Anterior cruciate ligament surgery is done to reconstruct a torn anterior cruciate ligament using graft tissue. The graft may come from the patient’s own body, called an autograft, or from a donor, called an allograft. Both types of grafts are used widely and have their own advantages and drawbacks. The goal of surgery is to restore knee stability and function after an anterior cruciate ligament injury.
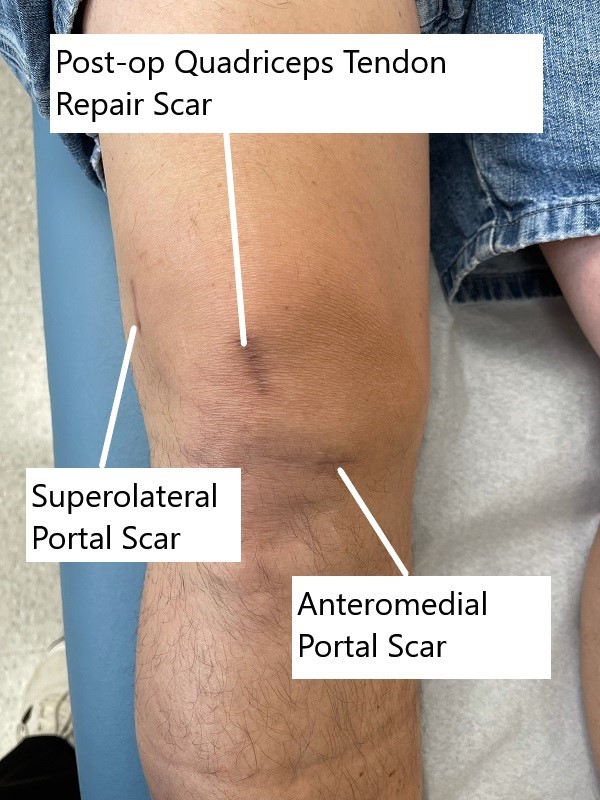
Postoperative images showing quadriceps tendon autograft scar and range of motion.
Postoperative images showing quadriceps tendon autograft scar and range of motion.
The choice of graft material depends upon the patient’s age, level of activity, availability, and the operating surgeon’s expertise. Both types of graft are highly successful and have been in use for the past many years. There are pros and cons associated with each type of graft. The patient is educated regarding the type of graft to be used for their surgery.
How Common It Is and Who Gets It? (Epidemiology)
Anterior cruciate ligament reconstruction is one of the most common orthopedic surgeries. Injuries often happen in athletes during sudden stops, twists, and jumps. Both younger and older patients may require reconstruction depending on symptoms and activity levels.
Why It Happens – Causes (Etiology and Pathophysiology)
Anterior cruciate ligament tears occur when the knee twists suddenly, absorbs a direct blow, or lands awkwardly. This stretching or tearing causes instability and may lead to degeneration of cartilage and early arthritis if left untreated.
How the Body Part Normally Works? (Relevant Anatomy)
The anterior cruciate ligament connects the thigh bone to the shin bone. It prevents the shin bone from sliding too far forward. It helps control stability when running, jumping, and pivoting. When torn, the knee moves abnormally and may feel unstable.
What You Might Feel – Symptoms (Clinical Presentation)
A torn anterior cruciate ligament can cause swelling, pain, and difficulty with knee motion. Many patients feel instability during walking or activity. Some injuries are accompanied by damage to the meniscus or other knee structures.
How Doctors Find the Problem? (Diagnosis and Imaging)
An MRI scan helps confirm an anterior cruciate ligament tear and shows whether the ligament is intact, partially torn, or fully torn. It also shows other structures such as the meniscus.
Classification
Anterior cruciate ligament injuries may be complete tears or partial tears. They may occur alone or with other injuries.
Other Problems That Can Feel Similar (Differential Diagnosis)
Symptoms may resemble meniscus tears, collateral ligament injuries, cartilage injuries, or bone bruises.
Treatment Options
Non-Surgical Care
Some older patients with early arthritic changes may be treated with a brace instead of surgery. Some torn anterior cruciate ligaments can scar and partially regain function, but this healing is unpredictable.
Surgical Care
Reconstruction replaces the torn ligament with a graft.
