General Guideline Principles for Gluteus Medius Tendinosis and
Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain
Syndrome and Trochanteric Bursitis
for workers compensation patients
The New York State workers compensation board has developed these guidelines to help physicians, podiatrists, and other healthcare professionals provide appropriate treatment for Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndome and Trochanteric Bursitis.
These Workers Compensation Board guidelines are intended to assist healthcare professionals in making decisions regarding the appropriate level of care for their patients with ankle and foot disorders.
The guidelines are not a substitute for clinical judgement or professional experience. The ultimate decision regarding care must be made by the patient in consultation with his or her healthcare provider.
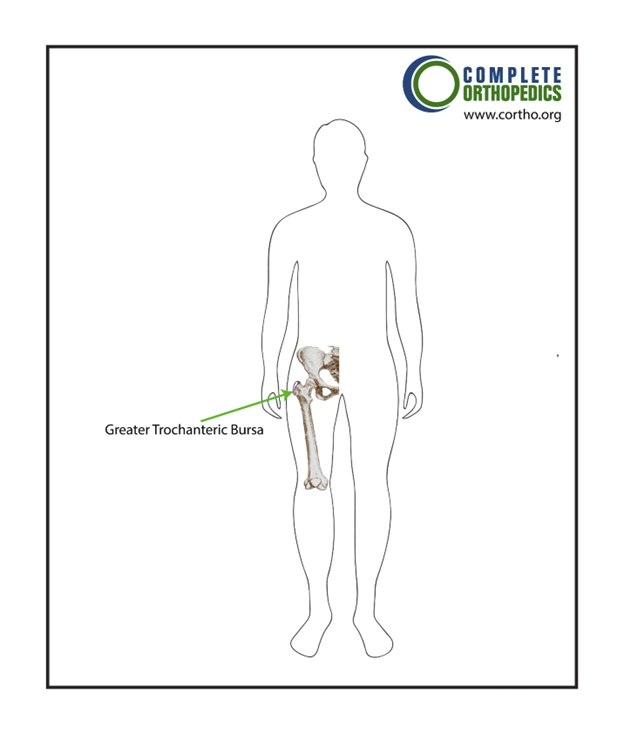
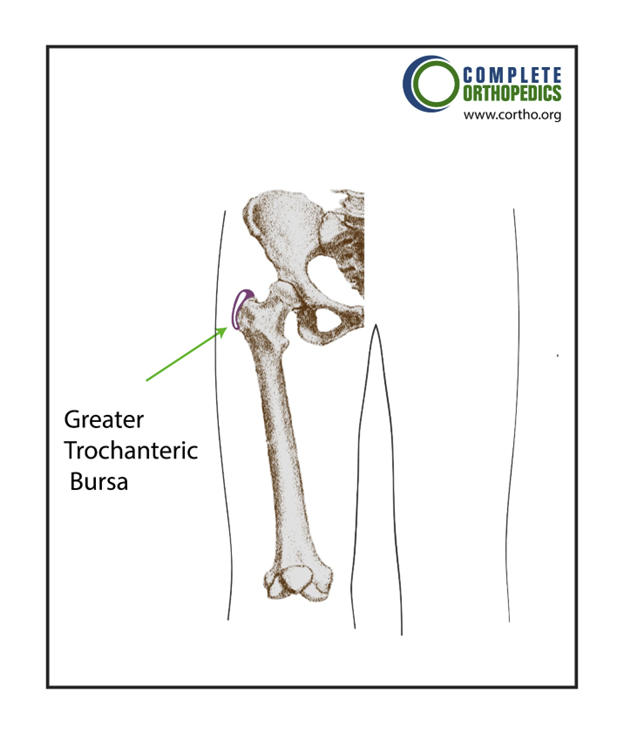
Location of greater trochanteric bursa
Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndome and Trochanteric Bursitis
Introduction of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndome and Trochanteric Bursitis
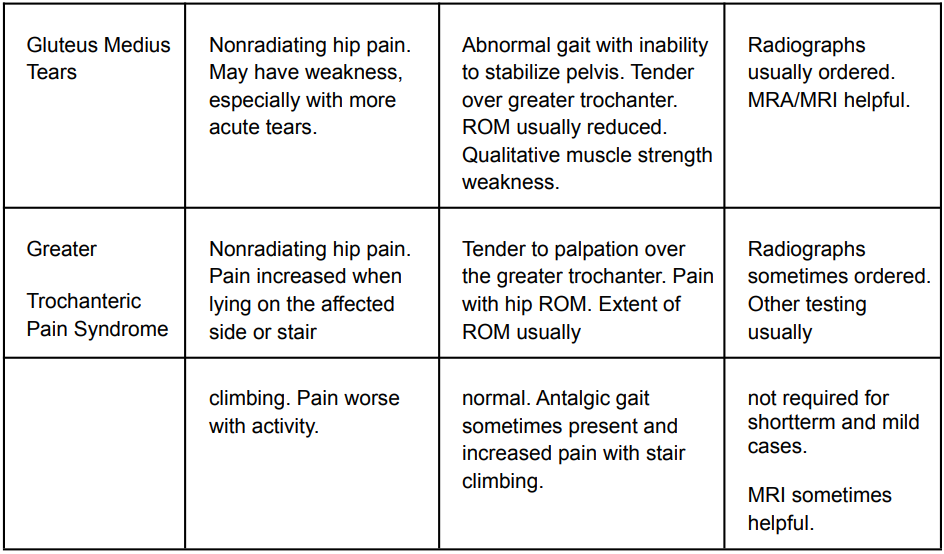
The examination criteria for greater trochanteric pain syndrome, trochanteric bursitis, and gluteus medius tendinopathy and tears (sometimes known as the “rotator cuff of the hip”) are summarised here.
Diagnostic Criteria for Non-Red-Flag Conditions
- MR ArthogramMR Arthogram is recommended to identify greater trochanteric pain syndrome and gluteus medius tendinosis or tearing in patients with subacute or persistent hip pain.
Indications: patients with increased trochanteric pain syndrome, subacute or chronic hip pain, symptoms, or clinical suspicion of gluteus medius tendinosis or tears Trochanteric bursitis sufferers should also take it into account, particularly if it is difficult to resolve.
