New York State Medical Treatment Guidelines for Shoulder
Impingement Syndrome in workers compensation patients
The New York State workers compensation board has developed these guidelines to help physicians, podiatrists, and other healthcare professionals provide appropriate treatment for Charcot Joint.
These Workers Compensation Board guidelines are intended to assist healthcare professionals in making decisions regarding the appropriate level of care for their patients with ankle and foot disorders. The guidelines are not a substitute for clinical judgement or professional experience. The ultimate decision regarding care must be made by the patient in consultation with his or her healthcare provider.
Impingement Syndrome of Shoulder Injury
A grouping of symptoms rather than a pathological diagnosis. The acromion, coracoacromial ligament, coracoid process, and/or the AC joint encroach on the rotator cuff mechanism as the shoulder moves, which causes the symptoms.
The coracoacromial arch is closely related to the cuff mechanism. Compression and friction, which are only separated by the bursar’s tiny lubricating surfaces, can be reduced in a number of ways, including:
- The coracoacromial arch’s shape, which permits the adjacent rotator cuff to pass;
- Normal AC joint undersurface;
- Normal bursa;
- Normal capsular laxity; and
- Coordinated scapulothoracic function.
Adhesive capsulitis/frozen shoulder, partial- and full-thickness rotator cuff tears, AC joint arthritis, and the impingement syndrome are all possible concomitants. The rotator cuff mechanism and biceps tendon should both be functioning normally to lessen impingement syndrome.
History and Mechanism of Injury of Impingement Syndrome
Mechanism of Injury: Overuse of the upper extremity due to established repetitive behaviour; this is typically seen with repetitive overhead action.
History may include:
- Delayed presentation: Since the syndrome is typically not an urgent issue, individuals will seek medical attention if their symptoms do not go away after resting, giving it some time, and “trying to work it out”;
- Complaints of functional impairment brought on by discomfort, stiffness, weakness, and catching when the arm is flexed and internally rotated; and
- Poor sleep is typical, and pain is frequently felt along the anterior proximal humerus or down the lateral aspect of the upper arm, close to the deltoid insertion.
Physical Findings of Injury of Impingement Syndrome
Physical Findings may include:
- Deltoid and rotator cuff atrophy may be found during a shoulder examination;
- Range of motion is constrained, especially in cross-body adduction and internal rotation;
- Pain and crepitus may accompany passive motion over the 60 to 90 degree arc of flexion; this is intensified as the shoulder is moved into and out of internal rotation;
- In general, active shoulder elevation causes more discomfort than passive elevation;
- Impingement syndrome typically manifests as pain on maximum active forward flexion, however this pain is not diagnostic;
- Testing your strengths could uncover weaknesses. This weakness could be brought by by discomfort, inactivity, tendon damage, or improper scapulothoracic mechanics;
- A weakening of the posterior scapular stabilisers may also be considered as a contributing factor to impingement syndrome by affecting the mechanics of the glenohumeral joint. Pain during resisted external rotation or abduction may also signal that the rotator cuff tendons may be weakened.
Laboratory Tests of Injury of Impingement Syndrome
Laboratory Tests of Injury of Impingement Syndrome is recommended – When a systemic illness or disease is suspected in a subset of patients.
Testing Procedures of Impingement Syndrome X-Ray
Testing Procedures of Impingement Syndrome X-Ray is recommended – Clinically appropriate in a subset of patients.
Indications: Calcification of bone spurs may be visible.
Subacromial Space Injection of Impingement Syndrome
Subacromial Space Injection of Impingement Syndrome is recommended- Clinically appropriate in a subset of patients.
Indications: injecting anaesthetic can be used as a diagnostic procedure, xylocaine or sensorcaine solutions, for example, into the area. If the discomfort is The injection provides relief, and the diagnosis is verified.
Non-Operative Treatment Procedures may include:
- Medicines like analgesics and nonsteroidal anti-inflammatory drugs
Subacromial Space Injection of Impingement Syndrome
Subacromial Space Injection of Impingement Syndrome is recommended clinically appropriate in a subset of patients.
Indications: If the patient responded favourably to an anaesthetic injection given for diagnostic purposes, a subacromial area injection of steroids might be therapeutic. Direct steroid injections into the tendons are not advised.
Frequency: Not more often than twice or three times per year. One or two injections are typically sufficient. It is advised to wait at least three weeks between injections.
Local anaesthetics take immediate impact, but corticosteroids take three days to start working.
Maximum duration: Three injections to the same place each year are permitted.
Considerations should be given to relative rest, immobilisation, thermal treatment, ultrasound, therapeutic exercise, physical medicine, and rehabilitation.
Operative Procedures of Subacromial Space Injection
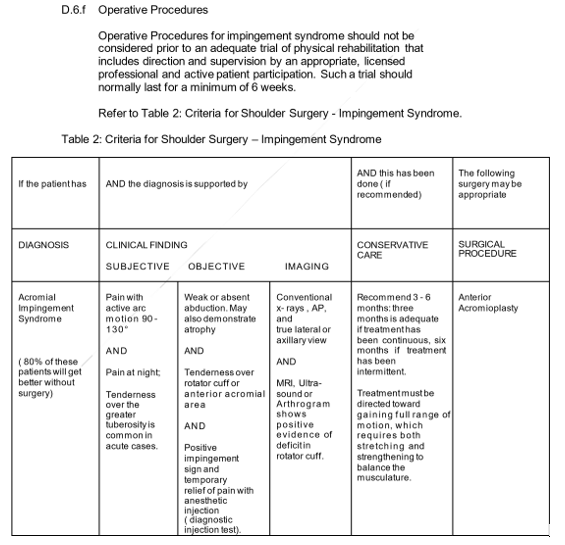
Before a sufficient trial of physical therapy that involves direction and supervision by a suitable, licensed practitioner and active patient participation, surgical procedures for impingement syndrome should not be considered. A minimum of six weeks should typically pass during such a trial.
Post-Operative Procedures of Subacromial Space Injection
Individualised rehabilitation plans based on collaboration between the doctor, the surgeon, and the therapist could include the following:
- Abduction splint or sling;
- Vigorous posterior scapular stabilising training, passive glenohumeral range of motion, and gentle pendulum exercise can be implemented;
- Start isometric exercises and taking part in ADLs four weeks after surgery; or
- Consider starting light resistive exercise at six weeks after surgery, depending on the patient’s functional recovery; concurrently, returning to a light or limited duty may be feasible given the ability to handle “no repetitive overhead activity.”
- All active non-operative methods specified in Section E, Therapeutic Procedures: Non-Operative, should be taken into consideration. These include progressive resistive exercise starting at two months with a gradual return to full activity starting at 5-7 months.
- During the post-operative recuperation and rehabilitation, work restrictions should be assessed every four to six weeks with appropriate written notifications to the patient and the employer. If the patient’s progress stagnates, the provider should reassess the patient’s health and modify the treatment plan as necessary.
What our office can do if you have shoulder Impingement Syndrome
We have the experience to help you with their workers compensation injuries. We understand what you are going through and will meet your medical needs and follow the guidelines set by the New York State Workers Compensation Board.
We understand the importance of your workers compensation cases. Let us help you navigate through the maze of dealing with the workers compensation insurance company and your employer.
We understand that this is a stressful time for you and your family. If you would like to schedule an appointment, please contact us so we will do everything we can to make it as easy on you as possible.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
