Hip Replacement Complications & Risks
Total hip replacement (THR) is one of the most successful surgeries in modern medicine, providing relief to thousands of patients suffering from chronic hip pain, often due to arthritis or fractures. The prosthetic components used in the surgery are designed to last for 20 years or more. However, like any major surgery, complications can occur. These complications may arise during surgery, immediately post-surgery, or years later. Timely identification and management of these complications are crucial for ensuring optimal recovery and long-term success of the surgery.
Functional Anatomy
The hip joint is a ball-and-socket joint made up of the femoral head (ball) and the acetabulum (socket). In total hip replacement, the damaged femoral head is replaced with a prosthetic ball, and the acetabulum is replaced with a prosthetic socket. The surrounding ligaments and muscles, particularly the gluteus medius, hip flexors, and rotator muscles, play essential roles in stabilizing the joint and allowing mobility. When complications arise, these components may be affected, leading to pain, instability, or functional limitations.
Biomechanics or Physiology
The femoral head rotates within the acetabulum to allow for normal movement in various directions. The components of a hip prosthesis are designed to replicate the natural biomechanics of the hip joint, maintaining stability and mobility. The success of the prosthesis depends on proper implant positioning and bone integration. When complications occur, such as dislocation or implant loosening, it disrupts the joint’s normal function, leading to pain and reduced movement.
Common Variants and Anomalies
Several complications can arise after hip replacement surgery, which include:
-
Dislocation: The prosthetic ball may pop out of the socket, leading to pain and instability.
-
Periprosthetic fracture: A break in the bone surrounding the implant, which may occur during or after surgery.
-
Sciatic nerve palsy: Damage to the sciatic nerve, leading to weakness or numbness in the lower leg.
-
Aseptic loosening: Loosening of the prosthetic components due to inflammation and bone resorption caused by wear debris.
-
Leg length discrepancy: A perceived or actual difference in leg length after surgery.
-
Impingement: The iliopsoas tendon may become impinged, leading to groin pain.
-
Infection: A serious complication that may require revision surgery.
-
Heterotrophic ossification: The formation of bone tissue in surrounding muscles, restricting movement and causing pain.
Total hip replacement dislocation
Dislocation may occur when the ball of the prosthetic joint pops out of the prosthetic socket. Majority of the total hip dislocation occurs in the first month following the surgery. Total hip dislocation occurs more frequently following the use of the posterior approach as compared to the anterior approach.
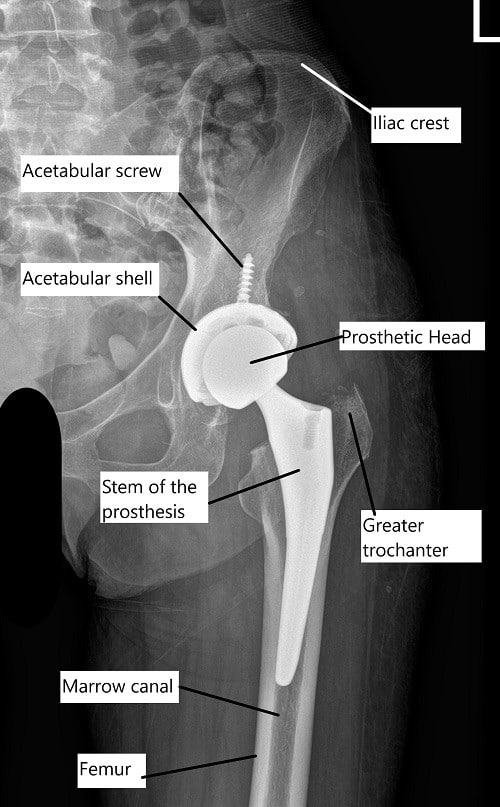
X-ray showing a total hip replacement.
Patient factors such as a prior hip surgery, elderly age, a history of alcoholism or drug abuse, and any neuromuscular disease such as Parkinson’s increase the risk for total hip joint dislocation.
Surgery factors include mal-position of the implant, inadequate repair of the soft tissues following the surgery. Noncompliance with the hip dislocation precautions immediately following the surgery also increase the risk for dislocation.
The management of dislocation following surgery is generally non operative but may require repeat surgery if dislocation is due to mal-position or wear of the plastic cup. Two or more dislocations need a revision surgery and may require the use of special implants to prevent future dislocation.
Periprosthetic fracture
Periprosthetic fracture is the break in bone surrounding the implant. The break may be in the bony acetabulum or the bony femur hosting the stem of the prosthesis. The fracture may occur during the surgery or may occur after the surgery.
While some stable fractures may be observed, the majority of the unstable fractures may require revision surgery. The surgery for periprosthetic fracture may require use of additional implants with plates, wires or screws.
