Cervical Alignment and its Impact on Spinal Health
If neck pain becomes severe and disrupts everyday activities, seeking medical advice is essential. At Complete Orthopedics, our specialized team focuses on treating neck issues with personalized care and surgical options. We aim to understand your symptoms, determine the root causes, and provide appropriate treatments or surgeries.
Our clinics are located throughout New York City and Long Island, partnering with six premier hospitals to deliver excellent neck care. You can book an appointment with our orthopedic specialists online or by phone. Discover the causes and treatments for neck pain and learn when surgery might be necessary.
Overview
The main functions of the cervical spine are to maintain the position of the head in relation to the body and to control the level of horizontal gaze. The sagittal plane’s center of mass of the head is located directly above the occipital condyle, approximately one centimeter anterior and superior to the external auditory canal.
Any deviations from the typical alignment of the head’s mass will cause an increase in cantilever loads, leading to a rise in the amount of energy muscles need to expend. To describe the stability of the cervical spine, literature has divided its bone structure into three primary columns, one anterior and two posterior:
- The vertebral bodies and discs make up the anterior column, while the two posterior columns are made up of the facet joints that articulate with each other.
- The middle column is composed of the posterior half of the vertebral body, the posterior annulus fibrosis, and the posterior longitudinal ligament.
- The ligamentous complex and the posterior arch make up the posterior column.
The head’s weight is supported by the condyle. This weight is then passed to a joint called C1-2 and divided into two parts – anterior column (including a disc between C2 and C3) and posterior column (including joints between C2 and C3).
Most of the weight is carried by the posterior column, which takes up about 64%, while the anterior column carries around 36%. The lumbar spine has been found to bear more weight in the front part (67% to 82%), and less weight in the back part (18% to 33%).
The cervical spine naturally has a curved shape called lordosis, which is created by the wedge-shaped cervical vertebrae and helps to balance out the curve in the thoracic spine called kyphosis. Kyphosis is a natural curve that allows the lungs to expand properly, but it can increase with age.
At the bottom of the lordotic curve, it meets the rigid kyphotic curve in the upper back, which is called the CTJ. Changes in the natural curvature, such as a loss of lordosis or the development of cervical kyphosis, are linked to pain and difficulty moving.
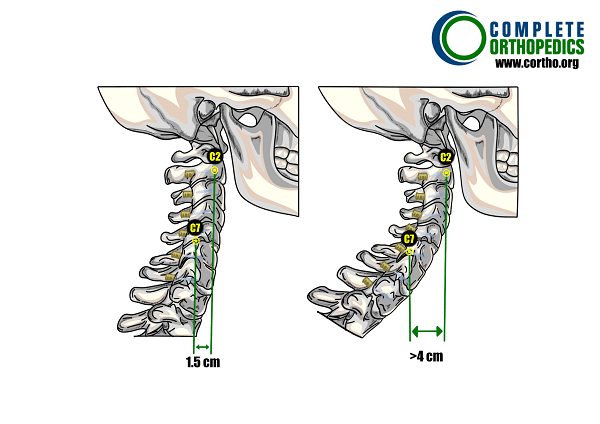
On the left, a normal cervical lordosis is shown with a small distance of 1.5 cm between the C-2 and C-7 plumb lines. On the right, cervical sagittal malalignment is shown with a large distance of more than 4 cm between the C-2 and C-7 plumb lines.
Cervical Lordosis Assessment Methods
There are three main ways to measure cervical lordosis:
- Cobb angle method: It involves drawing two parallel lines – one along the bottom of the second vertebra (C-2) and one from the front of the first vertebra (C-1) to the back of the spinous process – as well as another line parallel to the bottom of the seventh vertebra (C-7). Then, perpendicular lines are drawn from each of the first two lines, and the angle where they meet is the angle of the cervical curvature.
- Jackson physiological stress line method: Two lines are drawn parallel to the posterior surface of the C-7 and C-2 vertebrae. The angle between these two lines is then measured.
- Harrison posterior tangent method: Lines are drawn parallel to the posterior surfaces of each cervical vertebra from C-2 to C-7, and the segmental angles are added together to obtain the overall curvature angle of the neck.
Literature has proposed that the Cobb angle measured from C1 to C7 can give a higher value for cervical lordosis, while the Cobb angle from C2 to C7 may give a lower value.
The Harrison method may provide a more accurate measurement, but it is not widely used due to its complexity. Nevertheless, the Cobb method is still commonly used in clinical settings due to its simplicity and reliability in measuring cervical lordosis.

