Role of Fibular Bone Graft in the
Treatment of Avascular Necrosis
Avascular necrosis (AVN), also known as osteonecrosis, is a debilitating condition that affects the femoral head, leading to bone death due to compromised blood supply. It is most common in young and middle-aged adults, often causing pain, deformity, and limp. Fibular bone grafting is one of the preservation techniques used in the early stages of AVN to delay the need for total hip replacement (THR). Though THR is often recommended in late-stage AVN, fibular grafts provide an option to preserve the femoral head in select patients, especially those who are younger and wish to avoid or delay joint replacement surgery.
Functional Anatomy
The hip joint is a ball-and-socket joint formed by the femoral head (ball) and the acetabulum (socket) in the pelvis. The femoral head is supported by a delicate vascular network that provides essential nutrients to the bone. Avascular necrosis occurs when the blood supply to the femoral head is disrupted, often leading to bone collapse and severe arthritis if untreated. Fibular bone grafting aims to provide structural support and nutritional restoration to the affected bone, potentially slowing the progression of AVN and avoiding the collapse of the femoral head.

MRI in the coronal section showing avascular necrosis lesions in both hips.
Biomechanics or Physiology
In AVN, the loss of blood supply to the femoral head leads to bone death and the collapse of the femoral head. This collapse causes mechanical failure in the hip joint, resulting in pain, stiffness, and functional limitations. Fibular bone grafting works by addressing the bone collapse and restoring blood flow to the affected area. The fibula, a bone from the lower leg, is harvested and inserted into the femoral head to provide structural support and a vascular supply that can promote bone regeneration. The fibula’s bone cells gradually replace the necrotic bone through a process known as creeping substitution, wherein the graft tissue is replaced by new, healthy bone over time.
Common Variants and Anomalies
-
Early-stage AVN: When detected early, fibular bone grafting may prevent femoral head collapse and delay the need for total hip replacement.
-
Late-stage AVN: If the bone collapse is severe or if there is significant joint damage, total hip replacement is usually indicated.
-
Vascularized fibular grafting: This technique involves transferring fibular bone along with its blood vessels, ensuring an enhanced blood supply to the femoral head and improving the chances of bone regeneration.
-
Non-vascularized grafts are less effective in restoring bone health and may only provide structural support.
Clinical Relevance
Fibular bone grafting is a valuable treatment option for young patients with early-stage AVN who wish to avoid immediate joint replacement. It can help preserve the femoral head, delay the need for total hip replacement, and potentially restore normal hip function. However, the success of this procedure is not guaranteed, and AVN may progress despite intervention. This highlights the importance of careful patient selection, as well as the consideration of implant replacement surgery as a long-term solution, especially when conservative options fail.
Imaging Overview
-
X-rays: The primary imaging modality used to assess the femoral head for signs of AVN. Subchondral sclerosis (hardening of the bone) and joint space narrowing are indicative of advanced AVN.
-
MRI: The most sensitive test for detecting early-stage AVN. MRI can identify bone marrow edema (swelling) in the femoral head, which is often the first sign of AVN before bone collapse occurs.
-
CT scans: Used to visualize bone collapse and evaluate the extent of damage to the femoral head.
-
Bone scans: Can detect early changes in bone metabolism, such as increased uptake in the femoral head, indicating AVN.
Associated Conditions
-
Corticosteroid use: Long-term use of glucocorticoids for conditions such as rheumatoid arthritis, systemic lupus erythematosus, or nephrotic syndrome is a major risk factor for developing AVN.
-
Trauma: Hip fractures or dislocations can damage blood vessels supplying the femoral head, leading to AVN.
-
Alcohol abuse: Chronic alcohol consumption can disrupt blood flow to the femoral head, increasing the risk of AVN.
-
Other systemic diseases: Sickle cell disease and vascular disorders can also contribute to AVN by impairing blood supply to the hip.
Surgical or Diagnostic Applications
-
Core decompression: A procedure in which a small section of the femoral head is removed to reduce internal pressure and stimulate revascularization.
-
Fibular bone grafting: A non-surgical approach in which the fibula is harvested and implanted into the femoral head. The vascularized fibular graft enhances blood supply to the necrotic bone, encouraging healing.
-
Total hip replacement (THR): The most common treatment for late-stage AVN or advanced bone collapse, where the femoral head is replaced with an artificial joint.
-
Stem cell therapy: An experimental treatment option aimed at regenerating bone tissue using stem cells derived from the patient’s own body.
Prevention and Maintenance
While AVN cannot always be prevented, certain steps may reduce the risk:
-
Minimizing corticosteroid use whenever possible or using the lowest effective dose for the shortest period.
-
Maintaining bone health through calcium, vitamin D, and weight-bearing exercises.