Frequency/Dose/Duration: In most cases, just one arthrogram is required.
Rationale: In assessing and confirming gluteus medius tendinosis or rips, or greater trochanteric pain syndrome, MR arthrograms seem to be beneficial. In comparison to other imaging techniques, an enhanced MR arthrogram is advised for the diagnosis of trochanteric bursitis and gluteus medius tendinosis or tears because it provides for better labral examination.
It is advised for specific uses since it is probably the best imaging method available for these patients.
- MRIMRI is recommended in a small number of individuals with subacute or persistent lateral hip pain when the cause is unknown and to help with a proper diagnosis.
- UltrasoundUltrasound is recommended Hip discomfort in patients is thought to be caused by several conditions. Although arthrogram and MRI are typically the primary diagnostic procedures, ultrasonography can be useful in certain situations.
Frequency/Dose/Duration: Usually just once. The use of ultrasound is advised since it seems to be useful in diagnosing and verifying gluteus medius tendinopathies.
Medications of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndome and Trochanteric Bursitis
Ibuprofen, naproxen, or other NSAIDs from an earlier generation are suggested as first-line treatments for the majority of patients. For patients who are not candidates for NSAIDs, acetaminophen (or the analogue paracetamol) may be a viable alternative, even if the majority of research indicates it is just marginally less effective than NSAIDs.
There is proof that NSAIDs are less dangerous and just as effective in treating pain as opioids, such as tramadol.
- Non-Steroidal Anti-inflammatory Drugs (NSAIDs)Non-Steroidal Anti-inflammatory Drugs (NSAIDs) is recommended for the treatment of trochanteric bursitis, increased trochanteric discomfort, and gluteus medius tendinopathy or tears.
