Hip Pain and Sciatica
Pain around the hip region may originate from the hip or a pinched nerve in the back. Hip pain commonly results from wear and tear arthritis of the hip joint. A pinched nerve or sciatica results from compression or irritation of the nerve roots in the back. While both conditions may present similarly, their differentiation is important for correct treatment.
Hip pain
The hip joint is formed, but the upper part of the thigh bone and the pelvis. The joint is located behind the groin area and is involved in various activities such as sitting, walking, running, standing, etc. The hip joint may be involved in wear and tear arthritis known as osteoarthritis. The hip joint’s other afflictions may be avascular necrosis of the hip, rheumatoid arthritis, trauma/injury, etc.
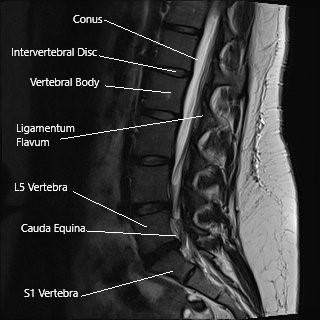
Sagittal section of the lumbosacral spine on MRI.
The pain from the pathologies of the hip joint commonly present in the front of the hip joint, i.e., the groin area. The pain may also be present on the sides or the back of the hip joint, i.e., the buttocks. At times, the hip pain may radiate down the thigh towards the inner side of the knee, but it is rare for the hip pain to present below the knee.
The hip pain due to underlying arthritis is usually worse with activity and gets better with rest. The patients may find it increasingly difficult to perform activities such as walking or climbing stairs. The pain of avascular necrosis of the head of the femur may present at rest and gets worse with activity.
Sciatica
Sciatica is a myriad of symptoms caused by a pinched nerve in the back. The sciatic nerve is the largest nerve in the human body, starting from the back and dividing into various branches till the toes. The sciatic nerve is formed by the spinal nerves L4, L5, S1, S2, and S3.
The sciatic nerve exits the pelvis in the buttock and travels in the back of the thigh. The nerve divides into two branches just above the back of the knee joint. The two branches give rise to various nerves that supply the calf and the feet.
The sciatic nerve is responsible for coordinating the movements of the muscles in the legs and feet. The nerve also carries nerve signals of sensation such as touch, pressure, and temperature from the lower extremities to the brain.
A pinched nerve results from compression or irritation of any of the nerve roots that form the sciatic nerve. The nerve may also be compressed as it passes beneath the piriform muscle (piriformis syndrome).
Sciatica presents as a pain in the buttocks that may go down the back of the thigh and calf. There may be an associated feeling of pins and needles in the legs. If the nerve roots’ compression is severe, there may be a progressive weakness of the legs, and patients may complain of difficulty in walking, getting up from a chair, or navigating stairs. The weakness may be accompanied by numbness in the legs and toes.
The pain may be aggravated by activities such as bending forward, sitting, coughing, sneezing when the herniated intervertebral disc is the cause of sciatica. Similarly, when the cause of sciatica is spinal canal stenosis, the symptoms may be aggravated on activities that require a patient to bend backward, such as walking downhill.
In rare instances, the compression of nerve roots in the spinal canal may lead to cauda equina syndrome symptoms. Cauda equina syndrome involves weakness and numbness of lower extremities, numbness of the saddle area, and bowel and bladder control loss.
Hip pain Vs. Sciatica
As there may be a significant overlay of hip pain and sciatica symptoms, it becomes important to examine and diagnose the root cause of pain. Pain in the buttocks may be caused by hip pathologies or may be a symptom of sciatica.
The buttock pain that radiates down the back of the thigh, along with back pain, is usually due to spine pathology. Meanwhile, buttock pain may or may not be associated with groin pain, and that gets worse with activity may indicate hip arthritis.
The pain of hip pathology usually is centered at the groin, and it is rare for it to radiate below the knee joint. Sciatica symptoms may, on the other hand, may radiate down the legs into the toes. Secondary to the hip joint pathology, patients may walk with a limp, and in severe cases of arthritis, there may be leg length discrepancy.
Usually, the attending orthopedic surgeon will examine the patient and extract a history leading to the symptoms. The physician may perform physical examinations to find out the part of the spine or the hip leading to the symptoms.
