Buckling after Total Knee Replacement
Total knee replacement (TKR) is a highly successful surgery aimed at alleviating pain and restoring function in the knee joint. However, some patients may experience knee instability, commonly referred to as “buckling,” after the procedure. This can lead to difficulties in walking, fear of falling, and a decreased quality of life. Understanding the causes, symptoms, and treatment options for buckling after TKR is essential for effective management and improved outcomes.
How Common It Is and Who Gets It? (Epidemiology)
While knee replacement surgery is generally very successful, buckling or instability after the procedure is a complication that can occur in a minority of patients. It is more commonly seen in individuals with certain risk factors, such as obesity, poor muscle strength, pre-existing deformities (e.g., bowlegs or knock knees), or those undergoing revision knee replacement surgery. Patients with underlying conditions like rheumatoid arthritis or connective tissue diseases may also be at higher risk for knee instability after TKR.
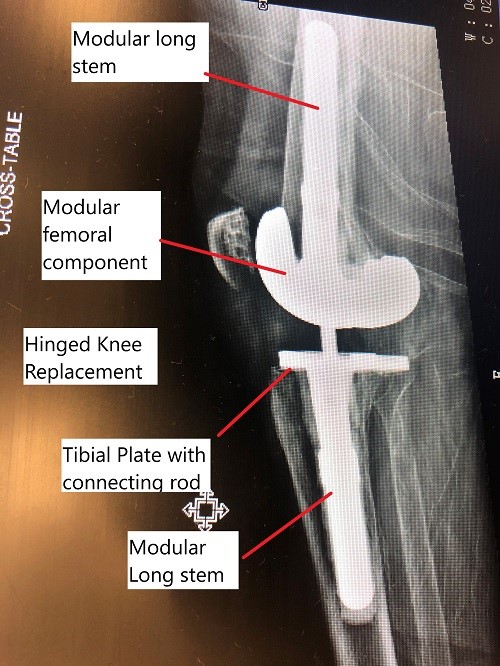
Intraoperative fluoroscopic image showing modular revision knee replacement.
What is Buckling After Total Knee Replacement?
Imagine you’re walking, and suddenly your knee gives out, causing you to stumble or fall. That’s what buckling feels like. Buckling after TKR refers to a sudden and unexpected loss of strength or stability in the knee joint, leading to a feeling of instability or giving way.
Why It Happens – Causes (Etiology and Pathophysiology)
The primary cause of buckling after TKR is instability in the knee joint, which can arise from several factors:
-
Weak Muscles: During surgery, muscles and tissues around the knee are disturbed, which can affect their strength and coordination.
-
Proprioception Loss: Proprioception refers to the body’s ability to sense the position of its joints. Changes in joint mechanics and nerve function after surgery can impair this ability, leading to instability.
-
Surgical Factors: Incorrect alignment, poor positioning of the implant, or excessive tissue release during surgery may lead to joint laxity and instability.
-
Infection, Implant Loosening, or Malposition: These complications can affect the stability of the knee, leading to buckling.
-
Pre-existing Deformities: Conditions like bowlegs or knock knees can place excessive strain on certain parts of the knee, contributing to instability after surgery.
How the Body Part Normally Works? (Relevant Anatomy)
The knee joint is a hinge joint formed by the femur (thigh bone), tibia (shin bone), and patella (kneecap). It is stabilized by ligaments, muscles, and tendons. The knee’s function is to allow smooth, controlled movement, and balance body weight during activities like walking, running, and jumping. After knee replacement surgery, the diseased parts of the knee are replaced with prosthetic components to restore function and alleviate pain.
What You Might Feel – Symptoms (Clinical Presentation)
Buckling after TKR presents as a sudden loss of knee stability, often resulting in a feeling that the knee is “giving way.” This may occur during physical activities or even at rest. Other symptoms include:
-
Knee Instability: A sensation of the knee buckling, giving way, or feeling weak during walking or standing.
-
Pain: Pain or discomfort in the knee joint, often associated with episodes of instability.
-
Swelling: Inflammation around the knee joint can exacerbate instability and cause discomfort.
-
Reduced Function: Difficulty performing activities that require weight-bearing or mobility, such as climbing stairs or walking long distances.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis is based on a thorough physical examination, patient history, and imaging studies. The physician will assess knee strength, alignment, and any visible signs of instability. Radiological studies such as X-rays, CT scans, or MRIs may be used to evaluate the alignment of the implants, detect loosening, and identify any structural issues such as bone damage or soft tissue problems.