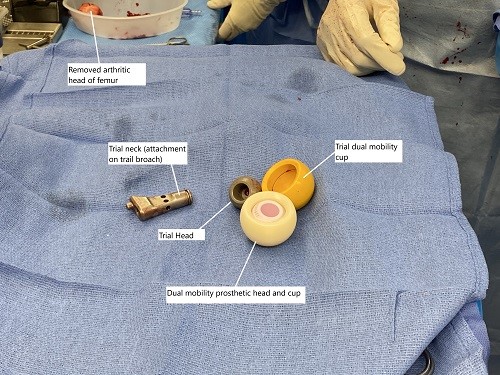
Intraoperative image showing a dual mobility cup system used for greater stability and prevention of dislocation.
Sciatic nerve palsy
Sciatic nerve is a large nerve that originates from the nerve roots in the lower spine. The nerve travels in the buttock behind the hip joint and supplies to the major muscles in the back of the thigh, calf and the foot.
Due to the proximity of the nerve to the hip joint, the nerve is often exposed during the posterior approach to the hip joint. The nerve is gently retracted back and is protected by the external rotator muscles.
The nerve may be damaged due to excessive pressure during retraction, direct injury to the nerve, lengthening of the leg, formation of blood collection, and in majority of the cases, the cause is unknown.
The patient may present with numbness, paresthesia, or inability to lift the foot up (foot drop). The treatment may include use of ankle foot orthotics until the nerve recovers.
Aseptic Loosening
The implanted prosthetic components may become loose secondary to aseptic loosening. Aseptic loosening occurs due to the body’s cells (macrophages) fighting against the microscopic particles released by the implanted components. The resulting inflammation may cause erosion of the bone around the implant leading to loosening. The management is usually surgical in the form of revision surgery.
Length discrepancy
There may be a leg length discrepancy following the surgery. Leg length discrepancy may occur as a result of operative techniques, contracture (fibrosis) or weakness of the muscles around the hip joint. At times, the patients may simply perceive the leg to be longer/shorter despite equal anatomical length. A shoe lift is generally helpful in resolving small discrepancies. A revision surgery may rarely be required for large discrepancy.
Impingement
There may be impingement of the iliopsoas tendon as it passes in front of the prosthetic joint. The iliopsoas tendon connects the iliopsoas muscles to the upper part of the femur. The tendon may impingement and cause groin pain especially during movement. The impingement may occur as a result of mal-position of the acetabulum implant, or due to the surgical technique. The management is generally surgical.
Prosthetic joint infection
Infection is a dreaded complication of hip replacement surgery and may require prolonged use of antibiotics and staged revision surgeries.
Heterotrophic ossification
Formation of bone tissue in the muscles surrounding the hip joint is a complication that may severely limit movement of the joint and cause pain. The cause of ossification may be linked to excessive surgery time and handling of the soft tissues during surgery. The management is generally surgical.
Clinical Relevance
Hip replacement surgery is generally successful, but complications like dislocation, infection, or implant loosening can lead to the need for revision surgery. Understanding these complications is crucial for both patients and surgeons to ensure timely treatment and prevent long-term disability. Early intervention for complications such as dislocation or infection can significantly improve outcomes, while conditions like aseptic loosening or nerve damage may require surgical correction or prolonged rehabilitation.
Imaging Overview
Imaging plays a critical role in diagnosing complications after hip replacement surgery:
-
X-rays are used to evaluate implant positioning, bone quality, and detect osteolysis or periprosthetic fractures.
-
MRI or CT scans are used to assess soft tissues, joint inflammation, or detect issues like impingement.
-
Bone scans help identify infection or areas of increased bone activity.
Radiologic assessments are crucial for monitoring the implant’s performance and identifying complications like implant loosening or infection.
Associated Conditions
Patients undergoing hip replacement surgery are at risk for complications including:
-
Hip dislocation: Often occurs in the first few months after surgery, especially if the prosthesis is not positioned correctly.
-
Periprosthetic fractures: These may result from trauma or stress to the bone surrounding the implant.
-
Sciatic nerve palsy: The nerve may be damaged due to retraction or pressure during surgery, leading to pain, weakness, or foot drop.
-
Aseptic loosening: Caused by wear debris that triggers an inflammatory response, leading to bone resorption and implant instability.
-
Impingement: The iliopsoas tendon may become impinged on the prosthetic components, causing groin pain.
-
Infection: This may occur in the immediate postoperative period or years later, often requiring antibiotic therapy and revision surgery.
-
Heterotrophic ossification: Bone formation in soft tissues, leading to restricted joint movement.
