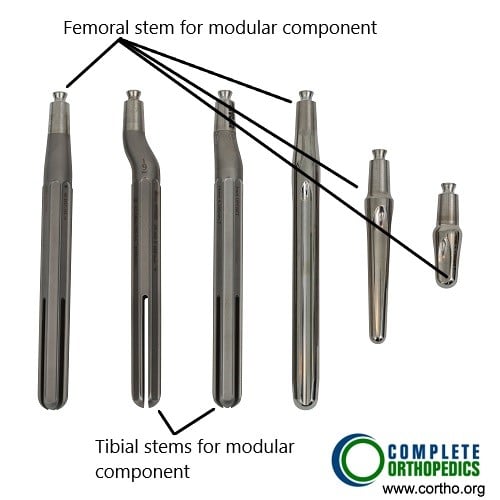
Tibial and femoral stems for modular knee components
A bone graft may be taken from the patient from a different location or may be taken from a bone bank. Metallic cones and metaphyseal sleeves may be used to compensate for bone loss. Specialized implants with a long stem or constrained tibial implants may be used to reduce instability and provide better fixation.
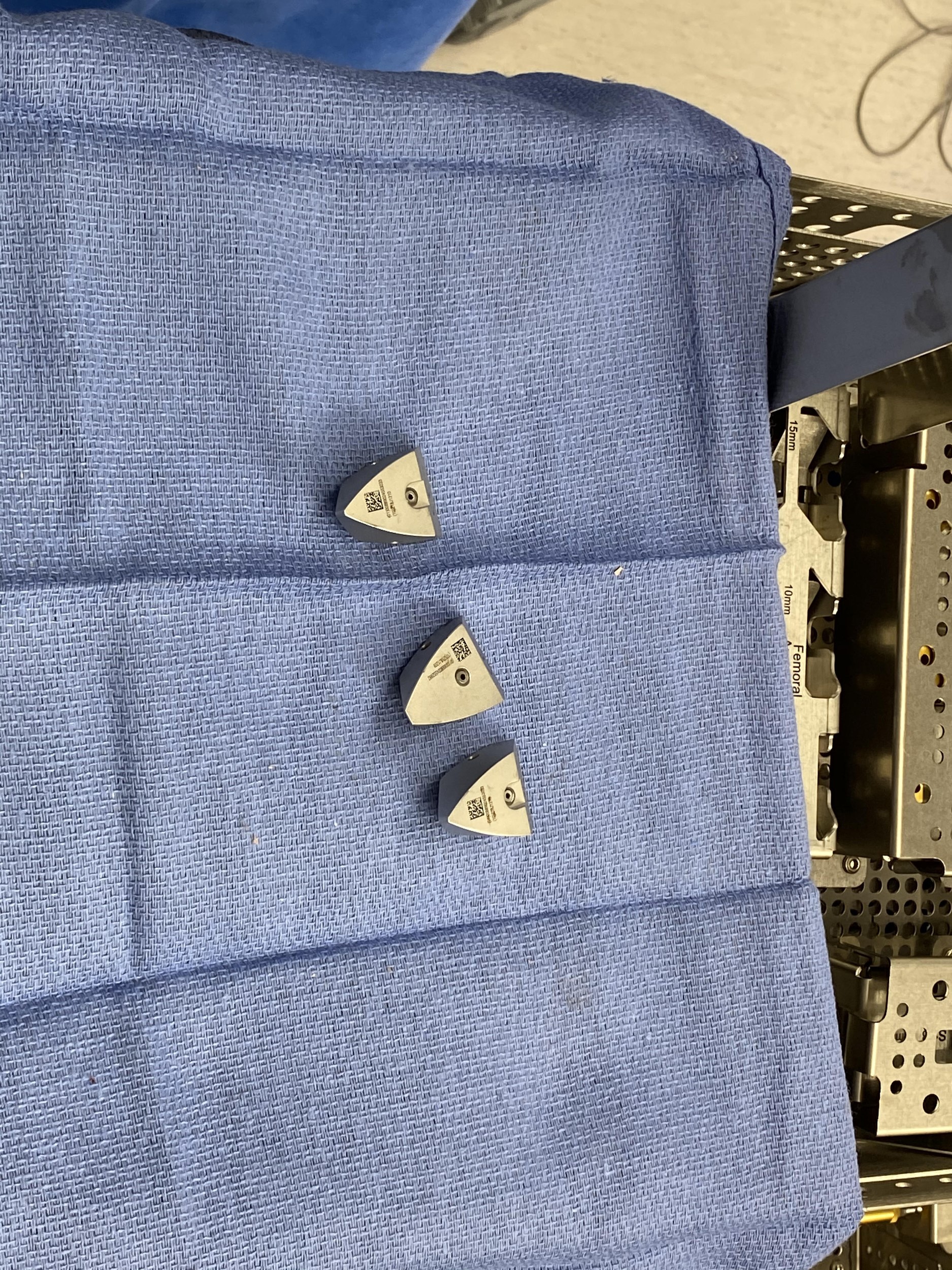
Metallic cones.

Metaphyseal sleeves.
Recovery and What to Expect After Treatment
Patients usually stay in the hospital for several days. Pain medicine and early physical therapy help restore movement. Therapy continues for several months. Home adjustments such as handrails and walkers help with safety. Follow-up visits check implant function. Full recovery may take up to a year. Patients are advised to stay active and maintain a healthy weight.
Possible Risks or Side Effects (Complications)
Risks include infection, blood clots, fractures, nerve injury, vessel injury, stiffness, and implant instability. Revision surgery has higher risks than first-time knee replacement. Early weeks carry a higher chance of infection or blood clots. Long-term risks include loosening, wear, and the need for further revision.
Advances in Revision Knee Surgery
Recent advancements have improved the outcomes of revision knee surgery:
Better Implants: Newer implants are designed to be more durable and to fit better, which can improve function and longevity.
Enhanced Techniques: Advances in surgical techniques have made the procedure more precise, reducing complications and improving recovery times.
Infection Control: Improved methods for preventing and treating infections have led to better outcomes.
Customized Implants: Some patients may benefit from customized implants designed specifically for their anatomy, which can improve the fit and function of the knee replacement.
Success