-
Regular monitoring of patients on corticosteroid therapy for early signs of AVN.
-
Early diagnosis through MRI or bone scans allows for prompt intervention before femoral head collapse occurs.
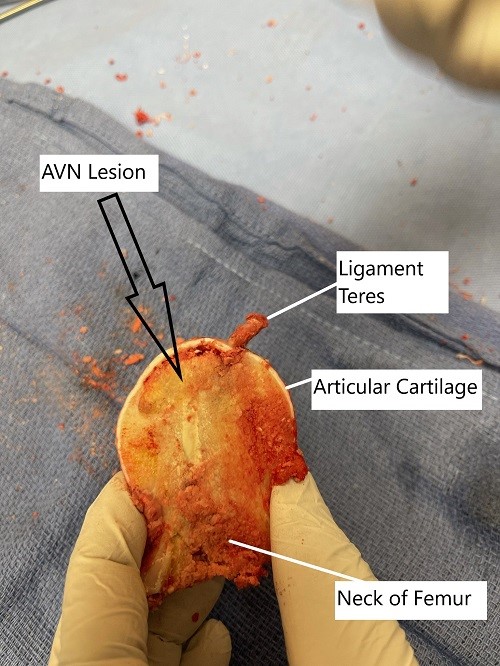
Removed head of femur during surgery showing avascular necrotic lesion.
Research Spotlight
A recent study assessed the outcomes of core decompression (CD) with or without nonvascularized fibular grafting in early-stage avascular necrosis (AVN) of the femoral head. The study included 76 hips, with Stage 1 patients undergoing CD alone and Stage 2 patients receiving CD with fibular grafting.
At an average follow-up of 53.5 months, the study found that 72.3% of hips showed no progression of the disease. However, 27.6% of cases demonstrated disease progression, with a higher failure rate in the fibular grafting group (30%) compared to CD alone (25%).
The study concluded that while CD with fibular grafting can delay disease progression and help preserve the femoral head, it does not entirely prevent further collapse or arthritis, emphasizing the importance of early intervention in the disease’s progression. (“Study on core decompression and fibular grafting for AVN – see PubMed“).
Summary and Key Takeaways
-
Avascular necrosis (AVN) of the femoral head is a progressive condition that can lead to pain and loss of joint function if untreated.
-
Corticosteroid use is the most common cause of AVN, particularly in young, middle-aged adults.
-
Early-stage AVN can be managed with core decompression, fibular bone grafting, and stem cell therapy, potentially delaying the need for total hip replacement.
-
Total hip replacement is the gold standard for advanced AVN, providing excellent pain relief and joint function.
-
Early diagnosis through MRI and bone scans is crucial for preserving the femoral head and preventing further joint damage.
Do you have more questions?
How does the experience and expertise of the surgeon impact the outcomes of fibular bone graft surgery for avascular necrosis of the hip?
The experience and expertise of the surgeon play a crucial role in the outcomes of fibular bone graft surgery for avascular necrosis of the hip, with skilled surgeons often achieving better results in terms of graft integration, joint preservation, and patient satisfaction.
Can fibular bone graft surgery be performed using minimally invasive techniques, and what are the potential benefits of such approaches?
Yes, fibular bone graft surgery can be performed using minimally invasive techniques, which may offer advantages such as smaller incisions, reduced blood loss, faster recovery times, and less postoperative pain compared to traditional open surgery.
How does the age of the patient impact the decision-making process for fibular bone graft surgery for avascular necrosis of the hip?
The age of the patient is an important consideration in the decision-making process for fibular bone graft surgery for avascular necrosis of the hip, with younger patients often being more suitable candidates due to their potential for better bone healing and longer-term outcomes.
Can fibular bone graft surgery be performed in patients with bilateral avascular necrosis of the hip, and if so, what are the potential challenges or considerations?
Fibular bone graft surgery can be performed in patients with bilateral avascular necrosis of the hip, but it may pose additional challenges such as longer recovery times, increased risk of complications, and the need for staged procedures to address both hips.
How does the success rate of fibular bone graft surgery for avascular necrosis of the hip compare to other treatment options available?
The success rate of fibular bone graft surgery for avascular necrosis of the hip varies depending on factors such as disease severity, patient characteristics, and surgical technique. Comparative studies may help determine the effectiveness of fibular bone graft surgery relative to other treatment modalities.
Are there any long-term complications or considerations associated with fibular bone graft surgery for avascular necrosis of the hip that patients should be aware of?
Long-term complications of fibular bone graft surgery for avascular necrosis of the hip may include graft failure, nonunion, arthritis, or progression of avascular necrosis in other areas of the hip joint. Regular follow-up with a healthcare provider is essential to monitor for potential complications.
