Due to the evolution and the success of a total hip replacement in the past decades, partial hip replacement is performed in a very small subset of patients. Partial hip replacement involves the prosthetic replacement of the femoral head with a prosthetic stem and head. The socket of the hip joint formed by the acetabulum is not replaced in partial hip replacement.
Candidates for Partial Hip Replacement
Partial hip replacement is mostly performed in elderly patients with multiple diseases and limited mobility. The surgical time of partial hip replacement is shorter with less blood loss as compared to a total hip replacement. The partial hip replacement surgery typically lasts just about an hour. As the surgery time is shorter, the complications associated with a major surgery such as hip replacement may be decreased.
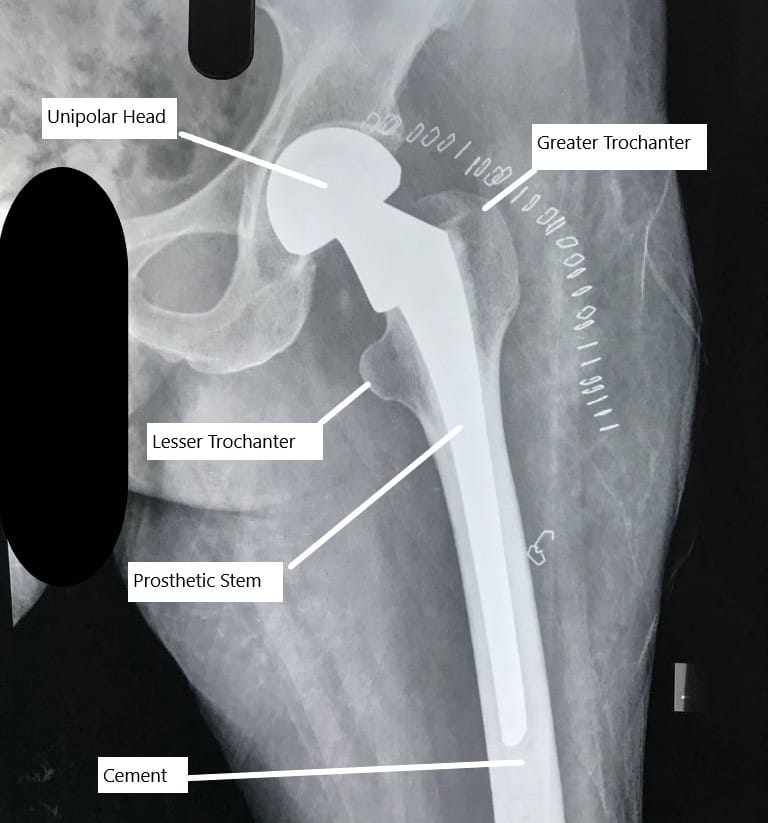
Partial unipolar hip replacement X -ray
Partial hip replacement is also offered to patients who have limited mobility. During partial hip replacement, a larger prosthetic head of femur is used. The large size of the head provides greater stability to the prosthetic joint. A large prosthetic head requires a greater motion before it can pop out of the socket.
A partial hip replacement is also offered sometimes for patients with fractures of the neck of the femur. The neck of the femur not only connects the ball shaped head to the upper thigh bone but also carries vital blood supply to the head. The fracture of the neck disrupts the precarious blood supply and may lead to bone death of the head of the femur.
These patients may require a hip replacement surgery and if the socket does not show any arthritic changes, a partial hip replacement may be offered to these patients.
Types of Partial Hip Replacement
Unipolar and bipolar are two types of partial hip replacement. The unipolar replacement is rarely performed and most of the partial hip replacement surgeries are bipolar. In a bipolar hip replacement, the prosthetic head of the femur actually consists of two balls. A smaller metallic ball rotates inside the larger metallic ball. A high grade polyethylene plastic covers the inner metal ball to provide a smooth rotating surface.
Compared to bipolar, a unipolar partial hip replacement only consists of a head firmly attached to the stem of the prosthesis. The bipolar design provides greater stability, movement and also helps protect the articular cartilage. The ball in ball design mimics the socket of the total hip replacement.
Procedure
Similar to total hip replacement, a partial hip replacement may be performed under general anesthesia or spinal anesthesia. The surgeon may access the joint from the more commonly used posterior approach. The surgeon may also utilize robotic techniques or use minimally invasive techniques.
After a skin incision the surgeon reaches the joint after cutting or separation of the various tissues. The surgeon then removes the diseased head of the femur. The acetabulum is not reamed or prepared in partial hip replacement.