Autograft uses the patient’s own tissue such as the patellar tendon, hamstring tendon, quadriceps tendon, or peroneal tendon.
Allograft uses tendon tissue from a donor such as achilles, tibialis, hamstrings, or patellar tendon.
Surgery involves examining the knee with an arthroscope, treating associated injuries, creating bone tunnels, placing the graft, tensioning it, and securing it with devices such as screws or buttons.
Autograft ACL reconstruction
Autograft is harvested from the patient’s own body. The graft is a part of the patient’s body that has the same cellular and tissue makeup. Genetic compatibility ensures that the graft is not rejected by the body’s immune system.
Graft harvestation is the first step in autograft ACL reconstruction. The graft is commonly taken from the patellar tendon along with bone blocks from the patella and the tibia (Bone-Patellar-Tendon-Bone). The BPTB graft along with the bony ends helps in the biological incorporation of the graft. The bone ends naturally fuse with the femur and the tibia as they heal.
A hamstring graft is a soft tissue graft harvested utilizing the tendon of hamstring muscle on the inner aspect of the knee. The tendons are quadrupled to increase their strength. The quadrupled tendon has more strength than the natural ACL.
Other autografts that may be used for ACL reconstruction include the quadriceps tendon and the peroneal tendon. The soft tissue tendon grafts are usually secured in the tunnel for ACL using undo buttons, screws, etc.
While the autograft offers the advantage of being a part of the patient’s own body, it may have a few associated cons. The location of the graft site may not help and cause morbidity. Patellar tendon grafts have been associated with pain located in front of the knee. Similarly, hamstring autograft may cause inhibition of the hamstrings. The hamstrings are required to bend the knee and a tendon graft from the hamstring may cause knee weakness. Similar weakness in straightening the knee may result from quadriceps tendon graft.
Autografts:
Lower Risk of Rejection: Since autografts use tissue from your own body, there’s no risk of rejection by your immune system. Your body recognizes its own tissue and is less likely to mount an immune response against it.
Better Healing: Some studies suggest that autografts may provide better long-term stability and healing compared to allografts. Your own tissue might adapt more naturally to its new role in supporting your knee.
Reduced Risk of Disease Transmission: While rare, there’s always a slight risk of disease transmission with allografts since they come from a donor. Autografts eliminate this risk entirely.
Potential for Better Performance: Some athletes prefer autografts because they believe using their own tissue can lead to better performance on the field or court. It’s a psychological boost knowing that it’s your own body’s strength supporting you.

Bone tunnel plug used in ACL reconstruction.
Autograft harvesting also increases the operative time of the surgery. The autograft at times may not be of the required thickness and length to substitute the natural ACL. The autograft ACL reconstruction may also prolong the rehabilitation period.
Allograft ACL reconstruction
Allograft anterior cruciate ligament reconstruction involves the use of a graft harvested from a human cadaver. Allograft may be from a cadaveric achilles tendon, tibialis anterior/posterior tendon, hamstrings or patellar tendon.
The allograft is usually irradiated to kill any infectious agent such as bacteria/viruses. The allograft is readily available and comes in different sizes. The allograft shortened the operative time. The allograft also leads to early incorporation in the bone tunnel. Allograft ACL reconstruction also offers the benefit of no graft site morbidity. Participation in rehabilitation and general recovery is faster than autograft.
Allografts:
Less Painful: Since allograft surgery doesn’t involve harvesting tissue from your own body, you might experience less pain at the donor site. That means less discomfort during your recovery.
Quicker Recovery: Some studies suggest that patients who undergo allograft surgery may have a faster recovery time compared to those who opt for autografts. This could mean getting back to your normal activities sooner.
No Extra Incisions: With allografts, there’s no need for additional incisions to harvest tissue from your own body, which means fewer scars and potentially fewer complications.
Availability: Allografts are readily available, which means you don’t have to wait for your own tissue to heal before scheduling surgery.
