General Guideline Principles for History Taking and
Physical Examination of Hand, Wrist and Forearm Injuries
for workers compensation patients
The New York State workers compensation board has developed these guidelines to help physicians, podiatrists, and other healthcare professionals provide appropriate treatment for History Taking and Physical Examination of Hand, Wrist and Forearm Injuries.
These Workers Compensation Board guidelines are intended to assist healthcare professionals in making decisions regarding the appropriate level of care for their patients with ankle and foot disorders.
The guidelines are not a substitute for clinical judgement or professional experience. The ultimate decision regarding care must be made by the patient in consultation with his or her healthcare provider.
History Taking and Physical Exam of Hand, Wrist and Forearm Injuries
Physical examination and history-taking lay the groundwork for and direct the progression of diagnostic and therapeutic procedures. When findings from clinical evalua tions and those from other diagnostic techniques do not agree, preference should be given to the objective clinical findings. The following should be appropriately documented in the medical records.
History Of Present Injury (HPI) of Hand, Wrist and Forearm Injuries
- Gender, age, and hand dominance.
- Mechanism of injury: includes information on when symptoms first appeared (date), how they developed over time, and if a triggering event was involved or not. Activity before or prior to symptom onset
- Prior injuries to the same area, both occupational and non-occupational, including particular prior treatments.
- Location of symptoms.
- Symptoms include discomfort, tingling, numbness, weakness, stiffness, swelling, reduced range of motion, and changes in temperature, wetness, and colour.
- Symptom-exacerbating and -alleviating variables. Determine the precise physical elements that worsen or improve the issue.
- The greatest and worst times of the day for symptoms are when you first get up and after work.
- If symptoms subside when not at work (weekends, vacations).
- For serious injuries, take note of whether the region ever swelled and, if so, how quickly that happened (immediately or delayed). Hand/finger \sdeformity.
- Detailed pain diagrams are used to better pinpoint pain symptoms.
- Sleep disturbances
- The patient also made note of further related symptoms and indicators.
- Ability to carry out daily living activities (ADLs) and work-related activities. Evaluation of the overall level or combination of restrictions
- Ability to carry out daily living activities (ADLs) and work-related activities. Evaluation of the overall level or combination of restrictions
- Discuss any symptoms that the damaged extremity may be experiencing.
- Relation to work: This involves an assessment of the likelihood that the ailment or injury is related to the job.
- Medicines used to treat present symptoms: Medications? Splints? Ice/heat?
- Rest? Surgery? Other? Have any treatments proven to be effective? What medical procedures didn’t work?
Past History of Hand, Wrist and Forearm Injuries
Neoplasm, gout, arthritis, diabetes, overweight/obesity, hypothyroidism, other endocrinopathies, pregnancy, osteoarthrosis, rheumatoid arthritis, other arthritides, renal disease, systemic lupus erythematosus, and spondyloarthropathy are only a few examples of past medical conditions;
- Symptoms of rheumatologic, neurologic, endocrine, neoplastic, and other systemic disorders are included in the review of systems, but are not limited to them
- Smoking history
- Avocational and extracurricular activities
- Previous examinations, scans, diagnostic procedures, or treatments, together with their outcomes
- Past surgical history
- Psychosocial history
Physical Examination of Hand, Wrist and Forearm Injuries
The joint above and below the afflicted area should be examined, as well as the unaffected side for comparison. A physical examination should use procedures and tests that are appropriate for the joint or area being evaluated, such as:
Visual inspection: Look for and note asymmetries and abnormalities that might indicate degeneration, deformity, fracture, or dislocation. Examine both hands, wrists, and forearms. Keep an eye out for any indications of severe wounds, such as degloving injuries, lacerations, puncture wounds, open wounds, and crush injuries.
Peripheral pulses, motor function, reflexes, and sensory status should all be considered while evaluating the neurologic and vascular status of the hand, wrist, forearm, and upper limb.
Additionally, any dystrophic alterations or variations in skin tone or turgor should be described. Most patients should also have their neck and cervical nerve root function examined.
Palpation of Hand, Wrist and Forearm Injuries
Range of motion (ROM) and quality of motion (active and passive); It is important to measure ROM both actively and passively for the hand, wrist, and forearm. Mobility on the effected and uneffected sides should be compared.
