General Guideline Principles for Introduction of Occupational
Work-Related Asthma for workers compensation patients
]The New York State workers compensation board has developed these guidelines to help physicians, podiatrists, and other healthcare professionals provide appropriate treatment for Introduction of Occupational_Work-Related Asthma.
These Workers Compensation Board guidelines are intended to assist healthcare professionals in making decisions regarding the appropriate level of care for their patients with ankle and foot disorders.
The guidelines are not a substitute for clinical judgement or professional experience. The ultimate decision regarding care must be made by the patient in consultation with his or her healthcare provider.
Introduction of Occupational Work Related Asthma
To cause airflow blockage, bronchial hyperresponsiveness, and underlying inflammation, asthma is a prevalent chronic condition of the airways. It is usual to experience increased airway reactivity to various stimuli.
Asthma symptoms that start or worsen at work are the hallmark of work-related asthma (WRA), typically brought on by exposure to a new chemical or environmental alteration. Occupational asthma (OA) and work-related asthma (WRA) are also included (WEA).
OA contains sensitizer-induced asthma, which develops occupational antigen sensitization, and irritant-induced asthma, which develops reactive airway disease brought on by irritating exposures. Each has a sizable risk of acute morbidity, a long-term impairment risk, and dangerous social and economic effects.
Occupational Asthma (OA)
The term “OA” refers to workplace asthma that has just started, and it can be brought on by exposure to either an irritant or a sensitizer. OA can also be divided into types with and without delay.
OA With Latency
-
All conditions of immunologically (sensitizer) caused asthma display OA with latency.
-
Agents known as sensitizers start an allergic (immunologic) reaction.
-
The latency period, or the interval between the initial exposure and the onset of symptoms, can last a few weeks to many years. It displays the period of time needed to induce an immune reaction to the allergen at work.
-
The time between the initial exposure and being sensitized, which causes asthma symptoms with reexposure, is occasionally a few months.
This division between high and low molecular weight substances helps to characterize the typical asthma mechanism, symptoms, and latency.
- Long-term exposure to low-level irritants can potentially cause late-onset OA.
OA Without latency
-
Exposure to irritants (gasses, fumes, vapors, and aerosols) causes an inflammatory reaction rather than an allergic one.
-
After getting exposed to irritating gasses, fumes, or chemicals such as nitrogen oxide, ammonia, and chloride, OA without latency may develop.
Work-Exacerbated Asthma (WEA)
When people with asthma are already present or currently experiencing it become more sensitive to certain irritants at work, such as:
-
Aerosols
-
Fumes
-
Vapors
-
Gases
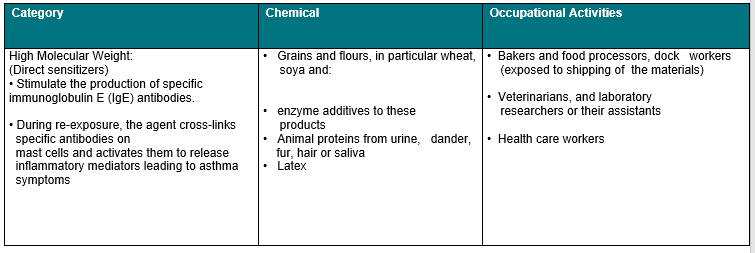
Table 1. Specific High and Low Weight Chemicals (Sensitizers) and Occupations
Etiology
The main symptoms of asthma are airway inflammation and responsiveness. The three main gestures of asthma are coughing, wheezing, and sporadic breathing difficulties.
Diagnosis of Work-Related Asthma
Signs and Symptoms of Work-Related Asthma
The main symptoms of asthma are airway inflammation and responsiveness. While coughing and sputum production are the main signs of bronchitis, episodic shortness of breath, wheezing, and coughing are also the main signs of asthma.
To diagnose OA, complete pulmonary history and diagnostic history are needed. American College of Cardiology For determining a diagnosis of WRA, doctors published the following criteria in 1995 (doi:10.1378/chest.108.4.1084), all of which must be met:
-
a background suggestive of occupational asthma.
-
airflow restriction is present and is reversible.
-
the existence of non-specific airway hyperresponsiveness when there is no airflow restriction.
-
The factual proof is that asthma is tied to a job.
Complications and Comorbid Conditions Relevant to Work
With a variety of secondary symptoms and issues that have an impact on everyday life and work, asthma can appear in complex ways. For instance, asthma may cause a persistent cough and secondary hoarseness, which may negatively affect certain occupations (e.g voice changes or the ability to carry on a conversation).
The condition known as gastroesophageal reflux disease (GERD), which can be worse by the effects of bronchodilator drugs on the lower esophageal sphincter, is frequently linked to asthma.
Although vocal cord dysfunction is not the same as asthma, it often coexists with it and can also be brought on by GERD or exposure to irritants.