Determining Cervical Lordosis using three different methods:
- Cobb Angle Method
- Jackson Physiological Stress Line Method
- Harrison Posterior Tangent Method
SVA Measurement
There are various ways to measure the sagittal plane translation of the cervical spine, and one of them is through the use of cervical SVA (Sagittal Vertical Axis). The distance between the C-2 and C-7 plumb lines can be used to measure sagittal alignment globally.
This is done by measuring the C-2 SVA and C-7 SVA, which measure the distance between the posterior superior corner of the sacrum and the C-2 and C-7 plumb lines, respectively. Another way to measure cervical SVA is to use a regional approach, which involves measuring the distance between the posterosuperior aspect of C-7 and a plumb line dropped from the centroid of C-2 or the dens.
A new method to evaluate global sagittal alignment is the gravity line, which is measured from the center of gravity of the head and proposed as an alternative to the C-7 plumb line.
Using a plumb line from the center of gravity of the head, instead of C-2, can also be applied to assess regional cervical SVA. The center of gravity of the head can be estimated on lateral X-rays by using the front part of the external auditory canal as a starting point for the plumb line.
The C-2 plumb line holds significant clinical importance as it has a direct association with Health-Related Quality of Life (HRQOL). An increase in C-2 SVA has been linked to lower HRQOL, making it a crucial factor in assessing the patient’s overall condition.
CBVA Measurement
The CBVA is a measure of the direction of a person’s gaze. It is particularly valuable when dealing with severe, inflexible cervical kyphotic deformities since the inability to maintain a horizontal gaze can significantly affect one’s quality of life and daily activities.
The CBVA is calculated by measuring the angle between a line drawn from the patient’s chin to brow and a vertical line. This angle is determined from clinical photographs of the patient, taken while standing with their hips and knees extended and their neck in a neutral or fixed position.
Relationship Between Thoracic and Neck Tilts with Cervical Alignment
The alignment of the cervical spine has been observed to have a correlation with several factors, including the thoracic inlet angle, neck tilt, cervical tilt, and cranial tilt.
Thoracic inlet angle is determined by measuring the angle between two lines. One line starts from the center of the T-1 endplate and is perpendicular to the T-1 endplate. The other line connects the center of the T-1 endplate to the upper end of the sternum.
Neck tilt is an angle measured between two lines that start from the upper end of the sternum. One line is a vertical line, while the other line connects to the center of the T-1 endplate.
Cervical tilt is determined by measuring the angle between two lines that originate from the center of the T-1 upper endplate. One line is perpendicular to the T-1 endplate, while the other line passes through the tip of the dens.
Cranial tilt is defined as an angle between two lines that originate from the center of the T-1 upper endplate. One line passes through the dens, which is the same as the second line in cervical tilt, while the other line is a vertical line.
There is a correlation between the thoracic inlet angle and the T-1 slope, which is the angle between a horizontal plane and a line that is parallel to the superior endplate of T-1, as well as the neck tilt
Normal Cervical Alignment
Various normal alignment ranges have been described for the cervical spine due to its high mobility. In individuals without any spinal problems, it has been observed that a significant proportion (around 75%-80%) of the normal curvature of the cervical spine when standing is concentrated around the C1-2 level, while there is relatively lesser curvature present in the lower cervical levels. The majority of the lumbar curvature is located at the lower end, with the L5-S1 level having the highest degree of curvature angle.
The curvature of the cervical spine may be influenced by the structure of the cervicothoracic junction (CTJ), which usually includes the C-7 and T-1 vertebrae, the discs between C1 and C7, and the ligaments connecting them. When planning for surgical procedures, it may be necessary to consider the structure of the CTJ as far up as T-2 or T-3.
The CTJ, which encompasses the junction between the cervical and thoracic spine, includes a rigid osseous ring called the thoracic inlet. This bony structure is made up of the first ribs, T-1 vertebra, and upper sternum.
The CTJ refers to the area where the cervical spine, which supports the head, transitions into the thoracic spine, which is relatively rigid due to the presence of the rib cage. In this area, the curvature of the cervical spine changes to the curvature of the thoracic spine, leading to stress on the CTJ, both in static and dynamic states. This stress can have implications for spinal alignment and overall health.
The shape and orientation of the thoracic inlet can affect the position of the cranium and cervical spine in the sagittal plane, which is important for maintaining an upright posture and level gaze. This relationship is similar to the relationship between pelvic incidence and lumbar lordosis.