The vast majority of the revision knee replacements are done without any complications. A few may complain of residual knee pain, which can be managed with medications and physical therapy. With the increasing effectiveness of the implant materials and surgical techniques, revision surgeries are being done successfully.
Revision knee surgery can significantly improve the quality of life for many patients. However, the success rates vary based on several factors:
Patient Health: Overall health and comorbidities (other health conditions) can affect recovery and outcomes.
Reason for Revision: The underlying reason for the revision (e.g., infection, loosening) can influence the success rate.
Surgical Expertise: The experience and skill of the surgeon performing the revision are crucial for a successful outcome.
Long-Term Outlook (Prognosis)
Many patients benefit from revision knee surgery with improved comfort and mobility. Some may have mild ongoing pain that can be managed. Success depends on overall health, the reason for revision, and the skill of the surgical team. With modern implants and techniques, outcomes continue to improve.
Out-of-Pocket Cost
Medicare
CPT Code 27486 – Revision total knee replacement (single component): $332.04
Medicare covers most of the approved amount for this revision procedure, but it still leaves a portion for the patient to pay. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield usually cover the remaining twenty percent that Medicare does not pay. These supplemental plans are designed to close that gap, so patients commonly owe nothing further when the procedure is Medicare-approved.
If you also carry secondary insurance through an employer plan, TRICARE, or the Veterans Health Administration, it becomes the next payer after Medicare. After any deductible is met, the secondary plan may pay the rest of the balance, including coinsurance. Many of these policies have their own deductible, typically between $100 and $300 depending on the plan and network requirements.