Classification
Buckling after TKR can be classified based on the type of instability:
-
Varus-Valgus Instability: Side-to-side instability that may occur if the knee’s deformity is not fully corrected during surgery or if there’s excessive cutting of the femur.
-
Flexion Instability: Front-to-back instability resulting from over-resection of the femoral condyle or issues with the tibial implant’s slope.
-
Mid-Flexion Instability: Instability that occurs when bending the knee from 45 to 90 degrees, often due to malrotation or improper implant positioning.
-
Genu Recurvatum: Excessive knee hyperextension, often caused by contracture of the iliotibial band, leading to instability.
-
Global Instability: A combination of multiple types of instability, often resulting from severe bone loss or previous surgeries.
Other Problems That Can Feel Similar (Differential Diagnosis)
Several conditions can cause symptoms similar to buckling after TKR, including:
-
Implant Loosening: A common cause of instability after knee replacement.
-
Meniscal Tears: Damage to the menisci can cause instability or discomfort.
-
Ligament Injuries: Damage to other knee ligaments, such as the anterior cruciate ligament (ACL), can result in instability.
-
Osteoarthritis: Degenerative changes in the joint can cause pain and instability, particularly if the knee replacement has not fully addressed the underlying issues.

Intraoperative image of knee replacement surgery.
Treatment Options
Non-Surgical Care
-
Physical Therapy: Strengthening exercises targeting the muscles around the knee, especially the quadriceps, can help improve stability and reduce episodes of buckling.
-
Bracing: Knee braces or orthotics may provide additional support and help improve joint alignment during weight-bearing activities.
-
Medications: NSAIDs may be prescribed to manage pain and inflammation, although they are not a direct treatment for instability.
Surgical Care
In cases where conservative measures fail, surgical intervention may be necessary. Options include:
-
Revision Surgery: Revision TKR involves replacing or adjusting the existing prosthetic components. Special implants, such as hinged implants or those with rotating platforms, may be used to address instability.
-
Soft Tissue Repair: If instability is caused by damaged soft tissues, surgical repair or tightening of the ligaments and tendons may be performed.
-
Realignment: In some cases, the alignment of the knee or prosthetic implant may need to be adjusted to correct the instability.
Recovery and What to Expect After Treatment
Recovery from treatments for knee instability, particularly revision surgery, involves a structured rehabilitation program. This includes strengthening exercises, gait training, and range-of-motion activities. Full recovery may take several months, and the patient should gradually resume activities under the guidance of their healthcare provider.
Possible Risks or Side Effects (Complications)
-
Infection: A risk with any surgery, particularly revision surgeries.
-
Blood Clots: Patients may be at risk for deep vein thrombosis (DVT) after surgery.
-
Nerve Damage: Nerves around the knee may be injured during surgery.
-
Implant Failure: Despite revision surgery, there is a risk of the new implant failing or loosening again.
Long-Term Outlook (Prognosis)
The prognosis for patients experiencing buckling after TKR depends on the underlying cause of the instability. Many patients can experience significant improvement with appropriate treatment, including physical therapy and, if necessary, revision surgery. However, some individuals may require multiple interventions to fully address the instability.
Out-of-Pocket Costs
Medicare
CPT Code 27487 – Revision Total Knee Replacement (Femoral and Tibial Components): $413.16
CPT Code 27380 – Soft Tissue Repair (Ligament/Tendon Repair Around Knee): $148.14
CPT Code 27427 – Soft Tissue Imbrication/Capsular Plication: $168.63
CPT Code 27418 – Realignment (Proximal Tibial/Tibial Tubercle Osteotomy): $967.95
Under Medicare, 80% of the approved amount for these procedures is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, leaving most patients with little to no out-of-pocket expenses for Medicare-approved knee surgeries. These supplemental plans work directly with Medicare to provide full coverage for procedures like knee replacement, soft tissue repair, and realignment surgeries.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on the specific policy and network status.
Workers’ Compensation
If your knee surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your knee injury requiring surgery is the result of a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses, including revision knee replacement, soft tissue repair, and realignment procedures. The only possible out-of-pocket cost may be a small deductible depending on your individual policy terms.
