Core Decompression for Avascular Necrosis of the Hip
Core decompression is a surgical procedure used in the management of the early stages of the avascular necrosis of the head of the femur. The avascular necrosis is also known as osteonecrosis, is a disease caused by disruption of the blood supply to the involved bone. The disruption of the blood supply may lead to bone death or necrosis.
The upper end of the thigh bone forms the ball of the hip joint. The ball known as the head of the femur has a precarious blood supply. Various mechanisms may lead to the disruption of the blood supply. Corticosteroids and alcoholism are the top causes of non-traumatic avascular necrosis of the head of the femur.
Blood supply is vital to maintain the normal surface and structure of the hip joint. Traumatic or nontraumatic causes may lead to a decreased or absent blood supply to parts of the head of the femur. With an absent blood supply, the segment of bone becomes nonviable.
The surrounding bone with blood supply tries to revascularize the dead bone. Vascular tissue lays down new bone in the area which increases the density (visible as increased whiteness in an X-ray.) A small fracture or break may develop between the new bone and the dead bone.
The space in between the break is filled by scar tissue. Overlying cartilage without nourishment softens and decays. The weight bore on the joint leads to small dents or breaks in the cartilage leading to collapse.
The smooth gliding is now lost and the ball grinds with the socket in the area. The process becomes widespread leading to severe arthritis and destruction of the joint surface.
In the early stages (stage 1 and 2 of Ficat & Arlet staging) of avascular necrosis, the surface of the ball and socket joint is smooth. There are no changes visible on an X-ray but changes appear on an MRI or a bone scan. The patients with early stages (pre-collapse) may benefit from core decompression.
In the early stages of osteonecrosis, the pressure inside in the head of the femur is vastly increased. The elevated pressure hampers the revascularisation of dying bone. The increased pressure also further decreases the blood of the head of the femur.
The procedure involves the creation of a small tunnel/tunnels in the head of the femur to slow or stop the osteonecrosis. The patient is laid on the operating table and the leg is placed in a specially designed table for positioning.
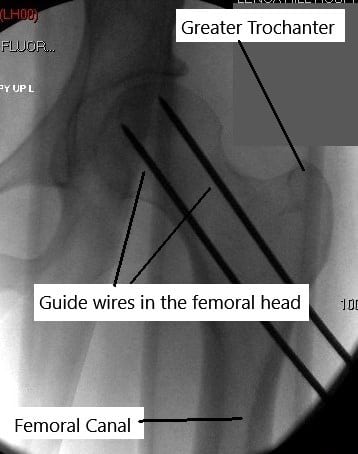
An intraoperative X-ray known as C-arm is used for checking the position of the instruments during the surgery. The patient may be given an intravenous sedative, spinal anesthesia, or general anesthesia. A small incision is given on the outer side of the upper thigh.
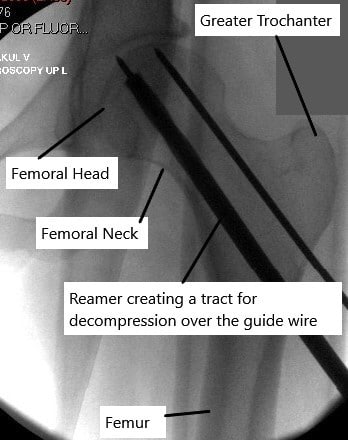
A small guide wire is passed from the incision to reach the area of the avascular necrosis without breaching the articular cartilage. A small drilling instrument is passed over the guidewire to create a tunnel to the dead bone. The procedure may involve the use of multiple drill holes instead of a single hole.
Usually, bone marrow is injected through the hole in the area of the dead bone. Sometimes bone graft taken from the patient’s body or from a bone bank may be used to fill the tunnel. The incision is closed with a suture and sterile dressing is placed on the site. The creation of a tunnel/tunnels decreases the pressure inside the head of the femur.
The reduction of pressure may lead to revascularisation and therefore repair the area of nonviable bone. The addition of bone marrow or bone graft may provide stem cells which may lead to early repair of the dead bone.
The patients are usually able to go home the same day of the procedure. The patients are usually instructed to bear 50% of the weight on the side of the procedure for the next 3 months. The patients are also instructed to avoid high impact activities.
The patients are usually followed up every 6 months to monitor the progression of osteonecrosis. In the majority of the patients, the disease process slows down or comes to a stop. They may have radiological evidence of repair of the necrotic bone.
Unfortunately, the disease process may progress in some patients. The progress is however slowed down after core decompression. The progressed cases of avascular necrosis and those in advanced stages usually require joint replacement surgery.
A total hip replacement provides excellent relief from pain and the patients are quickly able to get back to the activities they enjoy. The joint replacement surgery has revolutionized the treatment of advanced cases of avascular necrosis of the head of the femur.
Do you have more questions?