Indications – NSAIDs are advised as a treatment for trochanteric bursitis, increased trochanteric discomfort, and gluteus medius tendinosis or tears. First, try over-the-counter (OTC) medications to see whether they work.
Frequency/Duration – Many patients could find it reasonable to use as needed.
Indications for Discontinuation – Trochanteric bursitis, higher trochanteric discomfort, resolution of gluteus medius tendinosis or tears, ineffectiveness, or emergence of side effects requiring discontinuation are all possible outcomes.
- NSAIDs for Patients at High Risk of Gastrointestinal BleedingNSAIDs for Patients at High Risk of Gastrointestinal Bleeding is recommended Misoprostol, sucralfate, histamine Type 2 receptor blockers, and proton pump inhibitors are commonly used together by individuals who are at high risk of gastrointestinal bleeding.
Indications – Cytoprotective drugs should be taken into consideration for patients with a high-risk factor profile who also have indications for NSAIDs, especially if a prolonged course of treatment is planned. Patients who have a history of gastrointestinal bleeding in the past, the elderly, diabetics, and smokers are at risk.
Frequency/Dose/Duration – Proton pump inhibitors, misoprostol, sucralfate, H2 blockers recommended. Dose and frequency per manufacturer. There is not generally believed to be substantial differences in efficacy for prevention of gastrointestinal bleeding.
Indications for Discontinuation – Intolerance, development of adverse effects, or discontinuation of NSAID.
- NSAIDs for Patients at Risk for Cardiovascular Adverse EffectsNSAIDs for Patients at Risk for Cardiovascular Adverse Effects is recommended as far as cardiovascular side effects go, acetaminophen or aspirin as first-line medication seem to be the safest options. If necessary, non-selective NSAIDs are recommended to COX-2-specific medications.
To reduce the chance that an NSAID will negate the protective effects of low-dose aspirin in individuals receiving it for primary or secondary cardiovascular disease prevention, the NSAID should be taken at least 30 minutes after or 8 hours before the daily aspirin.
- AcetaminophenAcetaminophen is recommended for the treatment of trochanteric bursitis, increased trochanteric discomfort, and gluteus medius tendinosis or tears, especially in patients who are contraindicated for NSAIDs.
Indications – All patients with greater trochanteric pain, including acute, subacute, chronic, and post-operative pain, gluteus medius tendinosis, or tears.
Dose/Frequency – As per the manufacturer’s recommendations; can be used as required. Over four gm/day, there is evidence of liver toxicity.
Indications for Discontinuation – pain, side effects, or intolerance are gone.
- Opioids of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndome and Trochanteric BursitisPatients with trochanteric bursitis, increased trochanteric discomfort, or gluteus medius tendinosis or tears are rarely treated with opioids. They are more typically utilised for limited periods right after surgery.
- Opioids of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndome and Trochanteric BursitisOpioids of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndome and Trochanteric Bursitis are not recommended for trochanteric bursitis, increased trochanteric discomfort, or gluteus medius tendinosis or tears.
Rationale for Recommendations – Opioids have serious side effects, including poor tolerance, constipation, sleepiness, impaired judgement, memory loss, and the potential for overuse or dependency, which has been observed in up to 35% of patients.
Patients should be warned against using machinery or motor vehicles and aware of these possible side effects prior to receiving an opioid prescription. Opioids should only be used if necessary for severe pain or for a brief duration (not longer than one week) in the post-operative period because they do not seem to be any more efficient than safer analgesics at controlling the majority of musculoskeletal complaints.
- Opioids of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndome and Trochanteric BursitisOpioids of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndome and Trochanteric Bursitis are recommended for the selective treatment of individuals with increased trochanteric discomfort, trochanteric bursitis, or postoperative gluteus medius tendinosis or tears.
Indications – Treatment for post-operative gluteus medius tendinosis or tears, trochanteric bursitis, and larger trochanteric involves a brief course of opioid medication lasting a few days to no longer than one week. Following surgery, a small nocturnal dose of opioids may be beneficial. Prior to using opioids, the majority of patients should try NSAIDs and acetaminophen for pain relief. It is advised to stop using opioids as soon as possible.