Workers’ Compensation
If your revision total knee replacement surgery is needed because of a work-related injury, Workers’ Compensation will pay the full cost of the operation and all related care. You will not have any out-of-pocket costs.
No-Fault Insurance
If your knee condition is caused by a motor vehicle accident, No-Fault Insurance pays the entire cost of the revision surgery. You may only be responsible for a small deductible depending on your individual policy.
Example
A patient named Thomas required revision total knee replacement surgery to correct a failed implant. His estimated Medicare portion was $332.04. Because he also had secondary insurance, the remaining balance was fully covered, leaving him with no out-of-pocket expense.
Frequently Asked Questions (FAQ)
Q. Why would I need a revision knee replacement?
A. Common reasons include loosening, infection, wear, fracture, or instability.
Q. Is revision surgery more difficult than the first surgery?
A. Yes, it is more complex and requires special planning and implants.
Q. How long is recovery?
A. Recovery may take several months, and complete healing may take up to a year.
Q. Can infection be treated without surgery?
A. Deep infections usually require surgery and antibiotics.
Q. Will I walk after revision surgery?
A. Most patients walk with support soon after surgery.
Summary and Takeaway
Revision total knee replacement replaces a worn, loose, or infected knee implant. It is more complex than a first-time knee replacement and may require special implants, cones, sleeves, or bone grafts. Most people have improved comfort and function after surgery. The results depend on the cause of failure, overall health, and careful follow-up.
Clinical Insight & Recent Findings
A recent study followed more than 160 patients for two years after total knee replacement performed with a kinematic-alignment technique and found significant improvements in knee motion, muscle strength, walking ability, and patient-reported satisfaction, with no cases requiring revision surgery .
These findings highlight how modern alignment strategies can help preserve natural knee mechanics and may contribute to longer-lasting implants—an important consideration in revision knee replacement, where bone loss, instability, infection, or wear often necessitate complex reconstruction using stems, augments, cones, or constrained inserts.
The study’s demonstration of stable alignment and low complication rates supports the broader principle emphasized above: successful revision surgery relies on restoring functional alignment, addressing bone deficits, and providing durable fixation so patients can regain mobility after implant failure. (“Study on postoperative outcomes after knee replacement – see PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons with experience in complex knee reconstruction perform revision knee surgery. They work with anesthesiologists, nurses, physical therapists, and other specialists throughout the process.
When to See a Specialist?
You should see a specialist if you have worsening knee pain after a knee replacement, new swelling, redness, instability, difficulty walking, or signs of infection.
When to Go to the Emergency Room?
Seek emergency care if you experience sudden severe pain, inability to bear weight, fever with joint redness, or concern for infection or fracture.
What Recovery Really Looks Like?
Recovery includes a hospital stay, pain control, therapy, wound care, and gradual increase in movement. Swelling and stiffness are common early on. Over several months, strength and walking ability improve. It may take up to a year for full recovery.
What Happens If You Ignore It?
Ignoring implant failure can lead to worsening pain, bone loss, instability, fractures, and more complex surgery later. Infection can spread and become dangerous if untreated.
How to Prevent It?
Good joint care includes maintaining a healthy weight, avoiding falls, protecting the knee from injury, and seeking early treatment for infections. Regular checkups help detect problems early.
Nutrition and Bone or Joint Health
Healthy eating with enough protein, calcium, and vitamin D supports healing. Hydration and balanced meals help recovery and bone strength.
Activity and Lifestyle Modifications
Low-impact activities such as walking or cycling support joint health after revision. Avoiding heavy lifting, high-impact sports, or twisting motions helps protect the new implant and lower the chance of future failure.
Do you have more questions?
How long does a revision knee surgery take?
The duration of revision knee surgery can vary, but it generally takes between 2 to 3 hours, depending on the complexity of the case and the extent of the damage or complications with the initial implant.
