Posterior Cervical Fusion
At Complete Orthopedics, we focus on treating back and neck pain with customized treatment plans and various surgical options. We prioritize a comprehensive understanding of your symptoms to deliver precise diagnoses and effective treatments, whether to alleviate post-surgical pain or determine the need for additional surgery.
Our clinics, spread across New York City and Long Island, are affiliated with six leading hospitals and outfitted with cutting-edge technology for advanced back and neck surgeries. Booking a consultation with our orthopedic specialists is easy, available both online and by phone.
Overview
Posterior cervical fusion means operating the neck from the back and doing a fusion surgery so as to stabilize the neck. This surgery is usually performed in conjunction with laminectomy. Laminectomy means removing the bone and the tissue from the back of the spinal cord in the neck. Laminectomy is performed to remove the pressure from the spinal cord and possibly nerve roots if needed.
Laminectomy in itself is bound to fail by causing instability of the neck. Posterior cervical fusion provides stability to the neck after laminectomy, to avoid late failures, which can be disastrous.
The surgery of posterior cervical fusion and laminectomy is usually performed on a long segment covering almost 50-70% of the neck as compared to the surgery from the front, which includes anterior cervical discectomy and fusion (ACDF) and Total disc replacement (TDR) and is done at shorter levels of 1 to 3 levels only.
Posterior cervical fusion and laminectomy is usually performed over 4 to 6 segments depending on the need. As it is a fusion surgery, it also leads to more stiffness, but the patients who usually need this surgery are already stiff and have pathology or disease, which can be properly taken care of from the surgery from the back of the neck only. If the disease is localized and can be taken care of from the front, then surgery from the front is preferred.
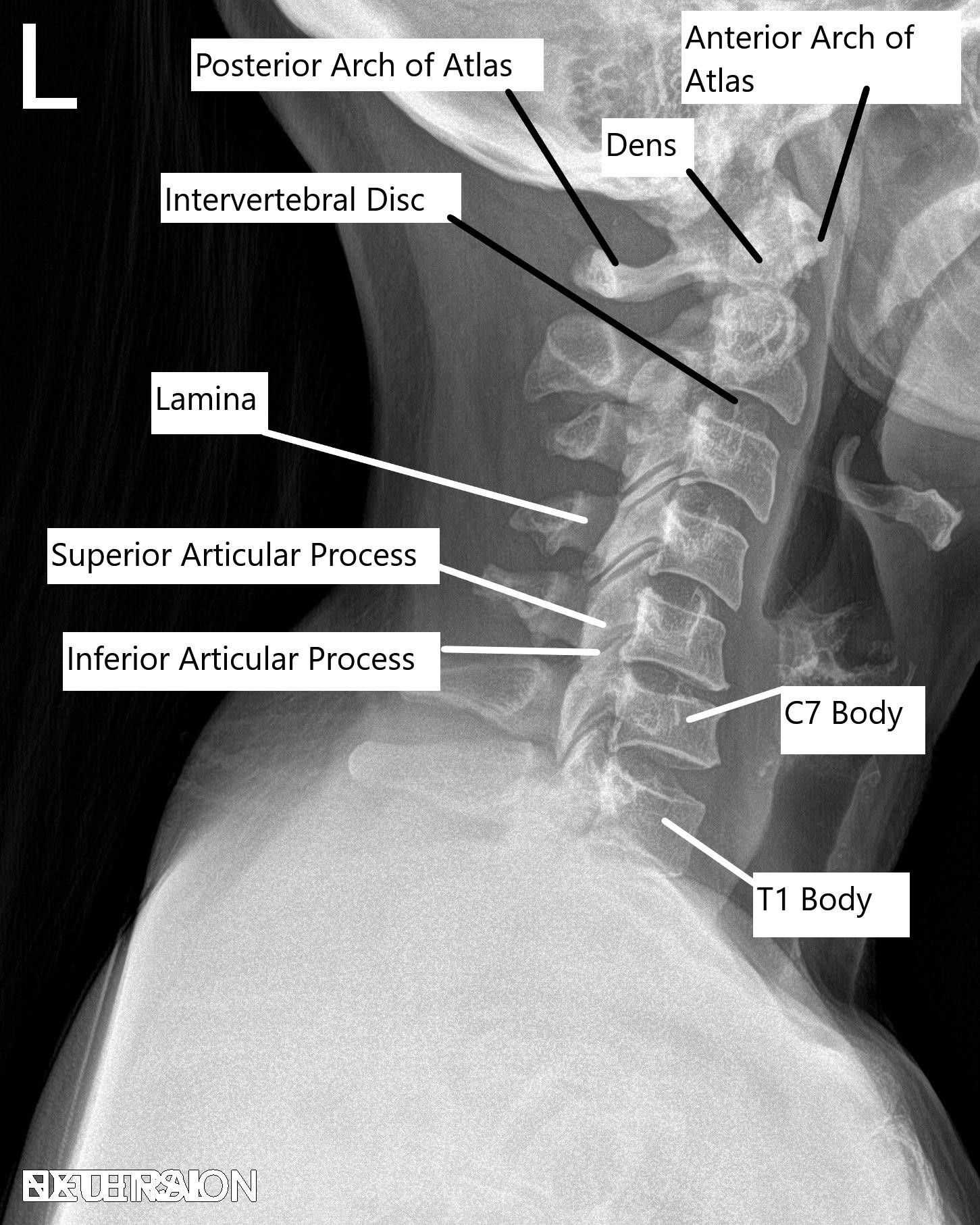
Cervical Spine X-ray in Lateral view.
Posterior Cervical Fusion Indications
The most common and widely used indication for laminectomy and posterior cervical fusion is cervical spondylotic myelopathy (CSM). CSM is defined as arthritic changes on the neck due to the ossification of the ligaments or disc disease, which causes compression of the spinal cord leading to changes in the neurological status of a patient.
CSM usually presents with weakness in the upper extremity only or in all four extremities. It may be associated with tingling and numbness. It may also be associated with gait problems due to imbalance and bowel and bladder issues. Patients with such a presentation may either stay stable or deteriorate.