Frequency/Dose/Duration – For the majority of epicondylar procedures, patients typically only need a few days to a week of opioid therapy.
Indications for Discontinuation – Resolution of the pain, adequate pain management with other medications, ineffectiveness, or the emergence of side effects necessitating termination.
- Opioids of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndome and Trochanteric BursitisOpioids of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndome and Trochanteric Bursitis are not recommended for trochanteric bursitis, increased trochanteric discomfort, or gluteus medius tendinosis or tears.
Treatments of Opioids of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndrome and Trochanteric Bursitis are
Therapeutic Exercise – Physical or Occupational Therapy
Therapeutic Exercise – Physical or Occupational Therapy is recommended for the treatment of gluteus medius tendinosis and rips, greater trochanteric pain syndrome, and trochanteric bursitis, in addition to addressing any weakness in the lateral hip musculature.
Frequency/Dose/Duration –With verification of continued objective functional progress, the total number of visits may be as low as two to three for individuals with minor functional deficits or as high as 12 to 15 for those with more severe deficits.
If there is evidence of functional improvement toward particular objective functional goals (such as increasing range of motion or improving capacity to conduct work activities), more than 12 to 15 visits may be necessary to address persistent functional impairments.
A home exercise regimen should be created and followed in conjunction with the therapy as part of the rehabilitation strategy.
Indications for Discontinuation – Resolution, post-surgical recovery, intolerance, ineffectiveness, or non-compliance.
Injection Therapy of Opioids of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndrome and Trochanteric Bursitis are
Glucocorticosteroid Injections
Glucocorticosteroid Injections is recommended as a possible course of treatment for gluteus medius tears with concurrent clinical bursitis, greater trochanteric pain syndrome, acute, subacute, or chronic trochanteric bursitis. Trochanteric bursitis symptoms that have persisted for at least a few weeks with prior NSAID or acetaminophen treatment and avoidance of aggravating activities are indicators.
Frequency/Dose/Duration: Three injections at most. Instead of scheduling a series of three injections, each injection should be scheduled independently, and its effects should be assessed before scheduling any more. Targeting the area that is most delicate is advised.
Although it is not necessary for a first injection, fluoroscopic guidance is a more logical choice for a follow-up shot, particularly if the first shot is unsuccessful.
Glucocorticosteroid injections are a therapy option, especially when NSAID trials, exercise, or other conservative therapies have yielded subpar outcomes.
Surgery of Opioids of Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndrome and Trochanteric Bursitis are
- Surgical RepairSurgical Repair is recommended for gluteus medius tears that do not improve with treatment from a doctor.
Indications/Rationale: Surgery is thought to be an effective treatment for gluteus medius tendon tears that are accompanied by discomfort and/or functional impairments.
In general, it is advised to try non-operative treatment for at least 3 weeks to see whether the function and pain can improve enough to avoid surgery.
- Post Operative Therapeutic Exercises – Physical / Occupational TherapyPost Operative Therapeutic Exercises – Physical / Occupational Therapy is recommended for patients who had their gluteus medius rips surgically repaired.
Indications: Programs must be customised based on aspects such preoperative health, bone quality, immediate surgical outcomes, contraindications, and other medical issues.
Frequency/Dose/Duration: Duration is determined mostly by the rate of improvement; two or three times per week for four to six weeks in an outpatient setting are gradually shortened when home exercises are implemented and the patient’s recovery progresses.
What our office can do if you have workers compensation Gluteus Medius Tendinosis and Tears (“Rotator Cuff of the Hip”) Greater Trochanteric Pain Syndrome and Trochanteric Bursitis
We have the experience to help you with their workers compensation injuries. We understand what you are going through and will meet your medical needs and follow the guidelines set by the New York State Workers Compensation Board.
We understand the importance of your workers compensation cases. Let us help you navigate through the maze of dealing with the workers compensation insurance company and your employer.
We understand that this is a stressful time for you and your family. If you would like to schedule an appointment, please contact us so we will do everything we can to make it as easy on you as possible.
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.