Nucleoplasty and microdiscectomy are two minimally invasive surgical procedures aimed at relieving symptoms caused by lumbar disc herniation or bulging discs. Both procedures help to decompress the spinal nerve roots, which are often compressed by herniated disc material, leading to pain, numbness, and weakness in the legs. While both procedures are effective, they differ in their techniques, indications, and suitability for different types of disc problems.
How Common It Is and Who Gets It? (Epidemiology)
Lumbar disc herniation and disc bulging are common causes of lower back pain and sciatica, especially in individuals aged 30 to 50, and in those who perform heavy lifting or repetitive movements. Sciatica, characterized by pain radiating down the legs, is a frequent symptom of lumbar disc herniation. Approximately 10% of individuals with lumbar disc issues require surgical intervention, with the choice of procedure depending on the severity and type of the disc issue.
Why It Happens – Causes (Etiology and Pathophysiology)
A herniated or bulging intervertebral disc occurs when the soft, inner part of the disc (nucleus pulposus) pushes through cracks in the outer, tougher part (annulus fibrosus). This may lead to nerve compression, which causes symptoms such as radiating pain, numbness, and weakness in the lower limbs. The disc degeneration can result from:
- Age-related wear and tear: The disc loses water content, leading to cracking and bulging.
- Trauma or injury: Sudden pressure or repetitive stress on the spine can cause disc herniation.
- Repetitive strain: Activities that put strain on the spine, such as lifting or poor posture, can also contribute to disc problems.
How the Body Part Normally Works? (Relevant Anatomy)
The lumbar spine is made up of five vertebrae (L1-L5) separated by intervertebral discs. The discs serve as shock absorbers and allow movement between vertebrae. The spinal cord runs through the spinal canal and nerve roots exit through openings called foramina. These nerves control sensation and movement in the legs, and when compressed by a herniated or bulging disc, they can lead to pain, numbness, and weakness in the affected area.
What You Might Feel – Symptoms (Clinical Presentation)
Common symptoms of lumbar disc herniation or bulging discs that may require nucleoplasty or microdiscectomy include:
- Radiating Pain: Pain that travels from the lower back down through the buttocks and legs (sciatica).
- Numbness and Tingling: Sensations of pins and needles in the legs or feet.
- Weakness: Difficulty in moving the legs or feet, or clumsiness when walking.
- Back Pain: Pain localized in the lower back, often worsened by movement or prolonged sitting.
How Doctors Find the Problem? (Diagnosis and Imaging)
To diagnose a herniated or bulging disc and determine the need for surgery, doctors typically use:
- Physical Examination: To assess reflexes, strength, and nerve function.
- MRI (Magnetic Resonance Imaging): The best imaging technique for visualizing soft tissues, including herniated discs and nerve compression.
- CT Scan: Useful for detailed bone images, especially in the case of spinal stenosis.
- X-rays: To check for structural abnormalities or degenerative changes.
- Electromyography (EMG): Measures the electrical activity of muscles and helps to assess nerve function.
Classification
Nucleoplasty and microdiscectomy are both minimally invasive but vary in their applications:
- Nucleoplasty: Primarily used for single-level disc bulges with less than 50% loss of disc height.
- Microdiscectomy: Typically performed for larger herniations or extrusion of disc material. It involves removing herniated disc material that is pressing on the nerve root.
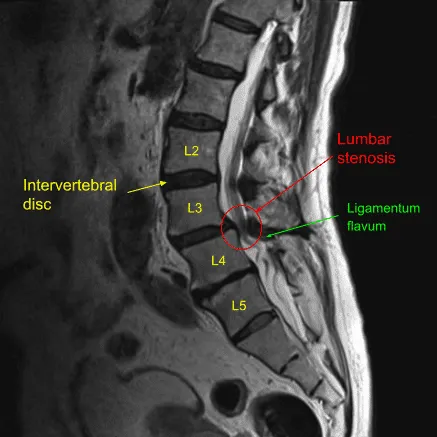
MRI of the lumbar spine in the sagittal section showing L4-L5 disc herniation.
