Open discectomy vs Microdiscectomy
Overview
Discectomy surgery is a gold standard surgical treatment for lumbar radiculopathy or sciatica. The surgery helps to alleviate symptoms of leg pain which may be associated with numbness or weakness of the extremities. While open discectomy has been in practice for a very long time, disc herniation in the lower spine has been the leading surgical technique for the past decades.
Lumbar radiculopathy or sciatica commonly results from disc herniation in the lower spine. The spinal cord consists of a mesh of spinal nerve roots in the lower spine below the L1/L2 level known as cauda equina. The nerve roots exit at each level to join other spinal nerve roots and form nerves/plexus that supply different regions in the lower extremities.
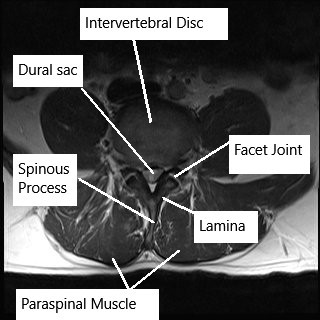
MRI of the lumbar spine in axial section.
The spinal nerve roots in the cauda equina are responsible for the sensations in the lower extremities and the genital region. The nerves also help in the movement of the lower extremities by supplying all the muscles in the legs. The nerve roots also help control bowel and bladder control.
The intervertebral discs are located in between the consecutive vertebrae, and the spinal nerves are contained inside a dural sac. The dural sac lies inside the central canal formed by the vertebrae, and the lamina forms the roof of the central canal. The exiting nerve roots are contained inside the intervertebral foramen.
The intervertebral disc may herniate as a result of trauma or repetitive motion. The disc also undergoes age-related wear and tear along with the formation of bone spurs by the vertebral bodies. The bulging or the herniation of the intervertebral discs leads to the narrowing of the precarious space available for the nerve roots/dural sac. The compression leads to inflammation, and patients usually complain of back pain that may radiate to the thighs and the legs.
After the establishment of the diagnosis of lumbar radiculopathy, conservative management is tried initially. The physician may prescribe the pain medications, advise activity modification, along heat/cold therapy to reduce inflammation and aid in recovery. After the initial few days, physical therapy may be started to increase the flexibility and improve the strength of the muscles of the back.
Epidural injections may be tried in patients who do not get better with conservative management. Surgical management in the form of discectomy is usually the gold standard when all other forms of management have been tried and failed.
Surgical Procedures
Open Discectomy (OD)
- Procedure: Involves a midline skin incision, retraction of paravertebral tissues, partial laminectomy, and removal of the ligamentum flavum to expose the spinal cord and nerve roots. The disc material is then removed, and the posterior longitudinal ligament is opened.
- Duration: Significantly shorter operation time (37.82±7.15 minutes).
Microdiscectomy (MD)
- Procedure: Utilizes a microscope for better visualization, with minimal laminectomy and removal of the ligamentum flavum. The nerve root is retracted medially, and the disc contents are removed.
- Duration: Longer operation time (49.07±6.88 minutes).
Results and Clinical Outcomes
Similarities
- No significant differences in postoperative clinical outcomes, complications, or reoperation rates.
- Both methods showed similar long-term outcomes in terms of pain relief and functional recovery.
Differences
- OD had a shorter operation time but involved more tissue manipulation.
- MD resulted in less blood loss, less postoperative pain, and quicker mobilization due to the minimally invasive nature.
Complications and Reoperations
- OD: 6.9% reoperation rate, 1.4% dural tears, 2.9% wound infections.
- MD: 9.5% reoperation rate, 3.3% dural tears, 3.3% wound infections.
- No significant differences in overall complication rates, suggesting both techniques are comparably safe when performed by experienced surgeons.
During an open discectomy, the patient lies on their stomach under general anesthesia. The surgeon identifies the level of surgery using an image intensifier. A midline incision is given in the lower back. The surgeon separates the paraspinal muscles to reach the ligamentum flavum.
A small part of the lamina is cut and the ligamentum flavum to removed to expose the nerve roots and the intervertebral disc. The nerve roots are carefully retracted towards the midline, and the surgeon removes the herniated disc under direct vision.
The bone spurs may also be removed, and the canal may also be widened during the surgery. The surgeon closes the incision in layers. Patients after open discectomy may stay in the hospital overnight for observation or may go home the same day of the surgery.
In microdiscectomy, the operating surgeon uses a magnifying endoscope/microscope to visualize the surgical field. The incision in the midline of the lower back is small as compared to the open discectomy. The incision is usually just about 1.5 inches or smaller. The surgeon separates the tissues to reach the lamina.
The magnifying microscope allows better visualization of the tissue surrounding the nerve roots and a gentle retraction of the spinal nerves. The microscope also helps in better removal of the herniated disc material.
After the removal of the compression, the surgeon closes the small incision in layers and applies a small tape over the incision site. The surgery utilizing a smaller incision; the majority of the patients are able to go home the same day of the procedure. Microdiscectomy may also be performed in an outpatient setting under local anesthesia.
The minimally invasive approach of microdiscectomy leads to less tissue damage, less blood loss, and fewer cases of postoperative infection of the surgical site. Patients treated with microdiscectomy can return to work early due to early mobilization, shorter hospital stays, and quicker rehabilitation.
Similarly, due to minimum trauma to the muscles during the surgical approach, the patients experience less back pain and subsequently need fewer pain medications postop. Microdiscectomy is also associated with fewer complications such as a dural tear, nerve root injury due to the use of the microscope, and better visualization of the surgical field.