Strength (atrophy/weakness)
Joint stability and integrity should be evaluated by stressing the ligaments and comparing the results to the other side that is unaffected.
A deformity, displacement, and swelling examination
As clinically warranted, evaluate the foot and ankle neurologic (motor, sensory, and reflex) and vascular state (integrity of distal circulation, peripheral pulses, skin temperature). Most patients should also have their neck and cervical nerve root function examined.
Keep an eye out for any indicators of significant wounds, such as degloving, lacerations, puncture wounds, open wounds, and crush wounds.
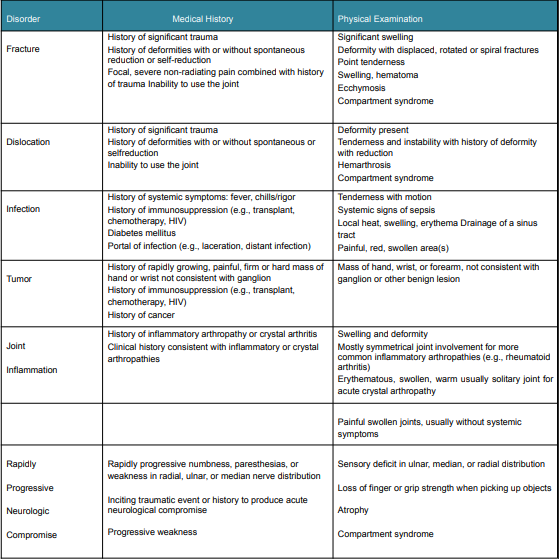
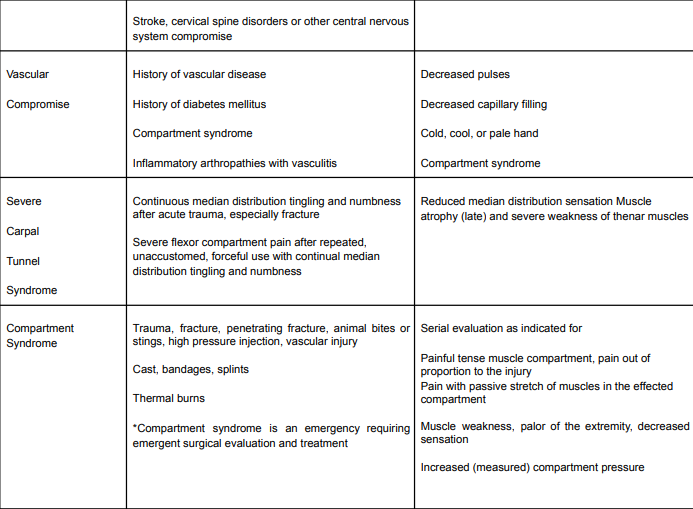
Red Flags of Hand, Wrist and Forearm Injuries
Red flags are observations that suggest potentially significant and urgent medical issues. Evaluation of red flags that require urgent/emergent assessment and treatment should be part of the assessment (history and physical examination), as clinically required. Changes in clinical care brought on by “red flags” are incorporated into the Hand Wrist and Forearm MTG.
For suggestions on how to perform a physical examination for each ailment, see table 4 and the individual conditions.
Assessing Red Flags of Hand, Wrist and Forearm Injuries
Table 3 provides a summary of potentially significant disorders affecting the hand, wrist, and forearm. Depending on the provider’s expertise and experience in treating the specific illness, early consultation by a hand or upper limb specialist, rheumatologist, or other relevant specialist is advised.