Example
Tom, a 65-year-old patient with knee arthritis, required revision total knee replacement (CPT 27487) and also underwent soft tissue repair (CPT 27380). His estimated Medicare out-of-pocket costs were $413.16 for the knee replacement and $148.14 for the soft tissue repair. Since Tom had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for the surgeries.
Frequently Asked Questions (FAQ)
Q. What causes buckling after TKR?
A. Buckling is primarily caused by instability in the knee joint, which may result from muscle weakness, poor implant positioning, infection, or other surgical complications.
Q. How is buckling after TKR treated?
A. Treatment typically includes physical therapy, strengthening exercises, knee bracing, and, in some cases, revision surgery to replace or adjust the implants.
Q. Can buckling after TKR be prevented?
A. While it may not be entirely preventable, following rehabilitation protocols, maintaining a healthy weight, and avoiding high-impact activities can reduce the risk of buckling.
Summary and Takeaway
Buckling after total knee replacement is a concerning complication that can affect mobility and quality of life. Early recognition of the symptoms and appropriate treatment, such as physical therapy or revision surgery, is key to managing this condition. By working closely with healthcare providers, individuals can improve knee stability and regain confidence in their knee function.
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons specializing in knee surgery and revision surgery are responsible for diagnosing and treating buckling after TKR. Physical therapists play a key role in rehabilitation and improving knee strength and stability.
When to See a Specialist?
If you experience knee instability, buckling, or pain after TKR, it is important to consult your surgeon or healthcare provider for an evaluation and appropriate treatment.
When to Go to the Emergency Room?
Seek emergency care if you experience severe pain, swelling, or signs of infection (e.g., redness, warmth, fever) after surgery, or if you fall due to knee instability.
What Recovery Really Looks Like?
Recovery from buckling after TKR involves strengthening exercises, improving mobility, and potentially undergoing revision surgery. It can take several months to regain full function and stability.
What Happens If You Ignore It?
Ignoring knee instability can lead to further damage to the knee joint, increased pain, and difficulty with daily activities. Timely intervention is essential to prevent complications and improve long-term outcomes.
How to Prevent It?
Prevention involves following a prescribed rehabilitation program, avoiding premature return to high-impact activities, and maintaining good knee health to reduce the risk of buckling after TKR.
Nutrition and Bone or Joint Health
Maintaining a healthy diet rich in calcium and vitamin D supports bone health and can help optimize the outcomes of knee surgery.
Activity and Lifestyle Modifications
Engaging in low-impact activities, maintaining a healthy weight, and following proper techniques for movements can help protect the knee joint and reduce the risk of instability.
Do you have more questions?
How common is buckling after total knee replacement surgery?
Buckling after total knee replacement surgery can occur in a minority of patients, but the exact prevalence varies depending on factors such as patient characteristics, surgical technique, and post-operative rehabilitation.
Can buckling after total knee replacement be prevented?
While it’s not always possible to prevent buckling entirely, certain measures such as adherence to rehabilitation protocols, maintaining a healthy weight, and avoiding high-impact activities can help minimize the risk.
Are there specific risk factors that increase the likelihood of experiencing buckling after total knee replacement?
Yes, factors such as muscle weakness or imbalance, impaired proprioception, complications like infection or implant loosening, and improper surgical technique can increase the risk of buckling after total knee replacement.
How is buckling diagnosed?
Diagnosis of buckling after total knee replacement involves a comprehensive evaluation by a healthcare professional, which may include physical examination, imaging studies, and diagnostic injections to identify underlying causes of instability.
What are the typical symptoms of buckling after total knee replacement?
Symptoms of buckling after total knee replacement include sudden loss of strength or stability in the knee joint, leading to a feeling of instability or giving way during weight-bearing activities.
Can physical therapy help with buckling after total knee replacement?
Yes, physical therapy is often an integral part of treatment for buckling after total knee replacement. Strengthening exercises and gait training can help improve muscle strength and coordination, thereby reducing episodes of instability.
Are there any specific exercises that can help prevent or manage buckling after total knee replacement?
Yes, exercises focused on strengthening the muscles around the knee, improving balance and proprioception, and optimizing joint mechanics can be beneficial in preventing and managing buckling after total knee replacement.
What role do orthotic devices play in the treatment of buckling after total knee replacement?
Orthotic devices such as knee braces or custom orthotics may provide additional support and stability for individuals experiencing buckling after total knee replacement. These devices help offload stress from the knee joint and improve alignment during weight-bearing activities.
