Piriformis Syndrome and Sciatica
Piriformis syndrome is a medical condition that causes sciatica symptoms of leg pain usually caused by lumbar radiculopathy. Sciatica is a collection of symptoms caused by nerve root compressions at the level of the spine. A herniated intervertebral disc is the most common cause of sciatica symptoms while piriformis syndrome is caused by compression of the nerve below the pelvis.
Anatomy of Lumbar Spine
The sciatic nerve is the largest nerve in the human body made by the collection of the nerve roots L4, L5, S1, S2, and S3. The nerve originates in the lower spine, and as it travels down the pelvis, it lies in front of the piriformis muscle. The nerve exits below the piriformis muscle and lies deep beneath the biceps femoris muscle at the back of the thigh.
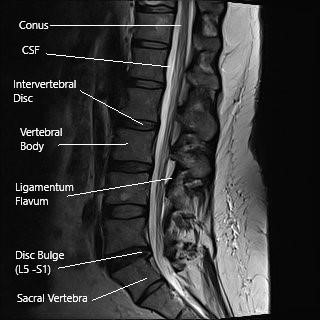
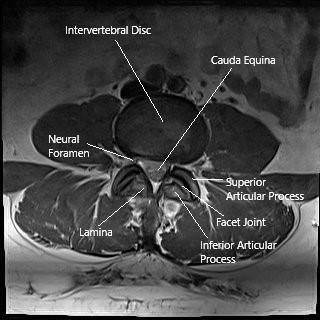
Sagittal and axial sections of the lumbar MRI
The sciatic nerve continues down the thigh and at the knee joint’s level, divided into two branches, the tibial nerve, and the common peroneal nerve. The sciatic nerve provides motor supply to major muscles in the thigh, leg, and feet. The nerve supplies the muscles responsible for bringing the thighs together, bending the knee, bending and extending the ankle and the toes. Besides the motor supply, the sciatic nerve carries the sensory input from the legs and feet.
The piriformis muscle is a small muscle originating from the inner aspect of the sacral bone. The muscle extends outwards and attaches to the prominence on the hip bone’s outer side (greater trochanter). The muscle primarily functions to rotate the hip joint outwards (external rotation) and aid in moving the hip to the side (abduction). External rotation and abduction movements help us in our day-to-day activities such as walking, sitting, running, etc.
Causes of Piriformis Syndrome
Piriformis syndrome occurs due to compression or irritation of the sciatic nerve as it passes under the muscle. The compression may occur as a result of muscle spasm in the piriformis due to irritation.
The piriformis spasm may occur due to excessive training without adequate stretching or repetitive action irritating the muscle. Piriformis tightening or swelling may occur as a result of direct injury to the buttock. The nerve may get entrapped inside the piriformis due to initial injury leading to adhesion of the nerve to the muscle.
There may be anatomical variations in the nerve’s relation to the piriformis muscle. The nerve may split into two parts, passing below it and the other passing above it. The split nerves join below the piriformis to continue down the thigh. One of the divided nerves or the whole sciatic nerve may also pass through the piriformis muscle.
The anatomical variation may make the sciatic nerve more vulnerable to compression or irritation at the piriformis muscle level. The entrapment may occur at the bony ischial tuberosity level or between the piriformis and the gemellus obturator internus muscle complex.
Symptoms of Piriformis Syndrome
The piriformis syndrome usually causes buttock pain that may or may not radiate down the thigh. The pain is generally exacerbated by activities such as sitting or walking for prolonged periods. The patients may especially be intolerant to sitting. In some cases, patients may experience sciatica symptoms during bowel movements as the muscle originates in the pelvis.
The sciatica symptoms caused by lumbar radiculopathy typically occur with activities such as raising your leg while laying down. Additionally, as sciatica is one of the many symptoms caused by the pathology at the spine level, the symptoms may be related to the cause of narrowing the spine. In the herniated intervertebral disc, activities such as bending forward, coughing, sneezing, etc., may worsen the symptoms. In the case of spinal stenosis, activities that involve bending the spine back make the symptoms worse.
Diagnosis of Piriformis Syndrome
The consulting spine surgeon will extract a thorough history regarding the onset of the symptoms and the activities that make the symptoms better or worse. Through a physical examination, the physician will try to localize the pathology causing the sciatica symptoms, which may be coming from the spine or the piriformis muscle.
Physical examination may involve a straight leg raise test, Pace test, and FAIR (flexion, abduction, internal rotation test). The Pace sign is the demonstration of pain from resisted external rotation and abduction. A positive FAIR test involves demonstrating pain as the physician tries to adduct and internally rotate the affected hip.
The straight leg raise test is usually positive in the case of sciatica resulting from lumbar radiculopathy. The test usually involves a demonstration of pain in the back as one lifts the affected leg in the range of 30 to 70 degrees. The test may also be positive in the case of piriformis syndrome.