Patients who deteriorate over time can only be treated by surgical options in an attempt to stop the progression and allow recovery. If the surgery involves multiple levels then surgery from the back is a good option to take care of the disease.
Multilevel compression of the spinal cord due to arthritic changes is the most common indication for this surgery. Patients with a small canal, which can be there since birth is at a higher risk of this disease process. For patients who are deteriorating neurological status, surgery is the only good option to halt the progression and possibly allow recovery of the neurological status.
Posterior Cervical Fusion Procedure
Posterior laminectomy and posterior cervical fusion are done from the back of the neck. It is a major spine surgery, which requires meticulous preparation and skills and instrumentation of the highest quality to carry it out. A thorough discussion with the patient is done before the surgery with regards to expectations and results. All relevant clearances from all the needed specialties as well as the anesthesia team are taken.
The patient is taken to the operating room where general anesthesia is used. A tube is passed into the windpipe to control respiration and breathing. The anesthesia team puts the patient onto multiple monitoring systems. Neurologic monitoring is also used to check the patient’s neurological status during the surgery. The neurological monitoring checks sensory as well as motor functions.
Once everything is in place, the patient is turned onto his belly on the operating table. The head of the patient is usually fixed to the table by the use of tongs (pins). Once a good position is managed, the shoulders are strapped. X-ray in the operating room is used to check the position of the neck as well as the levels.
A straight midline incision is used from the base of the head along the back of the neck. By meticulous dissection and control of bleeding, the bone on the back of the spine is reached and the muscles are separated from the bone. The back part of the vertebrae of the neck is removed meticulously with the use of bur at all the levels required.
Once the bone is removed, the spinal cord is exposed. Further, necessary cleaning up or decompression of the spinal cord is done with the use of precision instruments, this procedure is done at multiple levels as needed.
Now, the screws are planned into the outer part of the vertebral body (lateral mass). The screws are planned at each level, which needs to be fixed so as to prevent the instability from laminectomy and allow fusion. Once the screws are put in place, rods are put to fix the screws on either side to each other.
If the patient has radicular symptoms then a foraminotomy can also be performed at the same time. If there is a deformity then further excision of the facet joints allows the correction of the deformity before the rod fixation. Once the implants are in place and tightened, final pictures are checked with the x-ray.