Are there any alternative or complementary therapies that patients can explore alongside traditional medical treatments for avascular necrosis of the hip?
What steps can patients take to optimize their recovery and improve the success of core decompression surgery?
Following post-operative instructions, maintaining a healthy lifestyle, attending physical therapy sessions, and attending follow-up appointments are essential for optimal recovery.
Is avascular necrosis of the hip more prevalent in certain demographic groups or populations with specific genetic predispositions?
Certain genetic factors may predispose individuals to avascular necrosis, but the condition can occur in people of all demographics.
What are the typical costs associated with core decompression surgery, and does insurance typically cover the procedure?
Costs can vary depending on factors such as hospital fees, surgeon fees, and post-operative care, and insurance coverage may vary based on individual policies.
Are there any occupational or lifestyle modifications that patients should consider after undergoing core decompression surgery?
Depending on their occupation and activities, patients may need to avoid high-impact or strenuous activities to protect the hip joint and aid in recovery.
How often should patients undergo follow-up imaging or clinical evaluations after core decompression surgery to monitor disease progression?
Follow-up frequency may vary but is typically every few months initially, then less frequently if the disease remains stable.
What are the potential complications associated with long-term use of medications to manage avascular necrosis symptoms, such as nonsteroidal anti-inflammatory drugs (NSAIDs)?
Long-term NSAID use may increase the risk of gastrointestinal bleeding, kidney damage, and cardiovascular events, so careful monitoring is necessary.
Are there any emerging treatments or research advancements in the field of avascular necrosis that patients should be aware of?
Research into new treatment modalities, such as stem cell therapy or biologic agents, is ongoing, but further studies are needed to assess their efficacy and safety.
How does avascular necrosis of the hip affect a patient’s quality of life, particularly in terms of mobility and pain management?
Avascular necrosis can significantly impact mobility and cause chronic pain, affecting daily activities and overall quality of life.
Are there any specific rehabilitation exercises or physical therapy regimens recommended after core decompression surgery?
Yes, physical therapy plays a crucial role in recovery and may include exercises to improve hip strength, flexibility, and range of motion.
What are the long-term outcomes of core decompression surgery compared to other surgical interventions, such as total hip replacement?
Long-term outcomes can vary, but core decompression may delay or avoid the need for hip replacement in some patients, while others may eventually require joint replacement.
Can core decompression surgery be performed bilaterally (on both hips) simultaneously, or is it typically done one hip at a time?
Bilateral core decompression surgery can be performed in select cases, but the decision depends on factors such as the patient’s overall health and surgical risk.
What are the factors that determine whether a patient is a suitable candidate for core decompression surgery?
Factors such as the stage of avascular necrosis, the extent of bone damage, overall health, and lifestyle factors are considered when determining candidacy for core decompression.
Are there any dietary or nutritional recommendations that can support bone health and potentially reduce the risk of avascular necrosis recurrence?
Maintaining a balanced diet rich in calcium and vitamin D may support bone health, but specific dietary recommendations may vary based on individual factors.
Is core decompression surgery appropriate for all patients with avascular necrosis of the hip, regardless of disease stage?
Core decompression is typically recommended for early-stage avascular necrosis, and its effectiveness may diminish as the disease progresses.
Can avascular necrosis of the hip be managed with non-surgical treatments alone?
In early stages, non-surgical treatments such as medication, physical therapy, and lifestyle modifications may help manage symptoms.
How does core decompression surgery differ from other treatment options for avascular necrosis?
Core decompression involves creating tunnels in the femoral head to relieve pressure and stimulate bone repair, whereas other options may include medication or joint replacement.
What are the success rates of core decompression surgery in preventing the progression of avascular necrosis?
Success rates vary depending on the stage of the disease and individual factors, but early intervention with core decompression can significantly slow or halt disease progression.
How long does it typically take to recover from core decompression surgery?
Recovery can vary, but patients typically begin weight-bearing activities within a few weeks and may return to normal activities within a few months.
What are the success rates of core decompression surgery in preventing the progression of avascular necrosis?
Success rates vary depending on the stage of the disease and individual factors, but early intervention with core decompression can significantly slow or halt disease progression.
How long does it typically take to recover from core decompression surgery?
Recovery can vary, but patients typically begin weight-bearing activities within a few weeks and may return to normal activities within a few months.
Are there any potential complications associated with core decompression surgery?
Complications are rare but can include infection, bleeding, or failure to relieve symptoms if the disease is advanced.
What imaging tests are used to diagnose avascular necrosis of the hip?
X-rays, MRI scans, and bone scans are commonly used to diagnose avascular necrosis and assess the extent of bone damage.
What are the limitations of core decompression surgery in treating advanced stages of avascular necrosis?
Core decompression may be less effective in advanced stages when significant bone collapse has occurred, and joint replacement surgery may be necessary.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