Surgical or Diagnostic Applications
-
Diagnosis: The diagnosis of complications such as dislocation or infection is made through clinical evaluation and imaging (X-ray, MRI, or CT scan).
-
Surgical management: Complications such as dislocation often require reduction or revision surgery. Aseptic loosening may require implant revision, and infection is managed through irrigation, debridement, and potentially implant replacement.
-
Non-surgical management: In some cases, conservative measures such as physical therapy, bracing, or medication may help manage complications like leg length discrepancy or groin impingement.
Prevention and Maintenance
To reduce the risk of complications following hip replacement surgery:
-
Follow surgical precautions: Avoid excessive hip flexion, internal rotation, or abduction during the early postoperative period, depending on the surgical approach.
-
Weight management: Maintaining a healthy weight reduces stress on the implant.
-
Avoid high-impact activities: Patients should avoid activities such as running or jumping that can accelerate wear on the implant.
-
Physical therapy: Strengthening the muscles around the hip joint is essential for improving mobility and preventing instability.
-
Regular follow-up imaging: Patients should undergo routine X-rays to monitor the implant for loosening or wear.
Summary and Key Takeaways
-
Hip replacement surgery is highly effective but can have complications such as dislocation, infection, aseptic loosening, and nerve injury.
-
Imaging is essential for diagnosing these complications and ensuring timely intervention.
-
Revision surgery is often required for dislocation, aseptic loosening, or periprosthetic fractures.
-
Physical therapy and postoperative care are essential for recovery and preventing complications such as thigh pain, impingement, or infection.
-
Dual mobility cups are effective for preventing dislocation in high-risk patients.
Do you have more questions?
What steps can I take to minimize my risk of experiencing complications such as dislocation or periprosthetic fracture following hip replacement surgery?
Minimizing risk factors such as maintaining a healthy weight, following postoperative precautions, and adhering to rehabilitation guidelines can help reduce the risk of complications after hip replacement surgery. Your surgeon can provide specific recommendations tailored to your individual needs and circumstances.
How common are complications like sciatic nerve palsy or aseptic loosening following hip replacement surgery, and what factors may increase my likelihood of experiencing these complications?
Complications like sciatic nerve palsy or aseptic loosening are relatively rare but can occur following hip replacement surgery. Factors such as surgical approach, patient anatomy, and overall health may influence the likelihood of experiencing these complications. Your surgeon can discuss the potential risks and risk factors with you in more detail.
If I experience symptoms such as numbness or weakness in my leg following hip replacement surgery, how soon should I seek medical attention, and what diagnostic tests may be necessary to determine the cause of my symptoms?
If you experience symptoms such as numbness or weakness in your leg following hip replacement surgery, it’s important to seek medical attention promptly. Your surgeon may recommend diagnostic tests such as imaging studies or nerve conduction tests to determine the cause of your symptoms and guide appropriate treatment.
What are the typical signs and symptoms of prosthetic joint infection, and how can I distinguish between normal postoperative discomfort and symptoms that may indicate an infection requiring medical attention?
Signs and symptoms of prosthetic joint infection may include increased pain, swelling, warmth, redness, fever, chills, or drainage from the surgical site. Distinguishing between normal postoperative discomfort and symptoms of infection can be challenging, so it’s important to promptly report any concerning symptoms to your healthcare provider for evaluation.
Are there specific lifestyle modifications or precautions I should follow to protect my prosthetic hip joint and reduce my risk of complications in the long term?
Following your surgeon’s recommendations for activity modification, weight management, and joint protection can help protect your prosthetic hip joint and reduce your risk of complications in the long term. Your surgeon can provide guidance on lifestyle modifications tailored to your individual needs and circumstances.
What is the typical recovery timeline after hip replacement surgery, and what factors may affect my recovery process and overall outcome?
The recovery timeline after hip replacement surgery can vary depending on individual factors such as age, overall health, surgical technique, and rehabilitation efforts. Your surgeon can provide guidance on what to expect during the recovery process and factors that may influence your outcome.
If I have concerns or questions about my hip replacement surgery or recovery process, who should I contact for assistance, and what resources are available to support me?
If you have concerns or questions about your hip replacement surgery or recovery process, you should contact your surgeon or healthcare provider for assistance. Additionally, there may be resources such as patient education materials, support groups, or rehabilitation services available to support you during your recovery journey.
Are there any specific activities or movements I should avoid after hip replacement surgery to minimize my risk of complications or implant wear?
Your surgeon may provide specific guidelines on activities or movements to avoid after hip replacement surgery to minimize your risk of complications or implant wear. Following these recommendations can help protect your prosthetic hip joint and promote a successful outcome.