Radiological examinations for the hip usually include an X-Ray, which may or may not be followed by an MRI or a CT scan. The diagnosis of spinal pathologies causing sciatica usually requires an MRI investigation. An MRI is able to differentiate between the soft tissue structures such as nerves, ligaments, intervertebral disc, etc.
The management of hip disease usually depends upon the diagnosis and the age of the patient. The management of advanced arthritis and avascular necrosis is usually a total hip replacement surgery. Younger patients with mild arthritis may benefit from hip arthroscopic procedures.
The management of sciatica is usually conservative in the form of medications, heat or cold therapy, physical therapy, etc. In some cases, patients may require decompression surgeries such as microdiscectomy or laminoplasty. Patients with the instability of the spine may require lumbar fusion surgeries.
Do you have more questions?
How can I differentiate between hip pain caused by musculoskeletal issues, such as arthritis, and pain originating from intra-abdominal problems like hernias?
Distinguishing between musculoskeletal hip pain and pain originating from intra-abdominal issues can be challenging. Asking your healthcare provider about specific symptoms, such as location, severity, and exacerbating factors, may help clarify the underlying cause of your hip pain.
What lifestyle modifications can I implement to alleviate hip pain, and are there any activities I should avoid to prevent exacerbating the condition?
Making lifestyle modifications may help alleviate hip pain and improve overall joint health. Your healthcare provider can offer guidance on activities to avoid and recommend exercises or ergonomic adjustments to support hip health and minimize discomfort.
Are there any specific risk factors or predisposing factors that may increase my likelihood of experiencing hip pain, and how can I mitigate these risks?
Identifying risk factors or predisposing factors for hip pain can help you take proactive steps to mitigate these risks and prevent future episodes of discomfort. Your healthcare provider can provide personalized recommendations based on your medical history, lifestyle factors, and overall health status.
Can psychological factors, such as stress or anxiety, contribute to or exacerbate hip pain, and are there strategies for addressing these factors as part of a comprehensive treatment plan?
Psychological factors, including stress and anxiety, may contribute to or exacerbate hip pain in some individuals. Integrating strategies for addressing psychological factors, such as stress management techniques or cognitive-behavioral therapy, as part of a comprehensive treatment plan may help improve overall pain management and quality of life.
What role does posture and body mechanics play in the development and management of hip pain, and are there specific exercises or techniques to improve alignment and reduce strain on the hip joint?
Posture and body mechanics can influence the development and management of hip pain. Your healthcare provider or physical therapist can recommend exercises or techniques to improve posture, strengthen supportive muscles, and reduce strain on the hip joint, which may help alleviate discomfort and prevent further injury.
Is there a connection between hip pain and other musculoskeletal conditions, such as lower back pain or knee pain, and how can addressing underlying issues in one area of the body impact hip health?
Hip pain may be interconnected with other musculoskeletal conditions, such as lower back pain or knee pain, due to biomechanical relationships within the body. Addressing underlying issues in one area of the body, such as through physical therapy or targeted exercises, may positively impact overall hip health and reduce pain.
Are there any specific dietary supplements or nutritional interventions that may help support joint health and alleviate hip pain, and how do I ensure safe and effective use of these supplements?
Certain dietary supplements or nutritional interventions may offer benefits for joint health and pain management. Your healthcare provider or a registered dietitian can provide guidance on safe and effective use of supplements, as well as recommend dietary modifications to support overall joint health and reduce inflammation.
What role does weight management play in managing hip pain, and are there recommended weight loss strategies for individuals experiencing discomfort or limited mobility due to hip issues?
Weight management can play a significant role in managing hip pain, as excess body weight can increase stress on the hip joint and exacerbate symptoms. Your healthcare provider can offer personalized recommendations for weight loss strategies, including diet modifications, exercise programs, and lifestyle changes tailored to your individual needs and goals.
How can I best advocate for myself in seeking appropriate diagnosis and treatment for hip pain, and what steps can I take to ensure I receive comprehensive care and support throughout the treatment process?
Are there any alternative or complementary therapies, such as acupuncture or massage, that may help alleviate hip pain, and how do I determine if these treatments are appropriate for me?
