Natural History of Lumbar Spine Disease
If spine pain becomes so severe that it disrupts daily life or is accompanied by swelling, tenderness, or redness, it’s important to seek medical attention.
At Complete Orthopedics, our expert spine specialists are adept at treating spine pain through both surgical and non-surgical means. We examine symptoms, diagnose the condition, and recommend suitable treatments, including surgery if necessary.
Serving New York City and Long Island, we partner with six hospitals to offer cutting-edge spine surgery and comprehensive orthopedic care. You can schedule a consultation with our orthopedic surgeons online or by phone.
Learn about the common causes of spine pain and the treatment options available, including when surgery might be the best choice.
Overview
Six decades ago, a groundbreaking publication documented a successful surgical intervention for a condition referred to as a “ruptured disk.” Despite notable advancements in the field since then, many questions remain regarding the accurate diagnosis and effective treatment of low back pain and lumbar radiculopathy. Intriguingly, the discussions that ensued after the release of that publication continue to hold relevance in contemporary times. Modern diagnostic techniques, including magnetic resonance imaging (MRI), have supplanted antiquated approaches like lumbar puncture, myelography, and exploratory laminectomy. Furthermore, surgical procedures have undergone transformation, becoming less invasive and more precise, with a shift towards targeted interventions instead of the extensive bilateral, multilevel laminectomy that was once commonplace.
The Evolution of Diagnostic Techniques
The ongoing central concerns revolve around determining the necessity of a specific diagnosis for low back pain and radiculopathy, as well as deciding when surgery is the appropriate course of action. While in the past these questions were addressed on an individual patient level, they now require consideration on a broader population scale. It is essential to evaluate factors such as cost and clinical outcomes. However, the changing perceptions of pain and disability, evolving health expectations, and easy access to medical care pose challenges in interpreting previous research findings.
Clinical Outcome Studies
Even when clinical outcome studies rely on parameters like return to work, daily activity performance, or patient self-assessment of pain, their interpretation remains complex. It is worth noting that our understanding of pathoanatomic abnormalities in the common cold is even more limited, offering little consolation in comparison. The natural progression of lumbar spine disorders is perplexing. Placebo-controlled studies have shown that even inert injections can lead to substantial improvement in back pain and radiculopathy. Patients with signs of nerve compression and confirmed lesions were included, and conservative treatment had failed before entering the studies.
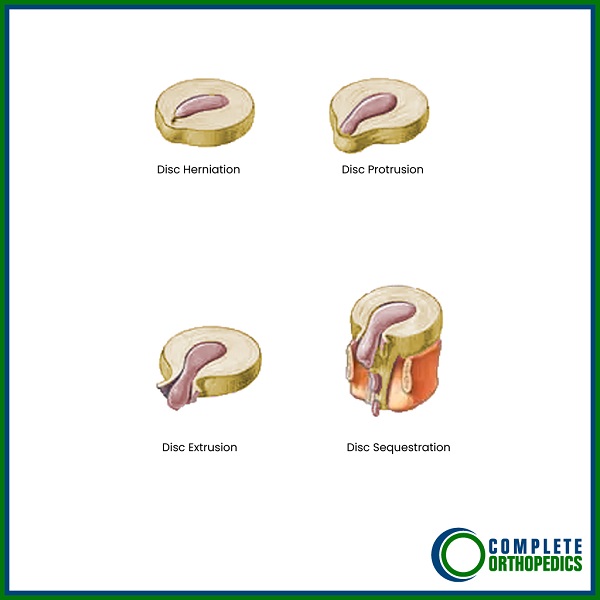
Disc Rupture Classification Illustrated
The Complexity of Lumbar Disk Disease
Understanding the progression of lumbar disk disease and its relationship to pain and disability is a complex matter. While a herniated disk is often linked to symptoms, degenerative spine disease can lead to abnormal imaging results without accompanying clinical manifestations. Differentiating between lesions that are likely to cause symptoms and incidental findings is of utmost importance when interpreting imaging data. In asymptomatic individuals, large compressive lesions are typically infrequent, but they are frequently observed in symptomatic patients who may require surgical intervention. Interestingly, these same sizable herniations, sequestrations, and extrusions demonstrate the highest rates of natural improvement when assessed through imaging studies.
Imaging Findings and Clinical Symptoms
The lack of consistent alignment between clinical symptoms and imaging findings suggests that the anatomical perspective alone is insufficient to fully comprehend the various aspects of lumbar spine disease. The existing literature presents an alternate perspective on herniated disks compared to the current understanding. It emphasizes the significance of larger lesions, often referred to as herniations, which were linked to severe motor impairments, sensory loss, or sphincter weakness in their patients. However, it is important to note that the correlation between the size of pathological specimens and imaging findings was not precise due to various contributing factors.