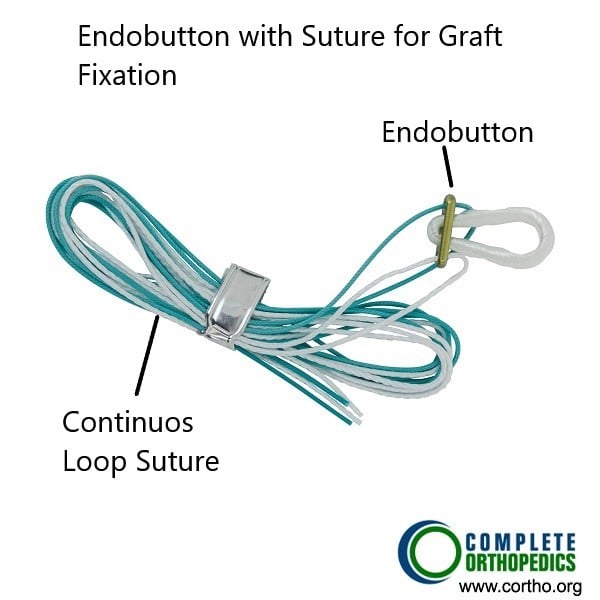
Endobutton used to secure the ACL graft.
Allografts however may present a challenge in younger age groups. Allografts in patients aged 30 or less have been associated with early graft failure. The failure may result from the rejection of the cadaveric graft tissue. The body’s immune system may reject the graft and the resulting inflammation may lead to graft failure.
The allograft ACL reconstruction is also considered to be less strong than the autograft reconstruction. The irradiation of the cadaveric graft to kill any infectious agent may also lead to biochemical changes in the structure of the graft that may weaken the integrity of the reconstruction. Although the irradiation kills any infectious agent, there might still be a possibility of transmission of a disease agent.
So, Which One Should You Choose?
Ultimately, the decision between allograft and autograft surgery depends on various factors, including your lifestyle, activity level, and personal preferences. Here are some questions to consider:
How important is a fast recovery to you? If you want to get back to your normal activities as quickly as possible, an allograft might be the way to go.
Are you concerned about the risk of rejection or disease transmission? If so, an autograft might offer peace of mind, knowing that you’re using your own tissue.
Do you prioritize long-term stability and performance? Some evidence suggests that autografts may provide better long-term outcomes, particularly for athletes or individuals with high activity levels.
Are you willing to undergo additional discomfort for the potential benefits of an autograft? Harvesting tissue for an autograft involves an additional surgical site and may result in some discomfort during recovery.
In the end, it’s essential to have a thorough discussion with your orthopedic surgeon to weigh the pros and cons of each option and determine which approach is best for you. Remember, everyone’s situation is unique, so what works for one person may not be the best choice for another.
Recovery and What to Expect After Treatment
Recovery includes managing pain, using crutches if needed, and attending physical therapy. Therapy restores motion, strength, and stability. Return to light activity may take a few weeks, while return to sports may take several months depending on healing and activity level.
Possible Risks or Side Effects (Complications)
Complications may include infection, bleeding, blood clots, graft failure, or re-tearing. Allografts may have a small risk of disease transmission. Autografts may cause discomfort or weakness at the harvest site.
Long-Term Outlook (Prognosis)
Most patients return to activity when rehabilitation is followed carefully. Autografts may give better long-term stability for young and active people. Allografts may offer faster early recovery but may have higher failure rates in patients under 30.
Out-of-Pocket Costs
Medicare
CPT Code 29888 – ACL Reconstruction: $229.85
Medicare generally pays most of the approved amount for this operation, leaving patients responsible for the standard twenty percent portion. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield typically remove that remaining co-insurance entirely. These plans work alongside Medicare and are intended to cover the amount Medicare does not pay, which often results in little or no cost to the patient when the procedure is Medicare-approved.
Secondary insurance plans such as employer-based policies, TRICARE, or the Veterans Health Administration become the next payer after Medicare. These plans may cover the remaining balance after their deductible is met. Deductibles in secondary plans usually fall between one hundred and three hundred dollars, depending on the policy. Once that requirement is met, the secondary plan often covers the leftover charges tied to the ACL reconstruction.
Workers’ Compensation
If your ACL injury occurred during work-related activity, Workers’ Compensation covers the entire cost of surgery, rehabilitation, and follow-up care. This leaves you with no out-of-pocket cost.
No-Fault Insurance
If the ACL injury resulted from a motor vehicle accident, No-Fault Insurance pays for the full procedure. The only potential cost to you would be a small deductible depending on your specific policy.
