Understanding Your Joint Replacement Journey
We recognize the importance of understanding what to expect from your joint replacement journey. While you’re going through this material, feel free to reach out to us if you have any additional questions.

Unique Patient Experiences
Every patient’s experience with joint pain is unique. It’s essential to discuss the reasons behind your joint pain with us so that we can explore the treatment options available to you. Joint pain stemming from arthritis and degeneration can manifest in various ways: it may be persistent or intermittent, triggered by movement or rest, and localized or widespread across the body. Many patients initially try medication and other conservative treatments to manage their knee or hip pain. If you haven’t found relief with these options, you might be a candidate for Mako Total Knee, Total Hip, or Partial Knee replacement.
Mako’s Potential Benefits
Mako offers the potential for improved outcomes, such as reduced pain and shorter recovery times, compared to traditional manual joint replacement surgery.
Explaining Mako’s Functionality
Mako represents a cutting-edge solution for many individuals grappling with the agony of knee or hip arthritis.
Step One: Scan
It all begins with a CT scan, allowing your surgeon to gain deeper insights into your joint anatomy.
Step Two: Plan
Using the CT scan data, a 3D model of your joint is crafted. Your surgeon utilizes this model to develop a personalized surgical strategy, guiding them during your joint replacement procedure.
Step Three: Mako in Action
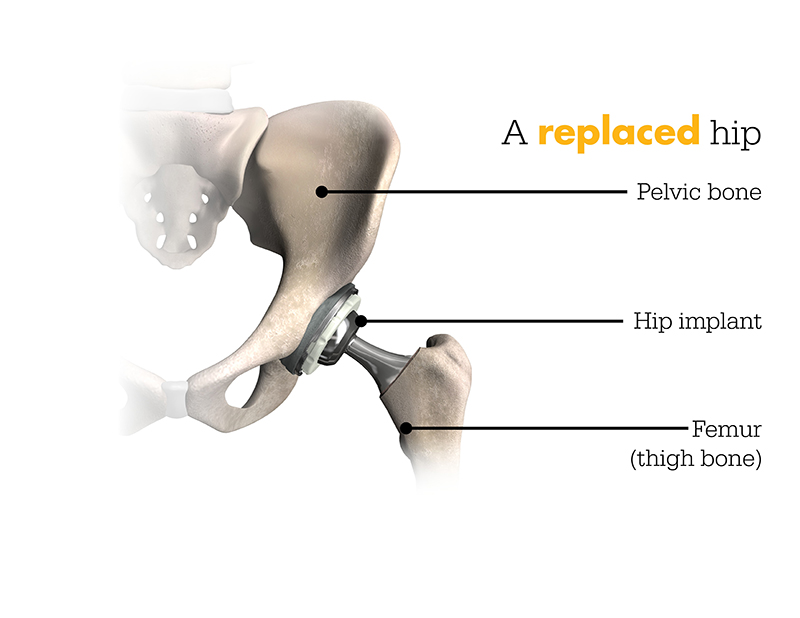
In the operating theater, your surgeon implements your tailored surgical plan, preparing the bone for implantation. Guiding Mako’s robotic arm within specified parameters, the surgeon benefits from Mako’s AccuStopTM technology, ensuring precise execution within the predetermined boundaries set during the preoperative planning phase.
Understanding Mako’s Role
It’s essential to understand that the surgery is conducted by an orthopedic surgeon who guides Mako’s robotic arm to position the implant in the knee and hip joints. Mako doesn’t independently perform surgery or make decisions; it operates under the surgeon’s guidance. Furthermore, Mako allows your surgeon to make real-time adjustments to the surgical plan as required.
Total knee vs. partial knee replacement
Assessing the degree of arthritis in the knee will determine whether a surgeon suggests total or partial knee replacement. In both cases, the orthopedic surgeon directs Mako’s robotic arm to extract damaged bone and cartilage.
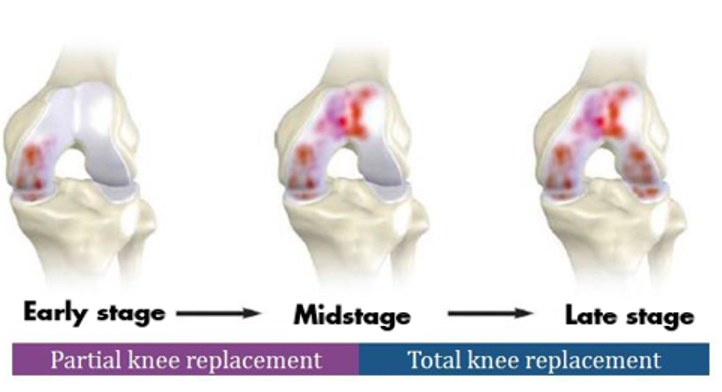
Mako Partial Knee replacement serves as a viable treatment choice for adults experiencing early to moderate stages of osteoarthritis (OA) that haven’t spread to all three knee compartments. Depending on the specific location of arthritis in the knee, patients may receive an implant in various areas, such as:
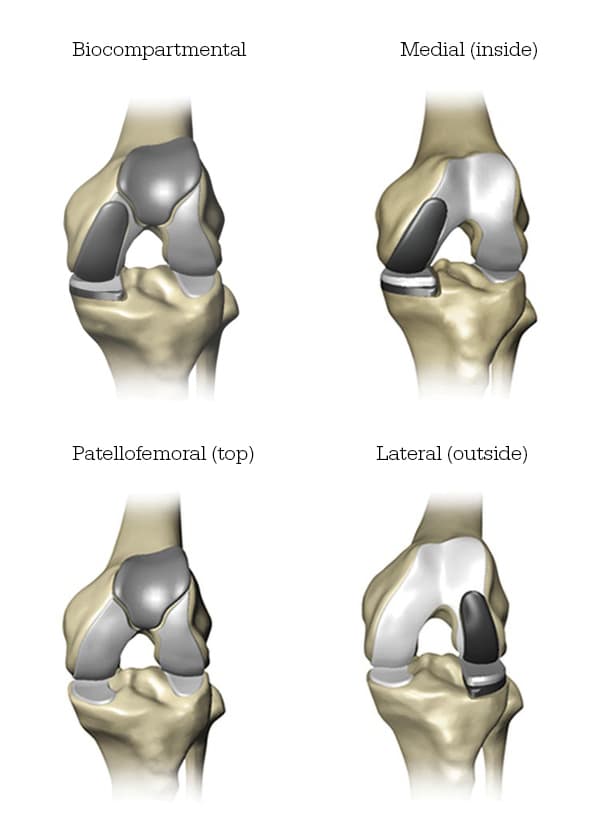
On the other hand, Mako for Total Knee replacement is a treatment possibility for adults dealing with moderate to advanced stages of knee osteoarthritis. During a Mako Total Knee replacement, the entire knee joint undergoes replacement, and the surgeon inserts a Triathlon Total Knee implant. Unlike conventional knee replacements, Triathlon knee replacements, with more than ten years of clinical experience, are engineered to collaborate with the body, promoting a natural circular motion.