Variations in Lesion Descriptions
The descriptions of lesions, such as herniation, protrusion, or bulge, vary across studies and even within the works of the same authors. Changes in surgical techniques have also led to inconsistencies in surgical findings, which are often used as a reference standard in diagnostic accuracy studies. Modern imaging studies depict smaller lesions compared to earlier reports, highlighting the evolving understanding of these spinal abnormalities.
Criteria for Imaging
There is agreement among experts on certain criteria for imaging in patients with low back pain. Initially, imaging is recommended for individuals who suffer from significant pain-related disability, exhibit neurological findings, have a history of tumors, or require surgery or hospitalization. After an unsuccessful period of conservative treatment lasting 4-6 weeks, imaging can be considered for cases involving simple sciatica. However, there is no consensus regarding imaging for patients with stable back pain alone. It is widely accepted, albeit without robust scientific evidence, that MRI is the preferred imaging modality for such cases. However, it has not been convincingly demonstrated that the additional cost of MRI compared to computed tomography (CT) is justified on a large scale.
Debates and Considerations
Debate continues surrounding different aspects of lumbar spine disorders. The majority of individuals with acute conditions typically resume work within a few weeks, regardless of the treatment they receive. However, prolonged disability can have lasting effects. Timely diagnosis and treatment are crucial for individuals at risk of enduring disabilities. A comprehensive study is necessary to identify the particular symptoms, signs, and occupational groups where the expense of imaging can be justified by improved outcomes.
Long-Term Conservative Management
Existing literature has presented studies highlighting the potential of long-term conservative management trials coupled with systematic longitudinal imaging evaluation. However, the available data is restricted and inconclusive, albeit revealing interesting trends. These studies underscore the significance of refraining from prematurely dismissing established approaches to lumbar spine disease solely based on new data. A cautious analysis within the framework of Bayesian analysis is vital before implementing substantial changes in medical practice.
MR Imaging Reliability
Despite its limitations in detecting significant lumbar disk disease, MR imaging is still considered more reliable than alternative clinical evaluations and pain scales. The straight leg raising test, for instance, has demonstrated suboptimal sensitivity and specificity in identifying disk herniation. A more extensive study would be necessary to establish a definitive correlation between the level of neurologic disability and the abnormalities observed on MR images.
Patterns of Clinical Improvement
The data indicate distinct patterns of clinical improvement and persistent pain in patients with specific conditions. The study authors approach the hypothesis that imaging findings determine the treatment for lumbar radiculopathy with caution, refraining from refuting it outright. Further data is required concerning the individuals who remained in the study and those who discontinued participation. Lumbar spine disease encompasses intricate interconnections involving both physical and psychosocial elements. The correlation between lumbar spine-related disability and income exhibits an N-shaped curve, while the association between disability and education varies across genders. The influence of litigation and compensation on the clinical outcomes of patients with lumbar spine disease is firmly established.
Future Directions
Moving ahead, there are several critical actions to be taken. Firstly, it is of utmost importance to develop a nomenclature system that is universally accepted, easily reproducible, and applicable to lumbar spine findings observed in MR imaging. Secondly, there is a need for consensus on the relevant parameters for assessing outcomes and the establishment of standardized methods for their evaluation. Given the existing lack of agreement among physicians, patients, and the general public, it is advisable to explore a wide range of outcome measures to ensure a comprehensive assessment.
Research and Education
To increase the credibility of results, it is advised to replicate studies reported in the literature with a larger sample size and a multi-center, multi-specialty approach to minimize any biases stemming from local practices. Determining the optimal surgery rate and addressing ethical concerns are challenging aspects, and it requires extensive education efforts to secure cooperation from both patients and physicians. Studies reported by literature have demonstrated the feasibility of the approaches discussed. It is our anticipation that a trial similar to the one they propose will be conducted in the near future. We hold a strong belief that this trial will provide confirmation regarding the efficacy of imaging in the treatment of specific patients with lumbar spine disorders.
Conclusion
The understanding and treatment of lumbar spine disorders have significantly evolved over the past six decades. Modern diagnostic and surgical techniques offer improved precision and less invasiveness. However, the complexity of lumbar disk disease, the variability in imaging findings, and the interplay of physical and psychosocial factors necessitate a nuanced approach to diagnosis and treatment. Continued research, standardization of nomenclature and outcomes assessment, and education of both patients and healthcare providers are essential for advancing the management of lumbar spine disorders.
Do you have more questions?
How has the treatment of lumbar disk disorders evolved over the past six decades?
Treatment has shifted from extensive surgeries like bilateral, multilevel laminectomies to less invasive, more targeted procedures. Diagnostic techniques have also advanced, with MRI replacing older methods like myelography and lumbar puncture.
What is a ruptured disk?