Nucleoplasty vs Microdiscectomy
Nucleoplasty is a minimally invasive surgical technique that allows the surgeon to decompress the nerves. Minimally invasive surgery means there is minimum trauma to the structures surrounding the disc while performing the surgery. Nucleoplasty may be performed in an outpatient setting under local anesthesia. The patient remains semi conscious during the procedure while the area where the surgery is performed is anesthetized.
After adequate anesthesia, the surgeon inserts a needle in the involved intervertebral disc. The needle is guided by an external x-ray image intensifier. After the correct position of the needle is verified, the surgeon inserts a thermal-cautery/radiofrequency device. The thermal cautery or the radiofrequency device works by heating the nucleus pulposus.
The heating of the nucleus pulposus leads to shrinkage of the nucleus pulposus (nucleoplasty). The heat generation also leads to the remodeling of the annulus fibrous ring. The shrinkage of the pulposus along with the closure of the cracks leads to relief from disc bulge. After the needle is withdrawn, the entry site is closed with a bandage.
While the heat helps in the shrinkage of the nucleus pulposus, the surrounding tissues such as nerves, muscles, and bone is not damaged. The procedure involves minimum cutting of the tissues leading to a quicker rehabilitation. The patients are able to go home the same day of the procedure.
Microdiscectomy surgery involves a small incision and removal of the herniated disk under the direct vision of the surgeon. The procedure may be performed under general anesthesia in a hospital or in an outpatient setting under local anesthesia. The surgeon carefully separates the tissues to reach the involved spine segment. A small part of the lamina is removed to visualize the intervertebral disc.
The surgeon carefully retracts the spinal nerve roots and punches out small bits of the herniated intervertebral disk. The surgeon may also remove any bone spurs and widen the spinal canal in case of spinal stenosis. The procedure may be performed with an open traditional approach or using an endoscope (minimally invasive technique).
While nucleoplasty is less invasive than microdiscectomy, nucleoplasty can only be performed in limited circumstances. Nucleoplasty is only performed in patients in whom there is a single-level disc bulge. The procedure is limited to patients in whom the cause of symptoms is diagnosed to be solely because of the disk. Similarly, herniation and extrusion of the disc are managed with microdiscectomy rather than nucleoplasty. Nucleoplasty is only used to treat disc bulges with less than 50% loss of diameter.
Microdiscectomy may be combined with laminectomy surgery to relieve symptoms of spinal canal stenosis. Spinal lumbar fusion surgery is better suited in cases of spine instability. Both nucleoplasty and microdiscectomy are highly successful procedures for the management of discogenic pain. Speak with your spine surgeon to determine the procedure best suited for your condition.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that mimic the symptoms of lumbar disc herniation include:
- Spinal Stenosis: Narrowing of the spinal canal or nerve foramen, leading to nerve compression.
- Piriformis Syndrome: Compression of the sciatic nerve by the piriformis muscle in the buttocks.
- Facet Joint Syndrome: Degenerative changes in the facet joints of the spine can also lead to pain and radiating symptoms.
- Sacroiliac Joint Dysfunction: Inflammation or dysfunction of the sacroiliac joint can cause lower back and leg pain.
Treatment Options
Non-Surgical Care
- Physical Therapy: Aimed at strengthening the back muscles and improving flexibility.
- Medications: Pain relief from NSAIDs, corticosteroids, or muscle relaxants.
- Epidural Steroid Injections: To reduce inflammation around the spinal nerves.
- Nerve Blocks: For targeted pain relief.
Surgical Care
- Nucleoplasty: A minimally invasive technique where a needle is inserted into the affected disc to apply radiofrequency or thermal energy, shrinking the nucleus pulposus and relieving pressure on the nerve.
- Microdiscectomy: A minimally invasive procedure where a small portion of the herniated disc is removed under direct visualization, typically performed through a small incision.
Recovery and What to Expect After Treatment
- Nucleoplasty:
- Recovery is typically quick, as the procedure involves minimal tissue disruption. Patients may return home the same day.
- Most patients experience pain relief within a few weeks, although full recovery may take a few months.