When is surgical intervention recommended for buckling after total knee replacement?
Surgical intervention may be recommended for persistent instability or underlying issues that contribute to buckling after total knee replacement. This may include revision TKR surgery to replace or adjust implants, repair damaged soft tissues, or realign the joint.
How long does it typically take to recover from revision TKR surgery for buckling?
Recovery from revision TKR surgery for buckling can vary depending on the extent of the procedure and individual patient factors. Generally, rehabilitation and recovery may take several months, with gradual improvement in symptoms and function over time.
What are the potential complications of revision TKR surgery for buckling?
Complications of revision TKR surgery for buckling may include infection, implant failure, persistent instability, stiffness, or nerve damage. However, these risks can be minimized with careful surgical planning and post-operative management.
Is there a risk of recurrence of buckling after successful treatment?
While recurrence of buckling after successful treatment is possible, it’s less common with appropriate rehabilitation and adherence to preventive measures. Close follow-up with healthcare providers can help monitor for any signs of recurrence and intervene as needed.
Are there any alternative treatments for buckling after total knee replacement?
In some cases, alternative treatments such as regenerative therapies or adjunctive procedures like nerve blocks may be considered for individuals who are not candidates for or prefer to avoid surgical intervention. However, the effectiveness of these treatments may vary, and consultation with a healthcare provider is recommended.
How can I manage fear of falling after experiencing buckling episodes?
Managing fear of falling after experiencing buckling episodes involves a combination of physical therapy to improve strength and balance, psychological support to address anxiety and apprehension, and environmental modifications to reduce fall risks at home and in the community.
Can buckling after total knee replacement affect my ability to return to work or participate in recreational activities?
Yes, buckling after total knee replacement can impact your ability to perform daily activities, work tasks, and recreational pursuits. However, with appropriate treatment and rehabilitation, many individuals can regain confidence and resume their desired level of activity.
Are there any long-term consequences of experiencing buckling after total knee replacement?
Long-term consequences of experiencing buckling after total knee replacement may include continued instability, joint damage, and reduced quality of life. However, early detection and intervention can help minimize these risks and improve outcomes.
How can I find a healthcare provider experienced in treating buckling after total knee replacement?
Finding a healthcare provider experienced in treating buckling after total knee replacement involves asking for referrals from your primary care physician, researching specialists in orthopedic surgery or sports medicine, and seeking recommendations from other patients who have undergone similar treatment.
Is there ongoing research into better treatments for buckling after total knee replacement?
Yes, ongoing research aims to identify better treatments for buckling after total knee replacement, including advances in surgical techniques, implant design, rehabilitation protocols, and adjunctive therapies. Participating in clinical trials or studies may offer opportunities to access innovative treatments and contribute to scientific knowledge in this field.
Can buckling after total knee replacement affect my overall quality of life?
Yes, buckling after total knee replacement can significantly impact your overall quality of life by limiting mobility, causing pain and discomfort, and affecting your ability to perform daily activities and participate in social or recreational pursuits. However, with appropriate treatment and support, many individuals can experience improvements in symptoms and regain function.
Are there any lifestyle modifications I can make to help manage buckling after total knee replacement?
Yes, lifestyle modifications such as maintaining a healthy weight, avoiding high-impact activities, using assistive devices as needed, and practicing fall prevention strategies can help manage buckling after total knee replacement and reduce the risk of further injury.
Can buckling after total knee replacement be a sign of implant failure?
Yes, buckling after total knee replacement can be a sign of implant failure, particularly if it occurs suddenly or is accompanied by other symptoms such as pain, swelling, or decreased range of motion. Prompt evaluation by a healthcare provider is important to identify and address any underlying issues.
How can I stay active and maintain fitness after experiencing buckling after total knee replacement?
Staying active and maintaining fitness after experiencing buckling after total knee replacement involves working closely with your healthcare team to develop a personalized exercise program that addresses your specific needs and limitations. This may include low-impact activities such as swimming, cycling, or strength training, as well as modifications to accommodate any residual symptoms or functional deficits.
Is there a support group or community for individuals who have experienced buckling after total knee replacement?
Yes, there are support groups and online communities where individuals who have experienced buckling after total knee replacement can connect with others facing similar challenges, share experiences, and provide mutual support and encouragement. These resources can be valuable for coping with the emotional and practical aspects of living with buckling and navigating the healthcare system.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://www.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