What are the signs that my knee replacement is failing?
Signs of a failing knee replacement include persistent pain, swelling, instability, decreased range of motion, and sometimes noticeable changes in the alignment of the leg.
Can revision knee surgery be done on an outpatient basis?
Revision knee surgery is generally more complex and is usually performed in a hospital setting with an expected stay of a few days, unlike some primary knee replacements that can sometimes be done on an outpatient basis.
What type of implants are used in revision knee surgery?
Revision knee surgery often uses more robust and specialized implants designed to address the specific issues of the failed primary implant, sometimes including stems and augments for additional stability.
Will I need physical therapy after revision knee surgery?
Yes, physical therapy is crucial for recovery after revision knee surgery. It helps to restore strength, flexibility, and function to the knee.
How painful is revision knee surgery compared to the initial knee replacement?
Pain levels can vary, but many patients report that the pain after revision surgery is similar to or slightly more than the initial knee replacement due to the complexity of the procedure.
What are the success rates for revision knee surgery?
Success rates for revision knee surgery can vary but are generally around 85% to 90%, depending on the reason for the revision and the patient’s overall health.
How long will the new implant last after revision surgery?
While there is no guarantee, a well-performed revision knee surgery with proper implants can last 10-20 years, similar to primary knee replacements.
What lifestyle changes should I make after revision knee surgery?
Post-surgery, it’s important to maintain a healthy weight, stay active with low-impact exercises, and avoid activities that put excessive stress on the knee.
What should I do if I experience complications after revision knee surgery?
Contact your surgeon immediately if you experience signs of infection (fever, redness, or drainage), severe pain, or if you have difficulty moving the knee.
: How can I prepare my home for recovery after revision knee surgery?
Preparing your home for recovery includes installing handrails, keeping essential items within reach, and possibly arranging for a raised toilet seat or shower chair.
Will I need help at home after revision knee surgery?
Yes, it’s advisable to have someone assist you at home during the initial recovery period to help with daily activities and transportation to follow-up appointments.
How often will I need to see my surgeon after revision knee surgery?
Follow-up visits typically occur at two weeks, six weeks, three months, six months, and then annually to monitor the implant and overall recovery.
Can revision knee surgery address alignment issues from my first knee replacement?
Yes, one of the goals of revision surgery is to correct any alignment issues that may have occurred with the initial knee replacement.
What dietary changes should I make to aid my recovery after revision knee surgery?
A balanced diet rich in protein, vitamins, and minerals can help in healing. Staying hydrated and possibly taking supplements as recommended by your doctor can also aid recovery.
What are the long-term outcomes of revision knee surgery?
Long-term outcomes are generally positive, with most patients experiencing significant pain relief and improved function, though the recovery process can be longer and more challenging than the initial surgery.
Is it normal to feel numbness around the incision site after revision knee surgery?
Yes, some numbness around the incision site is normal due to nerve disruption during surgery, and it may persist for several months.
Are there any special exercises I should do before revision knee surgery?
Preoperative exercises focusing on strengthening the quadriceps, hamstrings, and maintaining range of motion can help improve postoperative recovery.
How can I prevent infections after revision knee surgery?
Preventing infections includes proper wound care, following your surgeon’s instructions for hygiene, and possibly taking antibiotics as prescribed.
What type of support will I need for mobility after revision knee surgery?
Initially, you will likely need crutches or a walker. As you progress in your recovery, you may transition to a cane before becoming fully independent.
How does bone quality affect the success of revision knee surgery?
Good bone quality is crucial for the success of the surgery as it affects the stability and longevity of the new implant. Bone grafts may be used if there is significant bone loss.
Can I drive after revision knee surgery?
You can usually start driving again once you have regained sufficient strength and mobility in your knee and are no longer taking narcotic pain medications, typically 4-6 weeks post-surgery. Always get your surgeon’s approval before resuming driving.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://www.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