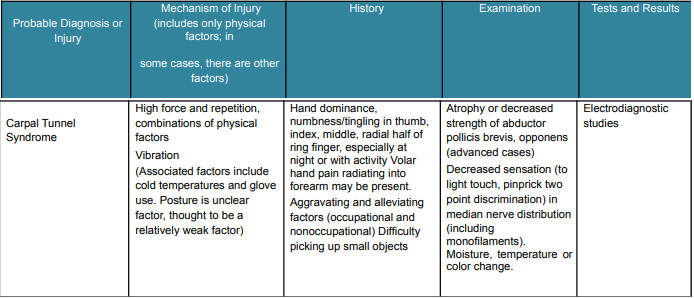
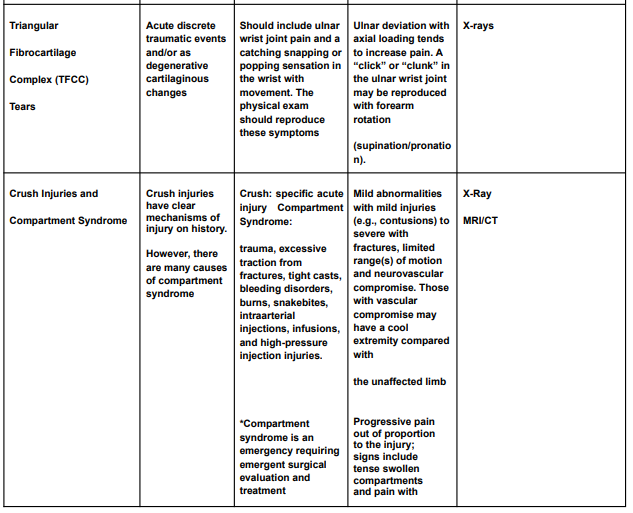
Diagnostic Criteria of Hand, Wrist and Forearm Injuries
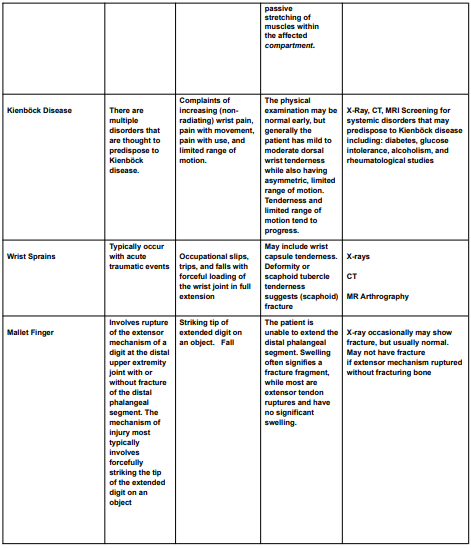
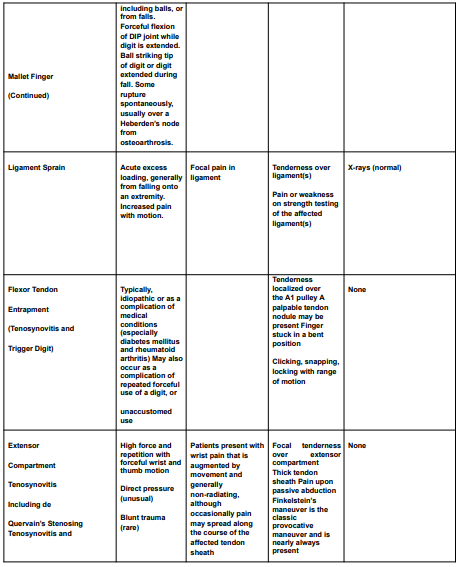
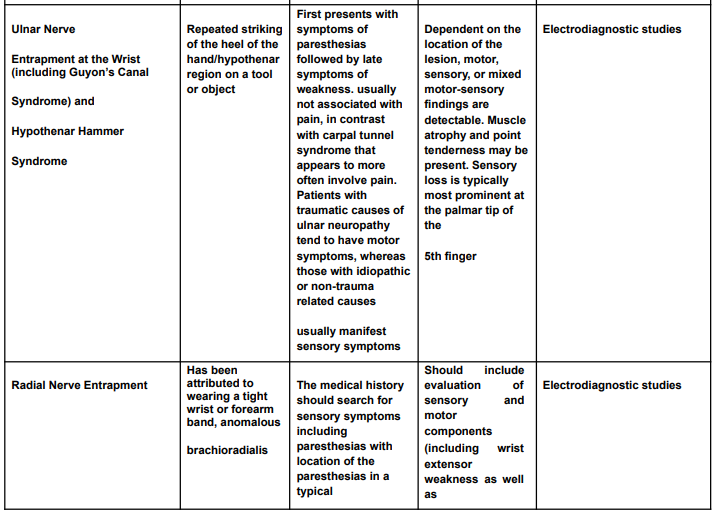
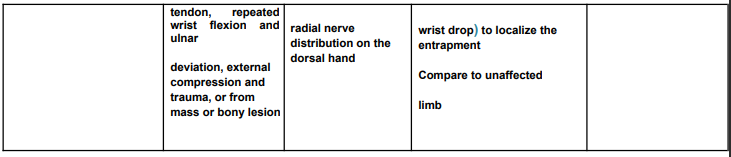
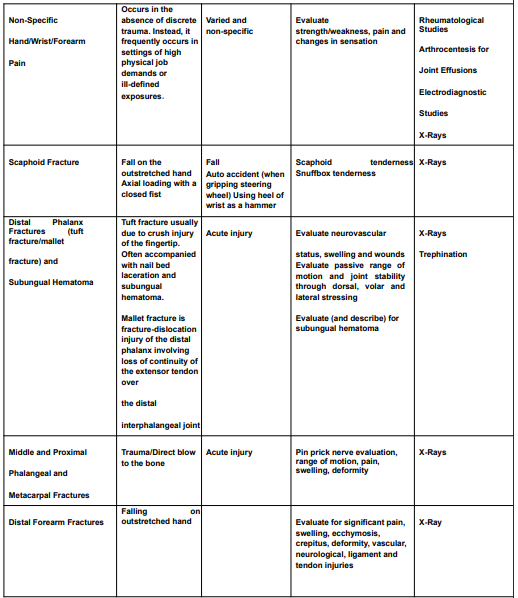
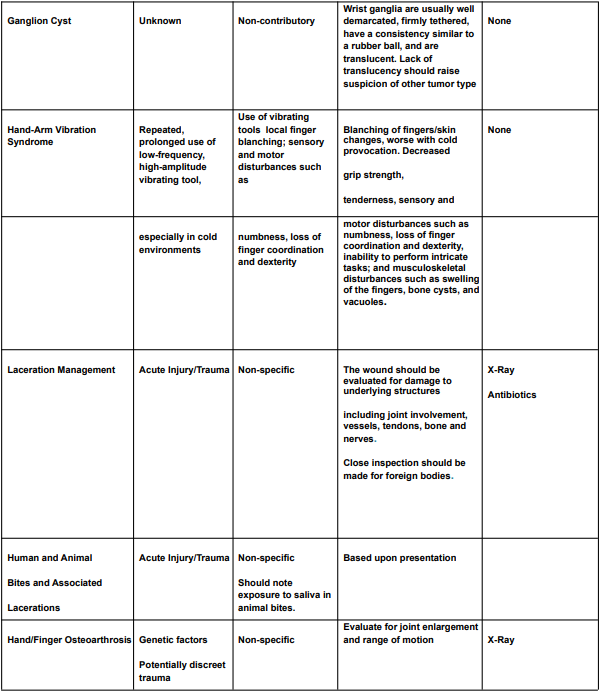
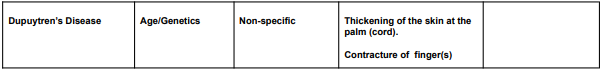
The diagnostic criteria for hand, wrist, or forearm disorders are listed in the Diagnostic Criteria for Hand, Wrist, or Forearm Disorders table (Table 4) and include the probable diagnosis or injury, potential mechanisms of illness or injury, symptoms, signs, and appropriate tests and results to take into account in assessment and treatment.
Rehabilitation Principles of Hand, Wrist and Forearm Injuries
Rehab (supervised formal therapy) needed after a work-related injury should be concentrated on regaining the functional ability needed to meet the patient’s daily and work obligations and enable them to return to work, with the goal of returning the injured worker to their pre-injury status to the extent that is practical.
Active therapy calls for the patient to put in an internal effort to finish a particular activity or assignment. The procedures known as passive therapy rely on modalities that are administered by a therapist rather than the patient exerting any effort on their side.
Passive therapies are typically seen as a way to speed up an active therapy programme and achieve concurrently objective functional gains. Over passive interventions, active initiatives should be prioritised.
To sustain improvement levels, the patient should be advised to continue both active and passive therapies at home as an extension of the therapeutic process.
To facilitate functional gains, assistive devices may be used as an adjuvant measure in the rehabilitation strategy.
What our office can do if you have workers compensation Injuries
We have the experience to help you with their workers compensation injuries. We understand what you are going through and will meet your medical needs and follow the guidelines set by the New York State Workers Compensation Board.
We understand the importance of your workers compensation cases. Let us help you navigate through the maze of dealing with the workers compensation insurance company and your employer.
We understand that this is a stressful time for you and your family. If you would like to schedule an appointment, please contact us so we will do everything we can to make it as easy on you as possible.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