How does the location and size of the avascular necrosis lesion in the hip joint influence the decision to perform fibular bone graft surgery?
The location and size of the avascular necrosis lesion in the hip joint may influence the decision to perform fibular bone graft surgery, with larger or more centrally located lesions often warranting more extensive surgical intervention.
What imaging studies are used to assess the success of fibular bone graft surgery for avascular necrosis of the hip, and how often are they performed postoperatively?
Imaging studies such as X-rays, MRI, or CT scans may be used to assess the success of fibular bone graft surgery for avascular necrosis of the hip, with follow-up intervals determined by the surgeon based on individual patient factors and disease progression.
Are there any lifestyle modifications or precautions recommended after fibular bone graft surgery for avascular necrosis of the hip to prevent disease recurrence?
Yes, lifestyle modifications such as avoiding excessive weight-bearing activities, quitting smoking, moderating alcohol intake, and maintaining a healthy lifestyle may help reduce the risk of disease recurrence after fibular bone graft surgery for avascular necrosis of the hip.
What are the criteria used to determine if a patient is a suitable candidate for fibular bone graft surgery for avascular necrosis of the hip?
Candidates for fibular bone graft surgery for avascular necrosis of the hip are typically those with early to moderate-stage disease, intact joint integrity, and adequate bone stock to support the graft.
Can fibular bone graft surgery prevent further progression of avascular necrosis in the hip joint, or is it primarily aimed at relieving symptoms?
Fibular bone graft surgery aims to provide structural support to the hip joint, potentially preventing further collapse and preserving joint function. However, its ability to halt the progression of avascular necrosis depends on various factors and may not always be guaranteed.
How long does it typically take to recover from fibular bone graft surgery for avascular necrosis of the hip, and what is the rehabilitation process like?
Recovery from fibular bone graft surgery for avascular necrosis of the hip may take several months to a year, with initial weight-bearing restrictions followed by gradual rehabilitation exercises to restore strength, range of motion, and function.
Are there alternative treatments to fibular bone graft surgery for avascular necrosis of the hip, and how do they compare in terms of effectiveness?
Yes, alternative treatments for avascular necrosis of the hip include core decompression, vascularized bone grafting, osteotomy, and total hip replacement. The choice of treatment depends on factors such as disease severity, patient age, and surgeon preference.
How successful is fibular bone graft surgery in treating avascular necrosis of the hip, and what factors contribute to its success?
The success of fibular bone graft surgery in treating avascular necrosis of the hip depends on various factors, including the stage of the disease, the quality of the graft, surgical technique, patient factors, and postoperative rehabilitation.
Can fibular bone graft surgery be performed as a standalone procedure for avascular necrosis of the hip, or is it often combined with other treatments?
Fibular bone graft surgery can be performed as a standalone procedure for avascular necrosis of the hip, but it may also be combined with other treatments such as core decompression or total hip replacement, depending on the extent and severity of the disease.
How long does it take for a fibular bone graft to integrate and provide structural support in the hip joint?
The timeline for integration of a fibular bone graft into the hip joint varies but typically ranges from several months to a year, during which the graft gradually incorporates with the surrounding bone tissue.
What are the limitations or potential risks of fibular bone graft surgery for avascular necrosis of the hip?
Like any surgical procedure, fibular bone graft surgery for avascular necrosis of the hip carries potential risks such as infection, blood loss, nerve injury, and failure of the graft to integrate properly with the host bone.
Are there different stages of avascular necrosis, and how do they affect treatment options?
Yes, avascular necrosis progresses through stages ranging from early changes in blood supply to advanced collapse of the bone. Treatment options may vary depending on the stage of the disease.
How does avascular necrosis affect the blood supply to the hip joint?
Avascular necrosis disrupts the blood supply to the hip joint, leading to inadequate oxygen and nutrients reaching the bone tissue, which ultimately results in bone cell death and tissue damage.
What is the typical progression of avascular necrosis if left untreated?
If left untreated, avascular necrosis of the hip can progress through stages characterized by increasing bone damage, collapse of the femoral head, degenerative changes in the hip joint, and eventual joint dysfunction.
Can avascular necrosis of the hip progress without treatment?
Yes, avascular necrosis of the hip can progress without treatment, potentially leading to further bone damage, collapse of the hip joint, and severe pain or disability.
Are there any risk factors associated with avascular necrosis of the hip?
Yes, several risk factors can predispose individuals to avascular necrosis of the hip, including trauma, corticosteroid use, excessive alcohol consumption, certain medical conditions like sickle cell disease, and joint diseases such as rheumatoid arthritis.
How common is avascular necrosis of the hip?
Avascular necrosis of the hip can occur in various conditions but is relatively rare. It may affect individuals of any age but is more commonly seen in middle-aged adults.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://www.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