A ruptured disk, also known as a herniated or slipped disk, occurs when the soft inner gel of the disk leaks out through a tear in the outer layer. This can compress nearby nerves, causing pain, numbness, or weakness.
Why is MRI preferred over older diagnostic techniques like myelography and lumbar puncture?
MRI is non-invasive, does not use ionizing radiation, and provides detailed images of both bone and soft tissues, making it more effective for diagnosing disk abnormalities and nerve compression.
What are the main symptoms of lumbar radiculopathy?
Symptoms include sharp pain radiating from the lower back to the legs, numbness or tingling in the legs or feet, muscle weakness, and sometimes difficulty with bladder or bowel control.
What are the risks and benefits of minimally invasive surgery for lumbar disk disorders?
Benefits include smaller incisions, less tissue damage, reduced pain, and faster recovery. Risks can include infection, nerve injury, and recurrence of the disk problem.
How can one differentiate between a herniated disk and degenerative spine disease on imaging?
A herniated disk typically shows a localized protrusion of disk material compressing the nerve roots, while degenerative spine disease may show widespread changes like disk space narrowing, bone spurs, and reduced disk height without nerve compression.
How do modern surgical techniques for lumbar disk disorders differ from older techniques?
Modern techniques focus on minimal tissue disruption, use of endoscopic methods, and precise targeting of the affected area, while older techniques involved larger incisions and more extensive tissue removal.
How effective are conservative treatments for lumbar disk disorders?
Conservative treatments like physical therapy, medications, and epidural injections can be effective for many patients, helping to reduce pain and improve function without the need for surgery.
What factors determine whether a patient needs surgery for a lumbar disk disorder?
Factors include the severity and duration of symptoms, failure of conservative treatments, significant nerve compression causing weakness or numbness, and the patient’s overall health and preferences.
What are the most common symptoms of lumbar disk herniation?
Common symptoms include lower back pain, radiating leg pain (sciatica), numbness or tingling in the leg or foot, and muscle weakness.
How reliable are MRIs in diagnosing lumbar disk disorders?
MRIs are highly reliable for detecting disk herniations, nerve compression, and other spinal abnormalities, but they must be correlated with clinical symptoms for an accurate diagnosis.
How can one manage lumbar radiculopathy symptoms without surgery?
Non-surgical management includes physical therapy, pain medications, anti-inflammatory drugs, epidural steroid injections, and lifestyle modifications such as weight management and ergonomic adjustments.
What role do psychological factors play in lumbar spine disease?
Psychological factors like stress, anxiety, and depression can exacerbate pain perception and disability, making a comprehensive treatment approach that includes psychological support important.
Why is it challenging to interpret clinical outcome studies for lumbar disk disorders?
Outcome studies can be complicated by variations in patient populations, treatment protocols, and the subjective nature of pain and disability assessments.
How important is early diagnosis and treatment for preventing long-term disability from lumbar disk disorders?
Early diagnosis and appropriate treatment are crucial for preventing chronic pain and long-term disability, as timely intervention can alleviate symptoms and improve function.
What are the current best practices for imaging patients with low back pain?
Imaging is recommended for patients with significant pain-related disability, neurological findings, or a history of tumors. After 4-6 weeks of unsuccessful conservative treatment, imaging can be considered for cases involving simple sciatica.
How does lumbar spine-related disability correlate with income and education?
There is an N-shaped curve relationship with income, where both low and high-income individuals may experience higher disability rates, while the correlation with education varies by gender.
What are the potential complications of lumbar disk surgery?
Complications can include infection, bleeding, nerve damage, recurrent disk herniation, and persistent pain.
How do changes in surgical techniques affect the findings and outcomes of lumbar disk surgeries?
Advances in surgical techniques have led to less tissue disruption, quicker recovery times, and improved precision, which can enhance outcomes and reduce complications.
Why is there a need for a universally accepted nomenclature system for lumbar spine findings?
A standardized nomenclature system would ensure consistency in diagnosis, treatment planning, and research, reducing confusion and improving patient care.
What are the key outcome measures for assessing the effectiveness of lumbar disk treatments?
Key measures include pain relief, functional improvement, return to work, patient satisfaction, and reduction in disability.
How can patient and physician education improve the management of lumbar spine disorders?
Education can enhance understanding of treatment options, set realistic expectations, improve adherence to conservative treatments, and ensure informed decision-making.
What future research is needed to improve the treatment of lumbar disk disorders?
Future research should focus on long-term outcomes of conservative vs. surgical treatments, the role of psychological factors, the effectiveness of new surgical techniques, and the development of personalized treatment plans.
How do litigation and compensation issues influence clinical outcomes in lumbar spine disease patients?
Litigation and compensation issues can complicate clinical outcomes by introducing external motivations and stressors, which may affect the patient’s perception of pain and disability and their response to treatment.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.