Example
A patient needed ACL reconstruction after a sudden twisting injury to the knee. With Medicare, the estimated out-of-pocket cost was 229.85 dollars. Because the patient also had a secondary insurance plan, that remaining twenty percent was covered completely, resulting in no out-of-pocket cost.
Frequently Asked Questions (FAQ)
Q. What is an autograft?
A. It uses tissue from your own body, such as hamstring, quadriceps, or patellar tendon.
Q. What is an allograft?
A. It uses tendon tissue from a donor.
Q. Which one heals better?
A. Some people prefer autografts because they use their own tissue. Allografts may heal faster early on.
Q. Which one hurts less after surgery?
A. Allografts avoid a harvest site, which may reduce early pain.
Q. Are allografts safe?
A. They are cleaned and irradiated, but there is still a small possibility of disease transmission.
Summary and Takeaway
Anterior cruciate ligament reconstruction can restore knee stability after injury. Autografts come from the patient’s own body and may provide durability. Allografts come from donors and may reduce early pain and shorten surgery time. The choice depends on age, activity level, and comfort with each option. A discussion with the surgeon helps determine the best approach.
Clinical Insight and Recent Findings
A recent study of tendon allografts used for anterior cruciate ligament revision showed strong improvements in stability and function, with International Knee Documentation Committee and Knee injury and Osteoarthritis Outcome Score values rising significantly and postoperative laxity averaging only about 1.5 millimeters.
These results align with your explanation of graft choices: autografts remain preferred for younger or high-demand patients because they integrate more reliably and avoid rejection, while allografts offer less pain, no donor-site morbidity, and shorter surgery time, making them practical in select or complex cases. (“Study of tendon allografts in anterior cruciate ligament revision – See PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons perform anterior cruciate ligament reconstruction. The care team may also include anesthesiologists, nurses, and physical therapists.
When to See a Specialist?
A specialist should be seen if the knee feels unstable after injury or if pain and swelling continue.
When to Go to the Emergency Room?
Emergency care is needed for severe swelling, uncontrolled pain, or signs of infection or blood clots.
What Recovery Really Looks Like?
Early recovery includes swelling reduction, pain control, and gentle motion. Therapy increases strength and stability over time. Activities return slowly, guided by the surgeon and therapist.
What Happens If You Ignore It?
Ignoring a torn anterior cruciate ligament may lead to instability and cartilage wear, which may cause early arthritis.
How to Prevent It?
Avoid sudden twisting movements, strengthen the leg muscles, and warm up before activities.
Nutrition and Bone or Joint Health
Balanced food choices support healing and improve overall joint recovery.
Activity and Lifestyle Modifications
Activity should increase in stages. Higher-demand activities take months, depending on graft type and rehabilitation progress.
Do you have more questions?
Is ACL surgery the only treatment option for a torn ACL?
While ACL surgery is a common treatment for a torn ACL, nonsurgical options such as physical therapy and bracing may be appropriate for some individuals, particularly those with minor injuries or who are not good candidates for surgery.
How do I know if I need ACL surgery?
The decision to undergo ACL surgery depends on various factors, including the severity of the injury, your symptoms, activity level, and overall health. Your orthopedic surgeon will evaluate your individual situation and recommend the most appropriate treatment option.
What are the different types of ACL surgery available?
There are several different surgical techniques for ACL reconstruction, including using autografts or allografts, as well as various fixation methods. Your surgeon will determine the most suitable approach based on your specific needs and circumstances.
What factors should I consider when choosing between an autograft and an allograft for ACL surgery?
Factors to consider when choosing between an autograft and an allograft for ACL surgery include recovery time, risk of complications, long-term outcomes, and personal preferences. Your surgeon can provide guidance based on your individual situation.
What type of anesthesia is used for ACL surgery?
ACL surgery is commonly performed under general anesthesia, which means you will be asleep and feel no pain during the procedure. In some cases, regional or local anesthesia may be used in addition to or instead of general anesthesia.
How soon after ACL surgery can I start walking?
You may be able to bear weight on your operated leg and start walking with crutches or a brace immediately after ACL surgery, depending on your surgeon’s instructions and the specific technique used.
How long will it take for me to regain full strength in my knee after ACL surgery?
