Percutaneous Lumbar Disc Laser Decompression
Overview
The herniation of the intervertebral disc occurs when the nucleus pulposus comes out through a defect in the annulus fibrosus. Lumbar intervertebral disc herniation is a frequent cause of low back pain and radiating pain in the lower extremities, known as sciatica. Surgical interventions are indicated once the medical management has failed. Laser disc decompression is a minimally invasive surgical technique used to decompress the pinched spinal nerves.
Low back pain and sciatica are common complaints in middle-aged adults and in adults with work-related or traumatic injuries. Lumbar disc herniation is a frequent cause and is more common in the lumbar spine due to the excessive load at the lower spine.
Intervertebral discs consist of a soft gelatinous center (nucleus pulposus) which is contained inside a tough outer ring (annulus fibrosus). Cracks may appear in the outer ring due to degenerative disc disease or due to repetitive actions or trauma. The soft inner center may herniate through the annulus and lead to thinning of the outer ring. At times, the nucleus may be extruded out of the outer ring completely.
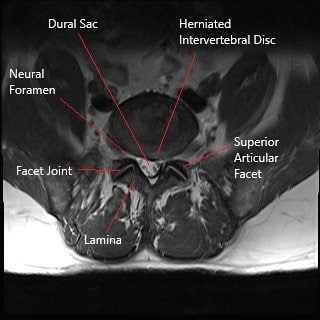
Axial section section of lumbar spine showing herniated intervertebral disc.
The herniated intervertebral disc creates local inflammation and compresses the exiting or traversing spinal nerve roots. The compression of the nerve roots and the dural sac may lead to symptoms of paraesthesia, pain, and weakness in the area supplied by the nerve root. The intervertebral disc is supplied by the sinovertebral nerves arising from the nerve roots. The sinovertebral nerves are irritated as a result of herniation and lead to low back pain.
Diagnosis
The herniated intervertebral disc is diagnosed clinically by the physician. The physician may request radiological studies for further investigation. An x-ray allows the physician to see the bony structure of the lumbar spine. The x-ray image is able to show arthritic changes in the lumbar spine, any fractures, or any narrowing of the canal. MRI is often the study most useful for diagnosing a herniated disc. The MRI images are able to show all the soft tissue structures in the lumbar spine including the nerves.
Treatment
The herniated disc is initially managed with modification of activity, nonsteroidal anti-inflammatory medications, and physical therapy. Additional relief may be obtained from heat, cold, and compression therapy. Some patients may require additional measures such as nerve root blocks and epidural steroid injections.
Surgical intervention in the form of disc decompression is recommended in patients who have tried non-surgical methods for at least 6 weeks. Patients with cauda equina syndrome and those with progressive weakness or numbness of the lower extremities may require immediate surgical decompression.

Intraoperative image of lumbar microdiscectomy surgery.
Patients without cauda equina syndrome or with power sensory loss may benefit from minimally invasive techniques such as laser disc decompression. The laser disc decompression works on the principle of thermal ablation of the nucleus pulposus of the involved disc.
The heat energy generated from the laser probe inside the nucleus leads to shrinkage of the nucleus pulposus. The decrease in the pressure inside the disc leads to the resorption of the extruded/herniated disc inside. The thermal energy also leads to a decrease in pain from the sinovertebral nerves.
Laser disc decompression may be done in an outpatient setting under local anesthesia. The physician uses a numbing medication in the lower back at the site of the insertion. The physician then uses intraoperative fluoroscopy to direct a needle/catheter inside the herniated intervertebral disc. The fluoroscopy is used to verify the position and a dye may be used to make sure the needle is at the right place.
The physician then introduces a fiber optic through the catheter to reach the center of the nucleus pulposus. Nd-YAG laser energy is transmitted through the fiber optic to heat the nucleus pulposus. The thermal energy leads to shrinkage of the center of the disc. The catheter is then withdrawn and a small bandage is applied at the incision site.
The patients are able to go home the same day of the procedure. The majority of the patients experience significant relief from laser decompression. However, there may be potential complications from the use of high-energy lasers.