The surgeon proceeds to ream and prepare the femoral canal. The canal is prepared by serial introduction of special instruments known as broaches. Special attention is paid to the angle of the preparation. After a trial, the final prosthesis is introduced. The prosthesis may be press fitted or may be cemented in the femoral canal.
A bipolar prosthetic head is then placed on the prosthetic stem. The head is introduced back in the socket using a maneuver. The implant is again assessed for stability, movement and leg length. The incision is closed in layers and the patient is shifted to the recovery area.
The patients are placed on deep vein thrombosis prophylaxis and are up and able to walk with support the next day of the surgery. As surgery time is shorter than the total hip replacement, the recovery is accelerated.
Total Hip Replacement benefits over Partial Hip Replacement
Partial hip replacement has fallen out of favor to a total hip replacement and only a very small number of patients in the US receive a partial hip replacement. The hip joint is a large ball and socket joint. The socket is formed by the acetabulum, a part of the pelvic bone.
Both the head of the femur (ball) and the acetabulum (socket) are covered with a protective tissue known as articular cartilage. The articular cartilage functions to lubricate the motion of the opposing bones. Arthritis of the hip joint leads to damage of the articular cartilage of the ball as well as the socket.
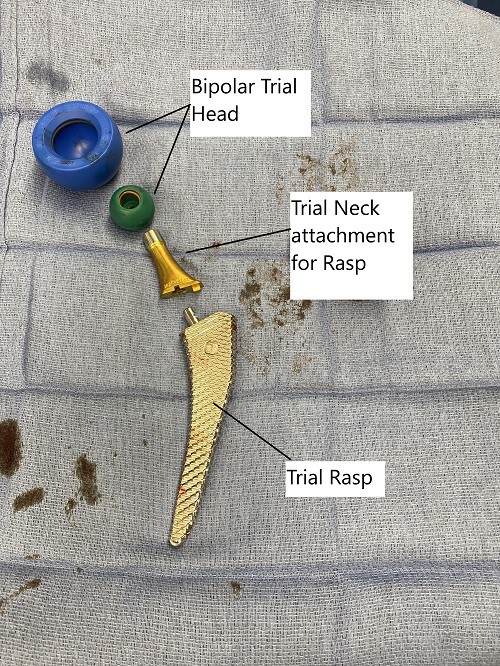
Intraoperative image of total hip replacement
Replacement of only the ball of the joint as in the case of a partial hip replacement leads to stress over the natural articular cartilage of the socket. The artificial surface of the prosthetic head rubs against the socket cartilage leading to progressive pain.
The majority of the patients have an active lifestyle after hip replacement surgery, and continued stress and motion over the socket cartilage leads to it’s damage. Therefore partial hip replacement is not recommended in patients with active lifestyle.
A total hip replacement involves the replacement of both the ball and the socket of the hip joint. The artificial joint allows greater movement and reduction of pain. The patients can freely move and play sports they enjoy after a total hip replacement.
A total hip replacement today may last for 20 years or more and in some patients a lifetime. Owing to the success and longevity of the implant, total hip replacement has today replaced most of the partial hip replacements.
For Total Hip Replacement procedure and cost information, please click here.
How Medicare Covers Partial Hip Replacement
If you have Medicare, your healthcare provider may bill for CPT Code 27125 — this refers to a surgical procedure where only part of the hip joint (usually the ball portion of the femur) is replaced with an artificial implant, while the socket is left intact.
“What Will It Cost You?”
If you don’t have secondary insurance, here’s what you can expect:
Estimated Out-of-Pocket Cost for Partial Hip Replacement (27125): $268.14
“For example, George needed a partial hip replacement after breaking his hip in a fall. His surgery included 1 procedure: replacement of the ball portion of his hip joint with an artificial implant (27125). Thanks to Medicare, his total out-of-pocket cost was about $268.14. His secondary insurance then covered it completely!”
Do you have more questions?
What types of hip conditions or injuries are commonly treated with partial hip replacement?
Partial hip replacement is often used to treat conditions such as femoral neck fractures, avascular necrosis of the femoral head, and certain types of hip arthritis affecting primarily the femoral head.
What are the disadvantages of partial hip replacement compared to total hip replacement?
Disadvantages of partial hip replacement may include a higher risk of needing revision surgery in the future if arthritis progresses, limited durability of the prosthetic femoral head, and potential challenges in achieving optimal alignment and stability.