The facet joints which are of the vertebrae, which are to be fused are decorticated with the use of a bur and bone graft is put over the area of the facets to allow fusion. The central part of the spine and the spinal cord are checked to be thoroughly decompressed. The wound is thoroughly washed and drained. Blood oozings are controlled.
Closure of the wound is done in layers. Vancomycin antibiotic powder is used, which allows the prevention of infection. The skin is closed and the patient is turned onto the back. A collar may be put after the surgery over the dressing. The tube is usually removed by the anesthesia after the surgery. Occasionally, the patient may need to go to ICU with or without the tube for a day for critical monitoring.
Posterior Cervical Fusion Recovery
Recovery from posterior cervical fusion can vary but typically includes:
Hospital Stay: Patients may stay in the hospital for several days post-surgery for monitoring.
Pain Management: Medications are prescribed to manage pain.
Physical Therapy: Rehabilitation exercises help restore movement and strengthen neck muscles.
Lifestyle Modifications: Patients are advised to avoid strenuous activities and follow guidelines to protect their neck during recovery.
Patients after laminectomy and posterior cervical fusion heal gradually over time. These patients may need to go to the rehab depending on their neurological status before and after the surgery. The recovery in the neurological status can take some time. The recovery may not be complete as the recovery of the spinal cord and nerves is unpredictable. The surgery helps in stopping further deterioration of the neurological status, and at the same time optimizing the conditions for the spinal cord to recover as much as it can.
Posterior Cervical Fusion Complications
Laminectomy and posterior cervical surgery is major surgery and has risks and complications. A surgery can lead to further deterioration of neurological status due to injury to the spinal cord and nerve roots. Weakness of muscles of one or both shoulders can happen after surgery. There is a risk of bleeding and need for blood transfusion. There is rare risk of injury to the vertebral artery.
Other risks include dural tear, implant failure, failure of fusion, incomplete recovery, failure of the adjacent segment. Other risks include infection and wound dehiscence, which is more common in surgeries from the back of the neck than the front.
Affordability & Insurance
Planning surgery can feel overwhelming — but understanding your insurance doesn’t have to be. Here’s a simple breakdown to help you feel confident and prepared.
How Medicare Covers Posterior Cervical Fusion
If you have Medicare, your healthcare provider may bill for CPT Code 22600 —this refers to a surgery done from the back to fuse two bones in the lower spine (lumbar region) to help stabilize the spine.
Medicare Coverage Overview
Medicare Part B typically covers 80% of the Medicare-approved amount for this procedure once you’ve met your deductible. That means most of the cost is taken care of — but you may be responsible for the remaining 20% – unless you have secondary insurance.
“What Will It Cost You?”
If you don’t have secondary insurance, here’s what you can expect:
Estimated Out-of-Pocket Cost for Posterior Cervical Fusion (22600): $322.92
Could Additional Procedures Be Needed?
Sometimes, your surgeon may need to perform extra procedures to ensure the best outcome. If that happens, here’s what it could mean for your costs:
- 22614 (Giving added support and stability) You pay $238
For example, Linda needed spine fusion surgery due to back pain. Her surgery included two procedures: joining the first part of her spine (22600) and connecting the second part (22614). Thanks to Medicare, her surgery was covered, and her secondary insurance paid the rest!
A Real-World Example
Imagine your surgery includes all three procedures:
- Connecting two bones in the lower spine→ $322.92
- Added support→ $238
Total Estimated Patient Cost: $560.92
Have AARP or Another Secondary Insurance?
Good news!
If you carry a secondary insurance plan like AARP, it often covers your Medicare coinsurance — which means you may owe nothing out of pocket.
Plans vary, so it’s smart to check with your insurance provider to confirm exactly what they cover.
Injured at Work? Here’s How Workers’ Compensation Helps
If your spine surgery is related to a workplace injury, workers’ compensation insurance usually covers 100% of your medical costs — including your surgery, hospital stay, follow-ups, and rehabilitation.
- No deductibles
- No copays
- No out-of-pocket expenses
As long as your surgery is approved as work-related, your employer’s insurance handles everything so you can focus fully on your recovery.