Alternative or complementary therapies like acupuncture or massage may offer relief for some individuals with hip pain. Your healthcare provider can discuss the potential benefits and risks of these therapies, as well as help you determine if they are appropriate for your specific condition and overall health
What are the potential long-term effects of chronic hip pain, and how can I best manage and cope with ongoing discomfort to maintain quality of life?
Chronic hip pain can have significant long-term effects on quality of life, including decreased mobility, functional limitations, and psychological distress. Learning effective pain management strategies, engaging in regular physical activity, and seeking support from healthcare providers or support groups can help you cope with ongoing discomfort and maintain overall well-being.
How does aging affect the prevalence and management of hip pain, and are there age-specific considerations I should be aware of in addressing my symptoms?
Aging can impact the prevalence and management of hip pain due to factors such as degenerative changes in the joint, decreased muscle strength, and changes in activity levels. Your healthcare provider can provide age-specific recommendations and considerations for managing hip pain, taking into account your individual needs, preferences, and overall health status.
Can hip pain be a symptom of more serious underlying conditions, such as infection or cancer, and what warning signs should I watch for that may indicate the need for urgent medical attention?
Hip pain can sometimes be a symptom of more serious underlying conditions, including infection or cancer. It’s important to be aware of warning signs such as persistent pain, unexplained weight loss, fever, or changes in bowel or bladder function that may indicate the need for urgent medical attention. If you experience any concerning symptoms, seek prompt evaluation from a healthcare provider.
How does gender influence the risk of developing hip pain, and are there gender-specific factors or considerations that may impact diagnosis and treatment?
Gender may influence the risk of developing hip pain due to differences in anatomy, hormonal factors, and activity levels between males and females. Your healthcare provider can discuss gender-specific considerations and recommendations for diagnosis and treatment based on current research and clinical guidelines.
Can certain occupations or activities increase the risk of hip pain, and are there specific ergonomic modifications or preventive measures I should consider to reduce my risk of injury?
Certain occupations or activities that involve repetitive motions, heavy lifting, or prolonged periods of sitting or standing may increase the risk of hip pain and injury. Your healthcare provider or occupational therapist can offer guidance on ergonomic modifications, proper lifting techniques, and preventive measures to reduce your risk of hip pain related to occupational or recreational activities.
What role does inflammation play in the development and progression of hip pain, and are there dietary or lifestyle factors that can help reduce inflammation and alleviate symptoms?
Inflammation may contribute to the development and progression of hip pain, particularly in conditions such as arthritis or bursitis. Your healthcare provider or a registered dietitian can discuss dietary and lifestyle factors that may help reduce inflammation and alleviate symptoms, such as consuming anti-inflammatory foods, maintaining a healthy weight, and managing stress.
Are there genetic factors or hereditary conditions that may predispose me to hip pain, and how can I determine if my family history influences my risk of developing hip problems?
Genetic factors or hereditary conditions may play a role in predisposing individuals to hip pain or musculoskeletal disorders. Discussing your family history with your healthcare provider can help determine if you have any genetic predispositions or familial patterns that may influence your risk of developing hip problems, allowing for proactive management and preventive measures.
What are the potential limitations or risks associated with surgical interventions for hip pain, and how can I make an informed decision about whether surgery is the right option for me?
Surgical interventions for hip pain carry potential limitations and risks, including complications, prolonged recovery periods, and uncertain outcomes. Your healthcare provider can discuss the potential benefits and risks of surgery, as well as alternative treatment options, allowing you to make an informed decision about whether surgery is the right option for you based on your individual circumstances and treatment goals.
Can sciatica cause knee pain?
Sciatica pain is usually radiated along the back or the side of the thigh and knee into the leg. Occasionally, patients may present with a confusing picture of knee problem, but maybe having sciatica. A thorough history and examination by the physician as well as diagnostic tests in the form of x-rays and MRI may be needed to confirm the diagnosis.
How to fix sciatica nerve pain?
Sciatica nerve pain can be relieved to various modalities. To start with, antiinflammatory medications like ibuprofen, naproxen or Tylenol may help. If pain is not relieved with the medications, physical therapy, chiropractor and acupuncture may also help. The patient may also take medications including gabapentin or pregabalin for pain relief.