What are the potential implications of complications such as heterotopic ossification or impingement on my long-term hip function and mobility, and how can these complications be effectively managed?
Complications such as heterotopic ossification or impingement may impact your long-term hip function and mobility. Your surgeon can discuss the potential implications of these complications and recommend appropriate management strategies, which may include surgical intervention or other treatments to address specific issues and optimize your outcomes.
How can I ensure that I receive appropriate follow-up care and monitoring after hip replacement surgery to detect and address any potential complications early on?
Ensuring regular follow-up appointments with your surgeon or healthcare provider can help facilitate ongoing monitoring and early detection of any potential complications after hip replacement surgery. Your surgeon can provide guidance on the recommended schedule for follow-up care and monitoring based on your individual needs and circumstances.
What are the potential risks associated with prolonged use of pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), following hip replacement surgery, and are there alternative pain management strategies available?
Prolonged use of pain medications, including NSAIDs, may carry risks such as gastrointestinal ulcers, kidney damage, and cardiovascular complications. Your healthcare provider can discuss these risks with you and explore alternative pain management strategies, such as physical therapy, acupuncture, or nerve blocks, to help minimize the need for long-term medication use.
Can you explain the difference between stable and unstable periprosthetic fractures, and how does the severity of the fracture influence the treatment approach?
Stable periprosthetic fractures are those in which the bone fragments remain relatively aligned and do not significantly affect the stability of the implant. Unstable fractures involve significant displacement of the bone fragments and may compromise the stability of the implant. Treatment approaches vary depending on the severity of the fracture, with stable fractures potentially managed conservatively and unstable fractures often requiring surgical intervention.
What precautions should I take to prevent falls and minimize the risk of complications, such as periprosthetic fracture or dislocation, particularly during the early stages of recovery after hip replacement surgery?
Taking precautions to prevent falls, such as using assistive devices like walkers or canes, ensuring clear pathways, and avoiding slippery surfaces, can help minimize the risk of complications during the early stages of recovery after hip replacement surgery. Your healthcare provider can provide specific guidance on fall prevention strategies tailored to your individual needs and circumstances.
Are there any dietary or nutritional considerations I should be aware of before and after hip replacement surgery to promote optimal healing and recovery?
Maintaining a balanced diet rich in nutrients such as protein, vitamins, and minerals can support optimal healing and recovery after hip replacement surgery. Your healthcare provider may recommend dietary modifications or supplements to ensure adequate nutrition before and after surgery, particularly if you have specific nutritional needs or deficiencies.
What factors should I consider when deciding whether to undergo hip replacement surgery, and how can I weigh the potential benefits against the risks and potential complications?
When considering hip replacement surgery, it’s important to weigh factors such as the severity of your symptoms, your overall health and medical history, and the potential benefits and risks of the procedure. Consulting with your surgeon and discussing your individual circumstances can help you make an informed decision about whether hip replacement surgery is the right choice for you.
Are there any lifestyle modifications or adaptive equipment that can help me maintain independence and quality of life following hip replacement surgery, particularly if I experience mobility limitations or other challenges during recovery?
– Lifestyle modifications such as modifying your home environment, using assistive devices like grab bars or raised toilet seats, and incorporating adaptive equipment like reachers or dressing aids can help you maintain independence and quality of life following hip replacement surgery. Your healthcare provider or a rehabilitation specialist can provide recommendations and resources to support your recovery and ongoing function.
What steps can I take to optimize my physical and mental health before hip replacement surgery, and how might factors such as stress or anxiety impact my recovery process?
Prior to hip replacement surgery, focusing on activities that promote physical and mental well-being, such as regular exercise, stress management techniques, and maintaining social connections, can help optimize your overall health and resilience for surgery and recovery. Managing stress and anxiety effectively can also positively influence your recovery process and outcomes.
Is there a risk of developing complications such as blood clots or deep vein thrombosis (DVT) after hip replacement surgery, and what preventive measures can be taken to reduce this risk?
– Yes, there is a risk of developing complications such as blood clots or DVT after hip replacement surgery. Preventive measures may include early mobilization, compression stockings, blood-thinning medications, and mechanical devices such as intermittent pneumatic compression devices. Your healthcare provider can assess your individual risk factors and recommend appropriate preventive strategies.
What role does physical therapy play in the recovery process after hip replacement surgery, and how can I ensure that I adhere to my rehabilitation program effectively?
Physical therapy plays a crucial role in the recovery process after hip replacement surgery by helping restore mobility, strength, and function. Adhering to your rehabilitation program effectively may involve attending scheduled therapy sessions, performing prescribed exercises at home, and communicating regularly with your physical therapist to address any challenges or concerns.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://www.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