Additionally, the physician looks for pain on pressing the area of the sciatic notch. The physician may request radiological investigations and neurodiagnostic studies to differentiate the sciatica symptoms.
Management of Piriformis Syndrome
The treatment of piriformis syndrome is mainly conservative. Conservative management involves anti-inflammatory medications, physical therapy, heat, and cold therapy, etc. The majority of the patients experience an excellent relief of symptoms. NSAID (nonsteroidal anti-inflammatory) medication such as naproxen and ibuprofen act to reduce the inflammation at the site of entrapment/compression/irritation.
Physical therapy is aimed to strengthen and stretch the piriformis muscle to reduce the tightening of the muscle. To improve the patient’s physical therapy participation, the surgeon may inject corticosteroid medication near the sciatic nerve to provide relief from symptoms. Very rarely, operative management may be needed to cut the muscle and release the nerve.
Do you have more questions?
How does Piriformis Syndrome differ from other causes of sciatica?
Unlike disc-related sciatica, Piriformis Syndrome involves the sciatic nerve being compressed by the piriformis muscle rather than a spinal disc herniation.
What are the most common symptoms of Piriformis Syndrome?
Common symptoms include deep buttock pain, pain that worsens with sitting, pain radiating down the leg, and discomfort with hip movements.
What causes the piriformis muscle to compress the sciatic nerve?
Causes include trauma to the buttock, overuse from activities like running, anatomical variations, or muscle spasm and hypertrophy.
What are the first steps in treating Piriformis Syndrome?
Initial treatment usually includes physical therapy, stretching exercises, pain relief with NSAIDs, and muscle relaxants.
Can Piriformis Syndrome resolve on its own?
In some cases, symptoms can resolve with rest and conservative treatment, but persistent symptoms may require more active intervention.
What exercises are recommended for Piriformis Syndrome?
Exercises often include piriformis stretches, hip abductor strengthening, and neurodynamic exercises to mobilize the sciatic nerve.
When should surgery be considered for Piriformis Syndrome?
Surgery is considered when conservative treatments fail to relieve symptoms, and the patient’s quality of life is significantly impacted.
Can injections help with Piriformis Syndrome?
Yes, corticosteroid or Botox injections can be used to reduce inflammation and muscle spasm, providing significant pain relief for some patients.
Is Piriformis Syndrome common among athletes?
What role does anatomy play in Piriformis Syndrome?
Anatomical variations in the sciatic nerve’s pathway relative to the piriformis muscle can predispose individuals to the syndrome.
Can sitting for long periods cause Piriformis Syndrome?
Yes, prolonged sitting, especially on hard surfaces, can aggravate the piriformis muscle, leading to or worsening the condition.
Are there any specific risk factors for developing Piriformis Syndrome?
Risk factors include previous trauma to the buttock area, prolonged sitting, and certain physical activities that strain the hip and buttock muscles.
How long does it take to recover from Piriformis Syndrome?
Recovery time varies but can range from a few weeks to several months, depending on the severity and the effectiveness of the treatment.
Can Piriformis Syndrome recur after treatment?
Yes, without proper management and lifestyle adjustments, such as regular exercise and ergonomic changes, the syndrome can recur.
What lifestyle changes can help prevent Piriformis Syndrome?
Preventive measures include maintaining good posture, taking breaks from prolonged sitting, regular stretching, and strengthening exercises.
Is there a specific type of doctor I should see for Piriformis Syndrome?
An orthopedic surgeon, especially one specializing in spine or sports medicine, is well-equipped to diagnose and treat Piriformis Syndrome.
Can Piriformis Syndrome affect both sides of the body?
It is typically unilateral, but in rare cases, it can affect both sides if the underlying causes or risk factors are present on both sides.
Can Piriformis Syndrome be confused with other conditions?
Yes, it can be confused with lumbar radiculopathy, sacroiliac joint dysfunction, or hip disorders due to overlapping symptoms.
What imaging studies are most useful in diagnosing Piriformis Syndrome?
MRI is the preferred imaging study to rule out other causes and may show an enlarged piriformis muscle or anatomical variations.
Can Piriformis Syndrome cause permanent nerve damage?
If untreated, chronic compression of the sciatic nerve can potentially lead to nerve damage, though this is rare.
Can physical therapy alone cure Piriformis Syndrome?
Physical therapy is highly effective for many patients and can cure the condition, especially when combined with other conservative treatments.
Are there any complications associated with Piriformis Syndrome?
Complications may include chronic pain, muscle weakness, and in rare cases, nerve damage if the condition is not adequately treated.
Is Piriformis Syndrome hereditary?
There is no direct hereditary link, but anatomical variations that predispose someone to the syndrome may be inherited.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