Different parts of the spine, such as the cervical, thoracic, lumbar, and pelvis regions, are not isolated from each other and there are several important connections or relationships that exist among them.
Pelvic incidence is related to the curvature of the lumbar spine, which is then related to the curvature of the thoracic spine, and finally related to the curvature of the cervical spine. There are correlations between all these spinal regions, indicating that they are not independent of each other.
Therefore, a rise in pelvic incidence is related to a rise in lumbar lordosis, which in turn is associated with an increase in thoracic kyphosis, which further associates with an increase in cervical lordosis.
Cervical lordosis can be considered as an adaptive spinal segment to global alignment, which correlates with lumbar lordosis and thoracic kyphosis. When lumbar lordosis and thoracic kyphosis are adapted to the patient’s pelvic incidence, the amount of cervical lordosis will be proportional to the other curves.
However, an increase in cervical lordosis is a compensatory mechanism when the patient has an anterior malalignment of the spine, whereas if a primary cervical deformity exists, changes in the lumbar spine and pelvis will attempt to compensate.
Cervical Deformity
Cervical spine deformities can occur in both sagittal and coronal planes, but sagittal plane deformities are more prevalent and surgical correction of these deformities is crucial for achieving favorable clinical outcomes.The cervical spine deformity can be classified as either primary or secondary:
- Primary: Often congenital
- Secondary: are caused by iatrogenic factors or ankylosing spondylitis, a condition characterized by the fusion of the joints and ligaments in the spine.
If primary spinal deformities in one area are not treated, they can cause secondary deformities in other regions because the entire spine operates as a single global unit, and the individual regions can strongly impact each other.
Prevalent Deformities
Cervical kyphosis is the most commonly occurring deformity in the cervical spine, and it is often caused by medical treatment, such as postlaminectomy kyphosis. When the spinal cord passes over the deformity, it may get compressed, resulting in various disabling symptoms.
Such as myelopathy, difficulty in looking straight ahead, and difficulty in swallowing. The main objectives of the surgical procedure are to correct and stabilize the deformity, decompress the neural components, and restore the sagittal alignment.
One should acknowledge that while cervical sagittal alignment (cervical SVA) is closely linked to the cervical sagittal Cobb angle (C2-7 Cobb angle), which measures the curvature of the spine, the former also considers the alignment of underlying segments, such as the thoracolumbar spine and pelvis.
Cervical Deformity Surgery
The primary goals of surgery for cervical deformities are to restore the normative alignment of the cervical spine, decompress neural components, and maintain or restore the ability to look straight ahead. In preoperative planning and postoperative evaluation, radiographic parameters such as Cobb angles for kyphosis, C1-2 lordosis, and C2-7 lordosis are commonly used to measure regional changes.
Despite the increasing evidence connecting radiographic parameters and clinical outcomes, most studies are limited by their retrospective design. Furthermore, these studies tend to overlook the potential benefits of spinal cord decompression in the surgical procedures.
Analyzing cervical regional alignment in relation to overall spinal pelvic alignment is crucial to gain a comprehensive understanding of the impact of cervical deformity on patient outcomes.
Cervical Deformity and ASD
The adjacent-segment disease of the cervical spine is defined as the occurrence of new radiculopathy or myelopathy in a motion segment adjacent to a previous arthrodesis of the spine, whether it is superior or inferior.
The correlation between cervical deformity and adjacent segment disease (ASD) has not been studied as extensively as other topics but requires considerable attention.
The cervical spine’s natural lordotic curvature allows it to distribute the load of the head between the posterior and anterior columns. The posterior columns, including the articular processes and facet joints, withstand about 64% of the load, while the anterior column withstands approximately 36%.
Cervical Deformity and Myelopathy
Spinal cord dysfunction due to cervical spondylotic myelopathy is frequently observed in patients aged over 55 years. The most frequent complaints related to cervical spondylotic myelopathy are motor and sensory dysfunction. Often, legs experience these symptoms.
Myelopathy has also been linked to the development of progressive cervical kyphosis, causing the spinal cord to drape over the vertebral bodies and anterior pathology, increasing longitudinal cord tension. The dentate ligaments and cervical nerve roots contribute to this phenomenon by tethering the spinal cord.
When treating cervical myelopathy, it is important to consider the sagittal alignment of the cervical spine, which can impact the approach and the origin and progression of the myelopathy. Merely performing decompression, including ventral decompression, without addressing the cord tension caused by kyphosis, may not lead to the best possible results.