What are the advantages of partial hip replacement compared to total hip replacement?
Partial hip replacement may offer advantages such as preservation of bone and soft tissue, potentially faster recovery, reduced risk of dislocation, and a more conservative surgical approach for certain patients.
How do surgeons determine whether a patient is a candidate for partial hip replacement versus total hip replacement?
Surgeons consider factors such as the extent of hip joint damage, the patient’s age, activity level, bone quality, and overall health when determining the most appropriate type of hip replacement surgery.
What is the main difference between partial hip replacement and total hip replacement?
Partial hip replacement involves replacing only the damaged portion of the hip joint, typically the femoral head, while preserving the acetabulum. Total hip replacement involves replacing both the femoral head and the acetabulum with prosthetic components.
How does the risk of post-operative complications differ between partial hip replacement and total hip replacement?
Partial hip replacement may be associated with a lower risk of certain post-operative complications such as dislocation and nerve injury compared to total hip replacement, as the surgery involves preserving more of the native hip anatomy and soft tissues. However, the overall risk of complications depends on various factors including patient-specific factors and surgical technique.
Are there any restrictions on driving or returning to work after partial hip replacement surgery?
Patients are typically advised to refrain from driving for a few weeks after partial hip replacement surgery until they are no longer taking narcotic pain medications and have regained sufficient mobility and strength. Returning to work will depend on the patient’s occupation and the type of activities involved, with most individuals able to resume sedentary or light-duty work within a few weeks to months after surgery.
How does the risk of periprosthetic fracture differ between partial hip replacement and total hip replacement?
Partial hip replacement may be associated with a lower risk of periprosthetic fracture compared to total hip replacement, as the surgery involves preserving more of the native hip anatomy and bone stock. However, certain patient factors such as osteoporosis and implant-related factors can influence the risk of periprosthetic fracture in both procedures.
Can partial hip replacement be performed using computer-assisted navigation techniques?
Yes, partial hip replacement surgery can be performed using computer-assisted navigation techniques, which offer potential benefits such as improved accuracy in implant placement, enhanced surgical precision, and better patient outcomes. Computer-assisted navigation may be particularly useful in complex cases or for achieving optimal component alignment.
How does the risk of post-operative stiffness differ between partial hip replacement and total hip replacement?
Partial hip replacement may be associated with a lower risk of post-operative stiffness compared to total hip replacement, as the surgery involves preserving more of the native hip anatomy and soft tissues. However, individual patient factors and surgical technique can influence the risk of stiffness in both procedures.
How does the choice between partial hip replacement and total hip replacement affect the risk of future revision surgery?
The choice between partial hip replacement and total hip replacement may impact the risk of future revision surgery, as partial hip replacement preserves more of the native hip anatomy and bone stock. However, factors such as implant wear, progression of arthritis, and patient-specific factors can influence the need for revision surgery over time.
What are the key factors to consider when deciding between partial hip replacement and total hip replacement?
Key factors to consider when deciding between partial hip replacement and total hip replacement include the extent of hip joint damage, the patient’s age and activity level, bone quality, overall health, surgical preferences, and the expected long-term outcomes of each procedure.
How does the recovery process differ between partial hip replacement and total hip replacement?
The recovery process may differ in terms of post-operative pain, rehabilitation duration, and return to normal activities. Partial hip replacement patients may experience a shorter recovery period and less post-operative pain compared to total hip replacement patients due to the less extensive nature of the surgery.
Are there specific exercises or physical therapy regimens recommended after partial hip replacement surgery?
Yes, patients typically undergo physical therapy after partial hip replacement surgery to improve hip strength, flexibility, and range of motion. Specific exercises may include gentle stretching, strengthening exercises, and mobility exercises tailored to the individual’s needs and limitations.
How does the risk of infection compare between partial hip replacement and total hip replacement?
Both partial and total hip replacement surgeries carry a risk of infection, but the risk may be slightly lower with partial hip replacement due to the smaller incision size and less extensive surgical exposure. However, infection risk can be minimized through strict adherence to sterile surgical techniques and antibiotic prophylaxis.
Can partial hip replacement be performed using robotic-assisted techniques?
Yes, robotic-assisted partial hip replacement procedures are available and offer potential benefits such as improved accuracy in implant placement, enhanced surgical precision, and better patient outcomes. However, not all surgeons may have access to or expertise in robotic technology for partial hip replacement.
What factors influence the choice between a cemented or uncemented prosthesis in partial hip replacement surgery?