- Microdiscectomy:
- Recovery takes a bit longer compared to nucleoplasty, but patients typically resume normal activities within 2-4 weeks.
- Full recovery, especially for more extensive disc issues, may take several months, with physical therapy to strengthen the back.
Possible Risks or Side Effects (Complications)
- Nucleoplasty:
- Inadequate Decompression: The procedure may not fully relieve symptoms, especially in cases of large herniations.
- Nerve Injury: Although rare, there is a small risk of nerve injury due to the heat generated during the procedure.
- Infection: As with any minimally invasive surgery, infection is a possible complication.
- Microdiscectomy:
- Infection: At the surgical site.
- Nerve Damage: Rare, but possible during the procedure.
- Recurrent Herniation: Some patients may experience a re-herniation at the same level.
- Dural Tear: Accidental damage to the dura mater, the protective covering of the spinal cord, which may require repair.
Long-Term Outlook (Prognosis)
Both nucleoplasty and microdiscectomy have high success rates in relieving symptoms of radiculopathy caused by lumbar disc herniation or bulging discs. However, the long-term outcome depends on factors such as the extent of the herniation, patient age, and the presence of other spinal conditions. In some cases, re-herniation or further degeneration may occur, but the overall prognosis for both procedures is generally favorable.
Out-of-Pocket Costs
Medicare
CPT Code 63030 – Lumbar Microdiscectomy: $225.06
CPT Code 63020 – Cervical Microdiscectomy: $271.49
CPT Code 63040 – Thoracic Microdiscectomy: $335.83
CPT Code 63047 – Lumbar Laminectomy: $271.76
CPT Code 62287 – Nucleoplasty (Percutaneous Disc Decompression): $137.26
Under Medicare, 80% of the approved amount for these procedures is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—typically cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved spinal surgeries. These supplemental plans coordinate directly with Medicare to ensure full coverage for the procedures.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or small residual charges. Most secondary insurance plans have a modest deductible, typically between $100 and $300, depending on the specific policy and network status.
Workers’ Compensation
If your spinal condition requiring these procedures is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your spinal injury is the result of a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses, including discectomy, laminectomy, and nucleoplasty procedures. The only possible out-of-pocket cost may be a small deductible depending on your individual policy terms.
Example
John, a 63-year-old patient with a herniated lumbar disc and chronic back pain, underwent lumbar microdiscectomy (CPT 63030) and nucleoplasty (CPT 62287) to relieve his symptoms. His estimated Medicare out-of-pocket costs were $225.06 for the lumbar discectomy and $137.26 for the nucleoplasty. Since John had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for the procedures.
Frequently Asked Questions (FAQ)
Q. How long does it take to recover from nucleoplasty or microdiscectomy?
A. Nucleoplasty has a quicker recovery time, with most patients returning to normal activities within a week or two. Microdiscectomy may take a bit longer, typically 2-4 weeks for light activity and a few months for full recovery.
Q. Which procedure is better for me: nucleoplasty or microdiscectomy?
A. Nucleoplasty is ideal for small bulging discs with less than 50% loss of disc height. Microdiscectomy is better for larger herniations or if the disc has extruded. Your spine surgeon will assess your condition and recommend the best approach.
Q. Are there risks involved with these procedures?
A. Both procedures carry minimal risks, with potential complications including nerve injury, infection, or incomplete decompression. However, the risks are low, and most patients experience significant improvement.
Summary and Takeaway
Nucleoplasty and microdiscectomy are effective minimally invasive procedures for treating lumbar disc herniation and bulging discs. Nucleoplasty is ideal for small disc bulges and offers a quicker recovery, while microdiscectomy is typically used for more significant herniations. Both surgeries have high success rates, but the choice between them depends on the extent of the disc issue and the patient’s specific condition.
Who Performs This Treatment? (Specialists and Team Involved)
Both nucleoplasty and microdiscectomy are typically performed by:
- Spine Surgeons: Orthopedic or neurosurgeons specializing in spinal disorders.
- Anesthesiologists: For anesthesia management during surgery.