Regaining full strength in your knee after ACL surgery can take several months of dedicated rehabilitation and exercise. Your physical therapist will work with you to gradually increase strength and function in your knee over time
Will I be able to kneel after ACL surgery?
Whether or not you’ll be able to kneel after ACL surgery depends on factors such as the specific technique used, your individual recovery, and any additional procedures that may have been performed. Your surgeon can provide guidance on when it’s safe to resume kneeling activities.
How can I prevent re-injury after ACL surgery?
Preventing re-injury after ACL surgery involves following your surgeon’s recommendations for rehabilitation, gradually returning to activities, and using proper techniques and protective equipment during sports and other physical activities.
What should I expect during the recovery process after ACL surgery?
The recovery process after ACL surgery typically involves a combination of rest, rehabilitation exercises, physical therapy, and gradual return to activities. Your surgeon will provide specific instructions and guidelines to help you navigate the recovery process successfully.
Can ACL surgery be performed on both knees at the same time?
While it is possible to perform ACL surgery on both knees at the same time, this approach may not be suitable for everyone. Your surgeon will evaluate your individual situation and recommend the most appropriate course of action.
Will I need to wear a compression sleeve after ACL surgery?
Whether or not you’ll need to wear a compression sleeve after ACL surgery depends on your surgeon’s recommendations and the specifics of your procedure. Some patients may benefit from wearing a compression sleeve to reduce swelling and provide support during the initial stages of recovery.
What are the potential complications of ACL surgery?
Complications of ACL surgery can include infection, blood clots, stiffness, nerve damage, and graft failure. However, serious complications are rare, especially when surgery is performed by an experienced surgeon and appropriate postoperative care is provided.
How can I prepare my home for recovery after ACL surgery?
Preparing your home for recovery after ACL surgery may involve making modifications such as clearing pathways, arranging furniture to minimize obstacles, and setting up a comfortable recovery area with pillows, blankets, and other essentials.
Will I need to undergo any tests before ACL surgery?
Before ACL surgery, you may undergo preoperative testing such as blood tests, imaging studies (such as X-rays or MRI scans), and a physical examination to assess your overall health and identify any potential risk factors or complications.
How long does ACL reconstruction surgery typically take?
ACL reconstruction surgery usually takes around 1 to 2 hours, depending on the complexity of the injury and the technique used.
Will I need to stay overnight in the hospital after ACL reconstruction surgery?
In most cases, ACL reconstruction surgery is performed on an outpatient basis, meaning you can go home the same day. However, some individuals may require overnight observation, particularly if there are concerns about pain management or other medical issues.
When can I expect to return to sports or physical activities after ACL reconstruction surgery?
The timeline for returning to sports or physical activities varies depending on factors such as the type of graft used, the extent of the injury, and your progress in rehabilitation. In general, most individuals can expect to return to sports within 6 to 12 months after surgery.
Will I be able to fully bend and straighten my knee after ACL reconstruction surgery?
Yes, restoring full range of motion in the knee is an essential goal of ACL reconstruction surgery. Physical therapy will focus on gradually increasing flexibility and strength in the knee joint.
Will I need to wear a knee brace after ACL reconstruction surgery?
Whether or not you need to wear a knee brace after ACL reconstruction surgery depends on factors such as the type of graft used, the extent of the injury, and your surgeon’s recommendations. In some cases, a knee brace may be recommended during sports or strenuous activities to provide additional support and stability.
Will I be able to drive after ACL reconstruction surgery?
You may be able to drive after ACL reconstruction surgery once you are no longer taking pain medications that impair your ability to drive safely and your knee is stable enough to operate the pedals without discomfort. It’s important to follow your surgeon’s guidance regarding driving restrictions.
How can I manage pain and discomfort after ACL reconstruction surgery?
Pain and discomfort after ACL reconstruction surgery can be managed with medications prescribed by your surgeon, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids. Additionally, applying ice to the knee and elevating it can help reduce swelling and discomfort.
Can ACL reconstruction surgery be performed if I have other medical conditions?
ACL reconstruction surgery can often be performed safely in individuals with other medical conditions, but it’s important to inform your surgeon about any preexisting health conditions or medications you’re taking. Your surgeon will assess the risks and benefits of surgery based on your overall health status.