Factors such as patient age, bone quality, surgeon preference, and implant design may influence the decision to use a cemented or uncemented prosthesis in partial hip replacement surgery. Cemented prostheses provide immediate fixation, while uncemented prostheses rely on bone ingrowth for stability.
How does the risk of leg length discrepancy differ between partial hip replacement and total hip replacement?
Partial hip replacement may carry a lower risk of leg length discrepancy compared to total hip replacement, as the surgery involves replacing only the damaged portion of the femoral head rather than altering the entire hip joint anatomy. However, careful pre-operative planning and surgical technique are essential to minimize this risk.
Are there specific dietary recommendations or supplements recommended after partial hip replacement surgery?
While there are no specific dietary restrictions following partial hip replacement surgery, maintaining a balanced diet rich in nutrients such as calcium and vitamin D can support bone health and facilitate the healing process. In some cases, healthcare providers may recommend calcium or vitamin D supplements to aid in bone healing.
How does the risk of implant wear and osteolysis compare between partial hip replacement and total hip replacement?
Partial hip replacement may be associated with a lower risk of implant wear and osteolysis compared to total hip replacement, as the surgery involves preserving more of the native hip anatomy and bone stock. However, long-term follow-up and monitoring are essential to detect any signs of implant-related complications.
Can partial hip replacement be performed using minimally invasive muscle-sparing techniques?
Yes, partial hip replacement can be performed using minimally invasive muscle-sparing techniques, which aim to minimize soft tissue damage, reduce post-operative pain, and accelerate recovery. These techniques typically involve smaller incisions and less disruption to surrounding muscles and tendons.
How does the risk of blood loss and the need for transfusion differ between partial hip replacement and total hip replacement?
Partial hip replacement may be associated with a lower risk of blood loss and the need for transfusion compared to total hip replacement, as the surgery involves a smaller incision and less extensive soft tissue dissection. However, individual patient factors and surgical techniques can influence blood loss and transfusion requirements.
What factors influence the choice between a metal-on-polyethylene or ceramic-on-ceramic bearing surface in partial hip replacement surgery?
Factors such as patient age, activity level, and surgeon preference may influence the choice between different bearing surface options in partial hip replacement surgery. Metal-on-polyethylene bearings are commonly used and offer durability and reliability, while ceramic-on-ceramic bearings may provide enhanced wear resistance and longevity.
Can partial hip replacement be performed as an outpatient procedure?
Yes, partial hip replacement surgery can be performed as an outpatient procedure in select patients who meet certain criteria, such as good overall health, minimal medical comorbidities, and a supportive home environment. Outpatient partial hip replacement allows patients to return home on the same day as surgery and may offer potential benefits such as reduced hospital costs and quicker recovery.
How does the risk of post-operative complications differ between partial hip replacement and total hip replacement?
Partial hip replacement may be associated with a lower risk of certain post-operative complications such as dislocation and nerve injury compared to total hip replacement, as the surgery involves preserving more of the native hip anatomy and soft tissues. However, the overall risk of complications depends on various factors including patient-specific factors and surgical technique.
Are there any restrictions on driving or returning to work after partial hip replacement surgery?
Patients are typically advised to refrain from driving for a few weeks after partial hip replacement surgery until they are no longer taking narcotic pain medications and have regained sufficient mobility and strength. Returning to work will depend on the patient’s occupation and the type of activities involved, with most individuals able to resume sedentary or light-duty work within a few weeks to months after surgery.
How does the risk of periprosthetic fracture differ between partial hip replacement and total hip replacement?
Partial hip replacement may be associated with a lower risk of periprosthetic fracture compared to total hip replacement, as the surgery involves preserving more of the native hip anatomy and bone stock. However, certain patient factors such as osteoporosis and implant-related factors can influence the risk of periprosthetic fracture in both procedures.
Can partial hip replacement be performed using computer-assisted navigation techniques?
Yes, partial hip replacement surgery can be performed using computer-assisted navigation techniques, which offer potential benefits such as improved accuracy in implant placement, enhanced surgical precision, and better patient outcomes. Computer-assisted navigation may be particularly useful in complex cases or for achieving optimal component alignment.
How does the risk of post-operative stiffness differ between partial hip replacement and total hip replacement?
Partial hip replacement may be associated with a lower risk of post-operative stiffness compared to total hip replacement, as the surgery involves preserving more of the native hip anatomy and soft tissues. However, individual patient factors and surgical technique can influence the risk of stiffness in both procedures.