The patient should take a short period of bed rest for a day or two. The patient should continue to do normal usual activities. If the pain is not relieved, he should see his doctor. Epidural injection or nerve root blocks may help in relieving the sciatica pain. Patients who are not having any relief with any of the above-mentioned treatment plans, may need an MRI for confirmation of diagnosis and possibly surgery to relieve their pain.
How do you diagnose sciatica?
Sciatica is a clinical diagnosis, which can be corroborated by imagings with or without nerve conduction/EMG studies. Typical patient will present with pain radiating down one leg along the back or the side of the thigh index. They may have been associated with tingling and numbness or back pain.
Occasionally, patients may have weakness in the toes or the ankle. Once the clinical diagnosis is made, confirmation can be done using x-rays and MRI. In patients who have a confusing picture due to underlying comorbidity or atypical presentation, nerve conduction study and electromyographic study can be done to further confirm or rule out sciatica.
Is heat or ice better for sciatica?
Heat is usually better in patients who have sciatica, though patients who are not relieved with heat should also try ice or occasionally rhythmic use of heat and ice, cyclic use of heat or ice may help better than one alone.
Does massage help sciatica?
Massage is one of the modalities of adjuvant therapy for sciatica can be helpful and can decrease pain by strengthening the muscles as well as stretching the nerves. Deep massage can also help decrease the muscle spasms that develop in patients with sciatica.
Where to put an ice pack for sciatica?
For sciatica, an ice pack or even a heating pad can be used by placing it into the lower back and the gluteal region. It helps decrease the inflammation of the nerve there and thereby decreasing the pain and associated symptoms.
Does the inversion table help sciatica?
Inversion table similar to traction helps sciatica by increasing the height of the disk and thereby allowing the disk to go back into space thereby decreasing the compression of the nerve root may help in decreasing the pain of sciatica. The issue of inversion table as well as traction is that this is effective until the patient uses them and once the patient is upright and moving, the effect of the inversion table or the traction may not be persistent.
Can the sciatica cause ankle pain?
Sciatica or lumbar radiculopathy causes pain radiating from the back or the hip into the lower extremities down the leg. The pain radiates along the back or the side of the thigh and leg and radiates down foot. An isolated ankle pain may not be caused by radiculopathy. If the pain is on outer or inner side of the ankle and is radiating down or coming from the top then it may be associated with sciatica or lumbar radiculopathy.
Does sciatica get worse before it gets better?
90% of patients with sciatica will eventually get better in a period of four to six weeks. During this time, the pain may worsen also or it may keep on improving. Patients who have severe pain with or without tingling or numbness usually will need medical attention to relieve their pain during this duration. The treatment may involve medications, physical therapy and cortisone shots. Patients who have sudden onset of neurological deficit or weakness or worsening of the neurological deficit may need surgery also.
Can stress cause sciatica?
Sciatica like any other neurologic pain can have relation with the mental status and cognitive functions of the person. Though stress may directly not be the causative factor for sciatica, it may have its effect on the severity as well as course of the disease process of sciatica. Patients with high stress levels may have difficulty coping with sciatica and may take longer time to get better.
What happens if sciatica left untreated?
Sciatica in most patients will get better by itself in a period of four to six weeks. The pain as well as tingling and numbness tend to improve over time, though it may have periods of worsening. Patients may need treatment in the form of medications or injections to relieve the pain, so as to spend this period of four to six weeks, till then the relief is evident.
Occasionally in about 10% of the patients, there will be no relief, worsening or recurrence of sciatica pain despite all treatment modalities over four to six weeks. These patients may need surgical management to relieve their pain due to the pressure over the nerve roots.
Can sciatica be a serious disorder?
Sciatica is usually self limiting in 90% of patients and only needs treatment in the form of medication and physical therapy and occasionally cortisone injection. In about 10% of patients, this may not be relieved by any modality and these patients may need to undergo surgical treatment.
Sciatica can also rarely lead to rapid neurological deficit presenting in the form of cauda equina syndrome, which can be potentially disabling. The neurological deficit caused due to cauda equina syndrome may be permanent especially if not treated early in the disease process. Such patients may not only have weakness in their legs, but may also lose control over their bowel and bladder, which may or may not recover over time.
What are the medication that can help sciatica?
Sciatica pain can be relieved by the help of anti-inflammatory medications like ibuprofen, naproxen. It can also be helped by Tylenol. Stronger pain medications like tramadol and narcotic medications may occasionally be needed for a short period of time.