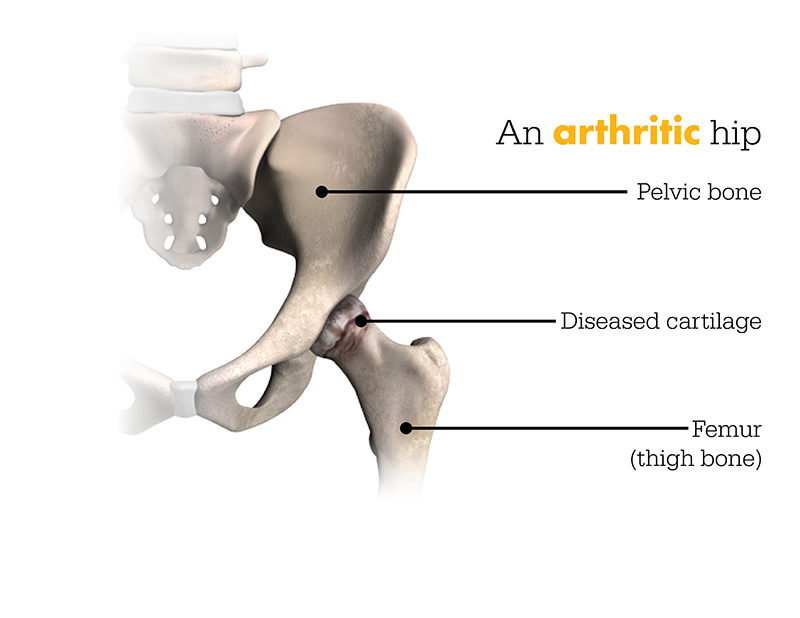
Similarly, Mako for Total Hip replacement is designed for patients grappling with noninflammatory or inflammatory degenerative joint diseases (DJD). Various forms of DJD include osteoarthritis (OA), post-traumatic arthritis, rheumatoid arthritis (RA), avascular necrosis (AVN), and hip dysplasia.
Vital Information Regarding Knee & Hip Replacements
Knee and hip replacement surgeries are intended for individuals suffering from joint diseases caused by degenerative and rheumatoid arthritis, avascular necrosis, femoral neck fractures, or hip functional deformities.
Knee joint replacement is aimed at individuals with joint diseases arising from degenerative, rheumatoid, and post-traumatic arthritis, as well as moderate knee deformities.
Certain conditions may make joint replacement surgery unsuitable for patients, including specific infections, mental or neuromuscular disorders posing risks of prosthesis instability, fixation failure, or postoperative complications, compromised bone strength, skeletal immaturity, severe joint instability, or excessive body weight.
Like any surgical procedure, joint replacement surgery entails serious risks, including pain, infection, bone fractures, leg length discrepancies, joint stiffness, fusion, amputation, nerve damage, circulatory issues, genitourinary, gastrointestinal, vascular, bronchopulmonary disorders, heart attack, and even death.
Implant-related risks that may necessitate implant revision include dislocation, loosening, fractures, nerve damage, abnormal bone growth, implant wear, metal sensitivity, tissue imbalance, localized bone loss, audible sounds during motion, reaction to debris or metal ions. It’s important to note that knee and hip implants may not replicate the same feel or performance as a healthy joint.
The provided information serves educational purposes only. Consult your doctor to determine if joint replacement surgery is suitable for you. Individual outcomes vary, and not all patients regain the same activity level post-surgery. The lifespan of any joint replacement depends on factors such as patient weight and activity level. Your doctor will advise strategies to potentially extend the device’s lifespan, including avoiding high-impact activities and maintaining a healthy weight. Following your doctor’s post-surgery instructions closely is essential. Discuss with your doctor if joint replacement is suitable for you.
Stryker Corporation or its affiliated entities own, use, or have applied for trademarks such as AccuStop, Mako, Stryker, Triathlon. All other trademarks belong to their respective owners.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