Hurt in a Car Accident? No-Fault Insurance Protects You
If your cervical surgery is related to a motor vehicle accident, no-fault insurance usually covers all your medical expenses.
It doesn’t matter who was at fault — you’re covered for:
- Surgery costs
- Hospital charges
- Physical therapy
- Follow-up care
- No out-of-pocket costs in most cases.
- Peace of mind while you heal.
Need Help Navigating Insurance?
Insurance can seem complicated, but it doesn’t have to be overwhelming — we’re here to help you every step of the way.
Got questions? Call us today at (631) 981-2663
We’re happy to check your coverage, answer your questions, or even speak directly with your insurance company on your behalf.
Your focus should be on healing — let us handle the rest.
Conclusion
Laminectomy and posterior cervical fusion surgery is done in carefully selected patients can help prevent further deterioration of neurological symptoms as well as help in the recovery of the neurological deficits that have already happened. This surgery has higher risks and complications than the surgery from the front, but in carefully selected patients can be helpful and critical.
Overall, the risks and complications are more from surgery from the back than the front of the neck. For the same reason, surgeries on the front of the neck are preferred, but in patients who have multilevel involvement and compression involved from the back are not good candidates for surgery from the front and need to be treated from the back.
Do you have more questions?
How do I prepare for posterior cervical fusion surgery?
Preparation includes medical evaluations, discontinuing certain medications, arranging post-surgery care, and following specific preoperative instructions from your healthcare team.
What are the alternative treatments to posterior cervical fusion?
Alternatives include physical therapy, medications, steroid injections, and other surgeries like anterior cervical discectomy and fusion (ACDF).
What are the risks of not undergoing the surgery?
Risks include worsening symptoms, increased pain, potential permanent nerve damage, and loss of function.
How long does the posterior cervical fusion surgery take?
The procedure typically lasts 2-4 hours, depending on the complexity and the number of levels being fused.
What are bone grafts, and where do they come from?
Bone grafts are materials promoting bone fusion, sourced from your body (autograft), a donor (allograft), or synthetic alternatives.
Will I have scars after the surgery?
Yes, there will be a scar at the incision site on the back of your neck. Its size and visibility depend on the surgical approach used.
How long will I need to stay in the hospital after surgery?
Most patients stay in the hospital for 2-3 days post-surgery for monitoring and initial recovery.
What should I expect in terms of pain after surgery?
Post-operative pain is common but manageable with medications, typically subsiding significantly within a few weeks.
When can I resume normal activities after the surgery?
Light activities can resume within a few weeks, but strenuous activities should be avoided for 3-6 months.
How will I know if the fusion was successful?
Success is assessed through follow-up appointments, imaging tests, and the resolution of pre-surgery symptoms.
Can the hardware used in the fusion cause problems later?
Rarely, hardware complications such as loosening or breakage can occur, potentially requiring additional surgery.
Will I lose any range of motion in my neck after the surgery?
Some loss of range of motion is expected, especially with multi-level fusions, but most patients adapt well.
Are there long-term restrictions after the surgery?
Long-term restrictions might include avoiding high-impact activities that strain the neck.
What is the success rate of posterior cervical fusion?
Success rates are high, with significant pain relief and improved function reported in over 80-90% of cases.
Can I still experience neck pain after the surgery?
Some patients may experience mild residual neck pain, but it is generally much less severe than before surgery.
What are the most common complications of this surgery?
Common complications include infection, nerve damage, non-union of the vertebrae, and hardware issues.
What are the signs of a post-surgery infection?
Signs of infection include redness, swelling, increased pain at the incision site, drainage or pus, fever, and chills.
How is a non-union treated if the bones don’t fuse properly?
Non-union may require additional surgical intervention to re-stabilize the spine, possibly involving new bone grafts or revised hardware placement.
What can I do to minimize the risk of complications?
To minimize risks, follow all post-operative care instructions, avoid smoking, maintain a healthy diet, and attend all scheduled follow-up appointments.
How often will I need to follow up with my surgeon after the surgery?
Follow-up appointments are typically scheduled at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year post-surgery to monitor progress and address any issues.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