Neuromodulator medications like gabapentin and pregabalin may also be helpful in decreasing the sciatica pain. Occasionally, medications like amitriptyline, duloxetine and carbamazepine may also be used in some patients to relieve their pain.
Is the back brace helpful for sciatica pain?
Back brace may be helpful in patients who have back pain with or without sciatica. Patients who have only radicular pain in their lower extremity may not be helped by the back brace. Use of back brace for a long period of time may be detrimental by causing atrophy of the back muscles.
What causes hip joint pain?
Pain in and around the hip joint has a vast myriad of potential causes. They range from the musculoskeletal in nature (e.g. hip arthritis, greater trochanteric bursitis, iliopsoas impingement) to the intra-abdominal (e.g. sportsman’s hernia, inguinal hernia, athletic pubalgia) to the less clear-cut or multifactorial (e.g. complex regional pain syndrome, fibromyalgia).
Although each of the aforementioned conditions will cause a form of hip pain, the hip pain will be slightly different depending on the cause and these differences will be identified by your healthcare practitioner and will help them achieve a definitive diagnosis of the underlying cause of your hip pain.
What does hip pain feel like?
Pain in and around the hip can present in great number of different ways, and each identifiable cause of hip pain has a unique presentation and characteristic quality to the pain itself. For example, hip osteoarthritis pain tends to present as a dull ache that is exacerbated with weightbearing, iliopsoas impingement tends to present as a sore burning sensation that is worsened with resisted hip flexion and an inguinal hernia will present with pain around the hip that is worsened with a Valsalva maneuver.
That being said there are number of conditions that will present with hip pain of very similar nature, for example pain from osteoarthritis can often be confused with pain from femoroacetabular impingement or any other intra-articular cause of hip pain.
Where is hip pain felt?
Although pain in the hip is generally felt in and around the hip joint, its specific location can give away key clues to the underlying cause of the hip pain. For example, greater trochanteric pain will worsen with specific palpation of the area directly overlying the greater trochanter. Hernia type pain will be felt more so in groin than the lateral deep aspects of the hip. Hip pain can even be felt in the buttock area – this is a common presentation of osteoarthritis.
What to do for hip pain?
Any sustained hip pain that lasts longer than a few days and is refractory to conservative management such as over-the-counter analgesics and rest, stretching or continued exercise should be brought to attention of a medical professional. Although a good amount of hip pain will respond well to over-the-counter analgesics such as Tylenol and nonsteroidal anti-inflammatory drugs, these may temporarily relieve the pain but on cessation of these medications, the pain may very well return.
Depending on the cause of the hip pain, these may actually be ineffective (for example using anti-inflammatories and Tylenol to treat an inguinal hernia will be largely ineffective. Although it may provide some pain relief, this will be likely incomplete and very temporary). Our specialist orthopedic surgeons would be happy to consult with you regarding any hip pain that you may have been experiencing and will help to reach a definitive diagnosis which is key to successfully treating your hip pain.
Can lower back pain cause hip pain?
One of the most common scenarios a surgeon will see is a patient who presents with pain in the hip and attribute this pain to arthritis of the hip, but on consultation with our specialist orthopedic surgeons and review of plain film radiographs, the patient lacks any radiographic evidence of arthritis in the hips at all, however, assessment of the lower back reveals significant arthritis in this area.
This is a common presentation for many people who experience hip pain that is actually coming from the lower back. Depending on the extent of the involvement of the lower back and the specific symptoms the patient presents, they may warrant a referral to a spine specialist, but in most cases a course of sustained and effective physical therapy often provides these patients with the muscular training that they require in order to improve their arthritis pain originating from their lumbar spine.
What doctor should I see for my hip pain?
Many patients choose to visit their regular family physician with hip pain complaints and this is perfectly reasonable, as is presenting to a physiotherapist or chiropractor. However, our specialist orthopedic surgeons have years of experience treating hip specific problems and are best qualified to assist you in achieving a definitive diagnosis for the cause of your hip pain.
Once we have made this diagnosis, we will be more than happy to discuss with you the treatment options and whether this includes surgery or nonsurgical options such as physical therapy, nonsteroidal anti-inflammatory medications, gait aids and injections.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