The thermal energy from the laser may dissipate outside the nucleus pulposus leading to damage to the vertebral bodies and the spinal nerves. Similarly, while inserting the catheter, there may be damage to the dural sac and the nerve roots. There may be inadequate shrinkage of the nucleus pulposus leading to continued symptoms.
Nucleoplasty is a similar procedure but utilizes radiofrequency energy instead of laser energy. The radiofrequency uses less thermal energy as compared to the laser. Despite the advent of laser and radiofrequency nucleoplasty, microdiscectomy surgery remains the gold standard in the management of a herniated intervertebral disc.
The microdiscectomy surgery is performed using an operating microscope and the herniated disc material is removed under direct vision. Speak with your spine surgeon regarding, which procedure may be best suited for you.
Do you have more questions?
What is a herniated disc?
A herniated disc occurs when the soft, gel-like center (nucleus pulposus) of an intervertebral disc pushes through a crack in the tough outer layer (annulus fibrosus).
¿Qué es una hernia discal?
Una hernia discal se produce cuando el centro blando y gelatinoso (núcleo pulposo) de un disco intervertebral empuja a través de una grieta en la dura capa externa (anillo fibroso).
What causes a herniated disc?
Herniated discs can result from degenerative disc disease, trauma, repetitive stress, or heavy lifting.
What non-surgical treatments are available for a herniated disc?
Treatments include physical therapy, NSAIDs, activity modification, heat/cold therapy, nerve root blocks, and epidural steroid injections.
What are the symptoms of a herniated disc?
Symptoms include low back pain, sciatica, numbness, tingling, and weakness in the legs.
When is surgery considered for a herniated disc?
Surgery is considered when non-surgical treatments fail after at least six weeks or if there is severe nerve compression causing significant symptoms.
What is laser disc decompression?
Laser disc decompression is a minimally invasive procedure that uses laser energy to shrink the nucleus pulposus, relieving pressure on the nerves.
When is surgery considered for a herniated disc?
Surgery is considered when non-surgical treatments fail after at least six weeks or if there is severe nerve compression causing significant symptoms.
What non-surgical treatments are available for a herniated disc?
Treatments include physical therapy, NSAIDs, activity modification, heat/cold therapy, nerve root blocks, and epidural steroid injections.
How is laser disc decompression performed?
Under local anesthesia, a needle and fiber optic are inserted into the disc using fluoroscopic guidance. Laser energy is then applied to shrink the disc material.e
What is the recovery like after laser disc decompression?
Most patients can go home the same day and experience significant pain relief, though they should avoid strenuous activities during recovery.
What are the risks of laser disc decompression?
Risks include thermal damage to nearby structures, inadequate shrinkage of the disc, and potential injury during needle insertion.
How does nucleoplasty differ from laser disc decompression?
Nucleoplasty uses radiofrequency energy instead of laser energy, generating less heat and reducing the risk of thermal damage.
What are the benefits of microdiscectomy over other procedures?
Microdiscectomy allows for precise removal of the herniated disc material, making it the gold standard for herniated disc surgery.
What is microdiscectomy surgery?
Microdiscectomy is a surgical procedure where the herniated disc material is removed under direct vision using an operating microscope.
What are the risks of microdiscectomy surgery?
Risks include infection, bleeding, nerve damage, and recurrence of the herniation.
How long is the recovery after microdiscectomy surgery?
Recovery time varies, but most patients can return to normal activities within a few weeks to a few months.
Can a herniated disc heal on its own?
In some cases, herniated discs can heal with conservative treatment over time, but severe cases may require surgery.
What is cauda equina syndrome?
Cauda equina syndrome is a serious condition where severe compression of the nerve roots in the lower spine causes loss of bowel or bladder control and leg weakness, requiring immediate surgery.
Is it possible to prevent a herniated disc?
Preventative measures include maintaining good posture, regular exercise, proper lifting techniques, and avoiding excessive strain on the back.
How do I know which treatment is best for my herniated disc?
The best treatment depends on the severity of symptoms, response to non-surgical treatments, and overall health. Consulting with a spine specialist can help determine the most appropriate treatment.
What lifestyle changes can help manage a herniated disc?
Lifestyle changes include staying active, losing weight if overweight, avoiding prolonged sitting, and strengthening the core muscles.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