- Physical Therapists: To assist in post-operative rehabilitation and recovery.
When to See a Specialist?
If you experience persistent or worsening back pain, sciatica, or other symptoms of a herniated disc that don’t improve with conservative treatments, consult a spine specialist to determine the best surgical option.
When to Go to the Emergency Room?
Seek emergency care if you experience:
- Sudden loss of bowel or bladder control.
- Severe, unmanageable pain.
- Sudden weakness or numbness in the legs or feet.
What Recovery Really Looks Like?
Nucleoplasty offers a quicker recovery, while microdiscectomy generally requires a few weeks for light activity and several months for full recovery. Both procedures have minimal downtime compared to traditional open surgery.
What Happens If You Ignore It?
Ignoring a herniated disc can lead to worsening symptoms, permanent nerve damage, and loss of function. Early surgical intervention is typically more successful and results in better long-term outcomes.
How to Prevent It?
Maintaining good posture, regular exercise, and proper lifting techniques can help prevent lumbar disc issues. Strengthening the core and back muscles is essential for spine health.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and anti-inflammatory foods can support spine health and reduce the risk of disc degeneration.
Activity and Lifestyle Modifications
After surgery, low-impact activities like walking or swimming are encouraged to promote healing and maintain flexibility. Avoid heavy lifting and high-impact activities during recovery.
Do you have more questions?
What is the main difference between microdiscectomy and nucleoplasty?
Microdiscectomy is a standard surgical procedure involving the removal of herniated disc material to relieve nerve pressure, often performed under general anesthesia. Nucleoplasty is a minimally invasive technique that uses thermal energy or radiofrequency to shrink and decompress the disc, suitable for smaller disc bulges.
Which procedure has a shorter recovery time?
Nucleoplasty generally has a shorter recovery time because it is minimally invasive, causing less tissue damage. Patients can often go home the same day and resume normal activities within a few days to weeks.
Can both procedures be performed under local anesthesia?
Yes, both procedures can be performed under local anesthesia. However, microdiscectomy is more commonly done under general anesthesia, especially in cases requiring more extensive surgery.
Which procedure is more effective in relieving severe nerve compression symptoms?
Microdiscectomy is generally more effective for severe nerve compression symptoms due to its ability to remove larger disc herniations and address more complex issues.
What kind of post-operative care is required for nucleoplasty?
Post-operative care for nucleoplasty includes rest, avoiding strenuous activities for a few days, and following a physical therapy regimen to strengthen the back and improve flexibility.
Can either procedure be performed on an outpatient basis?
Yes, both procedures can be performed on an outpatient basis, meaning the patient can go home the same day. However, microdiscectomy may require a short hospital stay in some cases.
What kind of post-operative care is required for microdiscectomy?
Post-operative care for microdiscectomy includes rest, wound care, gradually increasing activity, avoiding heavy lifting, and physical therapy to aid recovery and prevent future issues.
What are the chances of disc herniation recurrence after microdiscectomy?
Recurrence rates after microdiscectomy are around 5-15%. Following proper post-operative care and avoiding risk factors can reduce this risk.
Can nucleoplasty be performed on multiple disc levels?
Nucleoplasty is generally limited to single-level disc bulges. For multi-level issues, other procedures like microdiscectomy or fusion may be more appropriate.
How soon can patients return to work after each procedure?
Patients can typically return to work within a few days to a week after nucleoplasty, depending on the nature of their job. After microdiscectomy, patients may return to work within 2-4 weeks, depending on recovery and job demands.
What is the success rate of nucleoplasty in relieving pain?
The success rate of nucleoplasty in relieving pain ranges from 70-80%, depending on patient selection and the specific condition being treated.
Can physical therapy help in recovery after these procedures?
Yes, physical therapy is crucial in the recovery process for both nucleoplasty and microdiscectomy. It helps improve strength, flexibility, and overall spinal health, reducing the risk of recurrence.
What is the success rate of microdiscectomy in relieving pain?
The success rate of microdiscectomy is generally high, with 85-95% of patients experiencing significant pain relief and improved function.