Occupational / Work-Related Asthma
History Taking and Physical Exam of Occupational Work-Related Asthma
The foundation for diagnosis and treatment programs is laid forth by the history of occupational exposure, the symptoms, and the findings of diagnostic screening tests.
History of Present Illness
There should be documentation in the History of Present Illness (HPI).
-
Pulmonary exposures that are both occupational and non-occupational.
-
Occupation: past/current and variety of work activities (such as dock workers veterinarians, laboratory workers and those who produce chemicals, jewels, and alloys).
-
Duration of each job, including those held years or decades ago.
Exposures to:
-
The dust includes flour, grains, and wood.
-
Metals (aluminum and Platinum salts).
-
Exposure to fumes, gases, vapors (particularly isocyanates, ammonia, and solvents) smoke, and aerosols of chemicals or substances.
-
Non-occupational exposures to these agents should be mentioned in the history of exposure together with a description of the vulnerability, its length, and its intensity.
-
Exposure intensity Ideally, this information would include environmental measures (data on industrial hygiene) or at least a qualitative description of the exposure intensity, such as daily, weekly, monthly, yearly, etc.
-
Include inquiries describing the person’s obligations and exposure (e.g did you work in the office etc.).
Symptoms:
-
symptoms and when they first appeared
-
including grievances about:
-
throat constriction
-
breathing difficulty either during intake or expiration
-
loud breath noises
-
Sputum production from cough
-
ongoing bronchitis
-
chest constriction
The length, beginning, and frequency of symptoms
-
progression of symptoms, including
-
In relation to the workplace, the symptoms’ deterioration, and improvement
-
changes to the workplace
-
Symptoms that change in proportion to days worked and days off (particularly when they get better on the weekends or during time off from work)
-
development of symptoms
-
The pattern of the symptoms by season
Document if:
-
After a single, high-level workplace inhalation exposure to an irritating fume, vapor, gas, smoke, or aerosol, symptoms started to appear envisage and testing of the lungs.
-
Earlier therapies.
-
Relation to work This involves an assessment of the likelihood that the ailment or injury is related to the job.
-
Ability to carry out regular tasks and job responsibilities.
-
Workplace history of room dimensions, ventilation, and usage of any PPE both now and in the past.
Past Medical History
-
Past medical history, which may or may not include pulmonary exposures and treatments (such as childhood asthma, bronchitis susceptibility, hay fever, pneumonia, and eczema).
-
Symptoms of endocrine, neoplastic, neurologic, dermatologic, rheumatologic, and other systemic disorders are included in the review of systems, although they are not the only ones.
-
The detailed history of smoking (including marijuana, vaping, etc.)
-
A thorough medical history including usage of beta-blockers, beta-converting enzyme inhibitors, and pulmonary medicines.
-
Both professional and recreational activities.
-
Imaging tests are done earlier.
-
Past surgical experience.
-
History of atopic disease in the family.
-
History of allergies (as well as a history of atopy).
Physical Examination of Occupational Work-Related Asthma
The following aspects of an occupational pulmonary physical examination should be present:
-
Vital indicators, such as calculated respiration rate and oxygen saturation
-
Generally speaking, functional abilities include being able to move easily, walk, change positions, dress, and undress while evaluating dyspnea symptoms and indicators.
-
Evaluation of the respiratory condition (e.g. use of accessory muscles, depth, nasal flaring, and rate).
-
Examination for pulmonary illness stigmata and probable causes, such as:
-
anomalies of the mucous membranes
-
Nasal edema, discharge, and polyps
-
clubbing Chest diameter from anterior to posterior
-
Palpation for:
-
anomalies of the chest wall
-
neck lumps and adenoma
-
Use of percussion to detect resonance
-
The diaphragm
-
Aeration
-
Consolidation or fluid interface suggestion
-
Auscultation for:
-
The ratio of inspiration to expiry
-
unexpected breath sounds (wheeze, rhonchi, crackles, rales)
-
Pleural rubs, in addition to the timing, place, and persistence of lung findings
-
Cardiac examination paying close attention to heart failure and cor pulmonale results
-
Examining the skin for illness symptoms, such as erythema nodosum (Sarcoidosis).
-
Cardiac examination paying close attention to heart failure and cor pulmonale results
What our office can do if you have workers compensation Injuries
We have the experience to help you with their workers compensation injuries. We understand what you are going through and will meet your medical needs and follow the guidelines set by the New York State Workers Compensation Board.
We understand the importance of your workers compensation cases. Let us help you navigate through the maze of dealing with the workers compensation insurance company and your employer.
We understand that this is a stressful time for you and your family. If you would like to schedule an appointment, please contact us so we will do everything we can to make it as easy on you as possible.
We are orthopedic surgeons and do not treat chest diseases. We will refer you to someone in your area who does treat respiratory symptoms.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