Both open discectomy and microdiscectomy are highly successful surgeries for treating lumbar radiculopathy. The choice of surgery is mainly dependent upon surgeon experience and the underlying condition of the patient. While the ultimate goal is similar, microdiscectomy has primarily replaced open discectomies in the past decade. Discuss both the surgical options with your surgeon before undergoing management for sciatica or lumbar radiculopathy.
Conclusion
Both open discectomy and microdiscectomy are effective surgical techniques for treating lumbar disc herniation. While OD has a shorter operation time, MD offers the benefits of being minimally invasive, resulting in less postoperative pain and faster recovery. The choice of surgical method should consider the surgeon’s experience, the specific clinical scenario, and patient preferences. Ongoing advancements in endoscopic technologies promise further improvements in surgical outcomes for patients with LDH.
Do you have more questions?
What are the primary symptoms of LDH?
The primary symptoms include lower back pain, radiating leg pain (sciatica), numbness, tingling, and muscle weakness in the legs.
What is lumbar disc herniation (LDH)?
Lumbar disc herniation occurs when the inner gel-like core of a lumbar disc protrudes through its outer layer, compressing nearby nerves. This leads to symptoms like lower back pain, sciatica, and neurological deficits.
What is open discectomy (OD)?
Open discectomy is a surgical procedure where a larger incision is made to remove the herniated disc material. It involves direct visualization and access to the spinal structures.
How is LDH diagnosed?
LDH is diagnosed using imaging techniques such as magnetic resonance imaging (MRI), computed tomography (CT) scans, and X-rays, combined with a clinical examination of symptoms and medical history.
What is microdiscectomy (MD)?
Microdiscectomy is a minimally invasive surgical technique using a microscope to provide a clearer view of the surgical area. It involves smaller incisions and less tissue disruption compared to OD.
What are the advantages of MD over OD?
MD results in less tissue damage, reduced postoperative pain, quicker recovery, and a shorter hospital stay due to its minimally invasive nature.
What are the risks associated with OD?
Risks of OD include dural tears, wound infections, nerve root injuries, and reoperation due to recurrent herniation.
How do the operation times compare between OD and MD?
The operation time for OD is generally shorter (37.82±7.15 minutes) compared to MD (49.07±6.88 minutes).
What are the risks associated with MD?
Risks of MD include dural tears, wound infections, nerve root injuries, and slightly higher chances of reoperation due to recurrent herniation compared to OD.
Is there a significant difference in long-term outcomes between OD and MD?
No significant differences in long-term outcomes, including pain relief and functional recovery, have been observed between OD and MD.
Which surgical method has a higher reoperation rate?
MD has a slightly higher reoperation rate (9.5%) compared to OD (6.9%), though the difference is not statistically significant.
What is the postoperative recovery like for patients undergoing MD?
Patients undergoing MD typically experience less postoperative pain, faster mobilization, and shorter hospital stays due to the minimally invasive nature of the procedure.
How does the postoperative recovery compare between OD and MD?
MD generally offers a quicker postoperative recovery with less pain and shorter hospital stays compared to OD.
Are there any specific conditions where one method is preferred over the other?
MD is often preferred for patients who require a minimally invasive approach due to less tissue disruption, while OD may be preferred for surgeons with more experience in open procedures or in cases where direct visualization is necessary.
What is the role of endoscopic technology in spinal surgeries?
Endoscopic technology allows for minimally invasive procedures like microendoscopic discectomy (MED), offering a clearer surgical view, reduced trauma, and faster recovery.
What are the common complications of spinal surgeries like OD and MD?
Common complications include dural tears, nerve root injuries, wound infections, and reoperation due to recurrent herniation.
What measures are taken to minimize complications during these surgeries?
Surgeons use precise techniques, advanced imaging, and careful patient monitoring to minimize complications. Postoperative care includes antibiotics, pain management, and physical therapy.
How does patient age impact the outcomes of OD and MD?
While both methods are effective across different age groups, older patients might experience slightly higher reoperation rates. However, age alone does not significantly impact overall surgical outcomes.
What is the significance of the learning curve in MD?
The learning curve for MD can be longer due to the need for proficiency with microscopic techniques, but experienced surgeons can perform it effectively with excellent outcomes.
How does the size of the incision differ between OD and MD?
OD typically involves a larger incision compared to the smaller, minimally invasive incisions used in MD.
What postoperative care is required for patients undergoing OD or MD?
Postoperative care includes pain management, wound care, antibiotics to prevent infections, and physical therapy to aid in recovery and restore function.
Can both OD and MD be performed on all levels of the lumbar spine?
Yes, both OD and MD can be performed on various levels of the lumbar spine, though the choice of method may depend on the specific location and severity of the herniation.
What factors influence the choice between OD and MD?
Factors include the surgeon’s experience, the specific characteristics of the herniation, patient preferences, and the presence of any contraindications for minimally invasive surgery.
How does the surgical experience of the surgeon affect the outcomes of OD and MD?
Surgical experience is crucial in determining outcomes. Experienced surgeons can achieve excellent results with both OD and MD, minimizing complications and improving recovery times.
What future advancements are expected in the treatment of LDH?
Future advancements may include improved endoscopic techniques, robotic-assisted surgeries, and enhanced imaging technologies to further reduce invasiveness, improve precision, and enhance patient outcomes.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