Correcting cervical lordotic alignment in the subaxial spine above C-7 may not always be feasible using only a posterior approach. In some cases, it may be necessary to use an anterior approach and reconstruct the area with lordotic interbody spacers to restore the natural lordotic curve of the cervical spine.
Surgically managing cervical disease is a significant challenge due to the complexity of the cervical spine. To effectively handle complex cervical pathology, it is essential to have knowledge of cervical biomechanics and normative data for cervical alignment.
Conclusion
Cervical spine alignment is a key factor in maintaining spinal health and preventing complications such as myelopathy and ASD. Proper assessment and correction of misalignment can lead to significant improvements in pain, function, and overall quality of life. As research continues, our understanding of cervical alignment and its implications will improve, leading to better diagnostic and treatment strategies for patients with cervical spine issues.
By maintaining awareness of cervical alignment and seeking appropriate medical care when issues arise, individuals can help ensure their spine remains healthy and functional throughout their lives.
Do you have more questions?
What are the common symptoms of cervical spine misalignment?
Common symptoms include neck pain, stiffness, headaches, numbness or tingling in the arms and hands, and reduced range of motion.
What causes cervical spine misalignment?
Causes can include poor posture, trauma or injury, degenerative disc disease, arthritis, and congenital spine abnormalities.
Can cervical spine misalignment affect other parts of the body?
Yes, misalignment can cause referred pain in the shoulders, arms, and even lead to lower back pain due to compensatory changes in posture.
What non-surgical treatments are available for cervical spine misalignment?
Non-surgical treatments include physical therapy, chiropractic care, pain management with medications, and lifestyle modifications such as ergonomic adjustments.
When is surgery necessary for cervical spine misalignment?
Surgery may be necessary when there is severe pain, neurological deficits, spinal cord compression, or when conservative treatments have failed.
How can I prevent cervical spine misalignment?
Prevention strategies include maintaining good posture, using ergonomic furniture, regular exercise, and avoiding activities that strain the neck.
Can poor sleep habits contribute to cervical spine misalignment?
Yes, using inadequate pillows or sleeping in positions that strain the neck can contribute to misalignment.
How does cervical spine alignment affect athletic performance?
Proper alignment can enhance athletic performance by improving balance, coordination, and reducing the risk of injury.
What is cervical lordosis, and why is it important?
Cervical lordosis is the natural inward curvature of the cervical spine. It is important for absorbing shock and maintaining balance and alignment.
Can cervical spine misalignment cause headaches?
Yes, tension headaches and migraines can be caused or exacerbated by cervical spine misalignment due to muscle tension and nerve irritation.
Is cervical spine alignment related to overall spinal health?
Yes, proper cervical alignment supports the overall alignment and function of the entire spine, preventing compensatory issues and maintaining spinal health.
Are there specific exercises to improve cervical spine alignment?
Yes, exercises such as neck stretches, chin tucks, and strengthening exercises for the neck and upper back can help improve alignment.
How long does recovery take after cervical spine surgery?
Recovery time varies but typically ranges from several weeks to a few months, depending on the type and extent of the surgery.
Can cervical spine misalignment recur after treatment?
Yes, misalignment can recur, especially if underlying issues like poor posture or degenerative conditions are not addressed.
What are the risks of not treating cervical spine misalignment?
Untreated misalignment can lead to chronic pain, reduced mobility, neurological deficits, and progressive spinal deformities.
How does cervical spine alignment affect breathing and circulation?
Severe misalignment can impact breathing and circulation by affecting the muscles and nerves involved in these functions.
Are there specific postural habits to avoid to maintain cervical spine alignment?
Avoid slouching, forward head posture, and prolonged periods of looking down at electronic devices.
Can cervical spine misalignment affect mental health?
Yes, chronic pain and discomfort from misalignment can contribute to anxiety, depression, and decreased quality of life.
Is cervical spine alignment important for children as well?
Yes, proper alignment is crucial during growth and development to prevent future spinal issues.
Can wearing a neck brace help with cervical spine alignment?
A neck brace can provide temporary support and relief but should not be relied upon long-term without addressing the underlying cause.
How often should someone get their cervical spine alignment checked?
Regular check-ups are recommended, especially if experiencing symptoms. Frequency can vary based on individual risk factors and medical history.
Are there any dietary supplements that support spinal health?
Supplements such as calcium, vitamin D, and omega-3 fatty acids can support bone and joint health, which are important for maintaining spinal alignment. Always consult with a healthcare provider before starting any new supplement regimen.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
